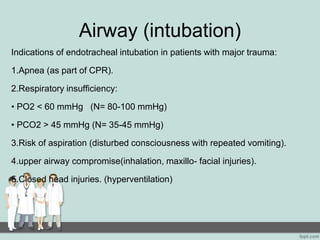
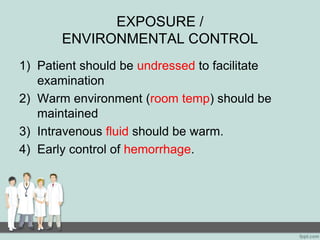
Polytrauma refers to injuries to two or more organ systems that are life threatening. It is a leading cause of death worldwide, especially among younger people. A polytrauma patient may have injuries to their head, chest, abdomen, pelvis or multiple long bone fractures. Immediate goals in treatment are to save the patient's life, limb, joint and restore function. Advanced Trauma Life Support (ATLS) protocols emphasize treating lethal threats like airway issues, bleeding and brain injuries first before fully assessing other injuries. The primary survey examines a patient's airway, breathing, circulation, disability and exposure to quickly identify and address life-threatening problems.