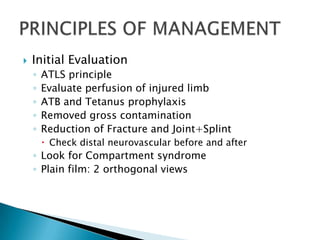
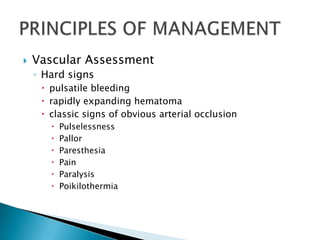
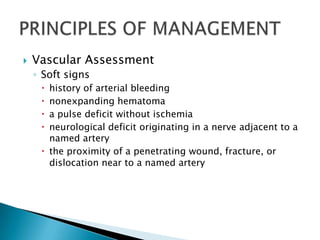
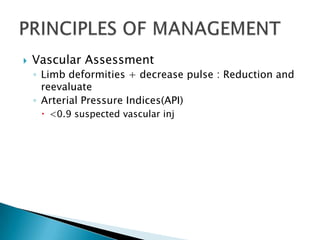
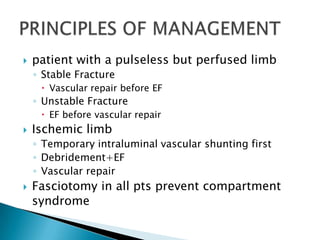
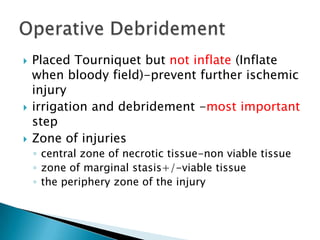
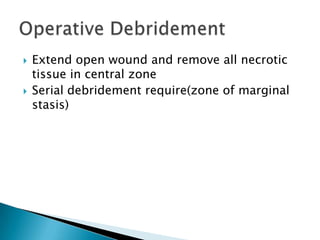
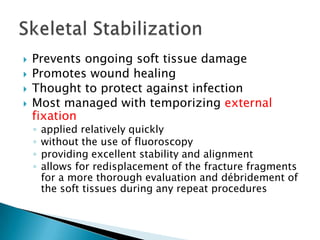
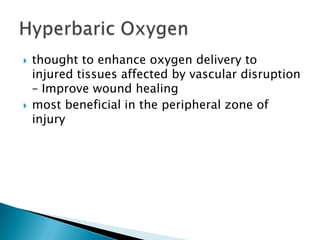
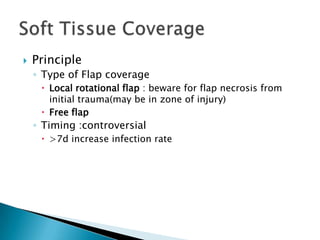
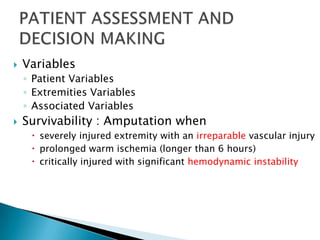
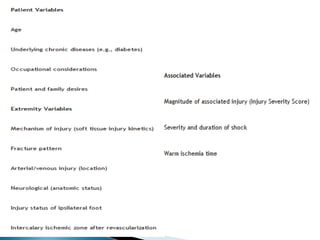
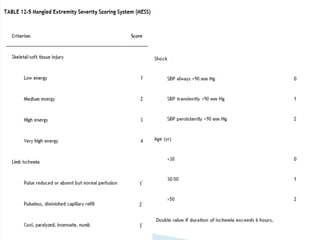
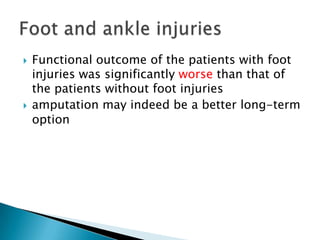
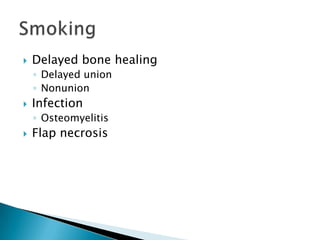
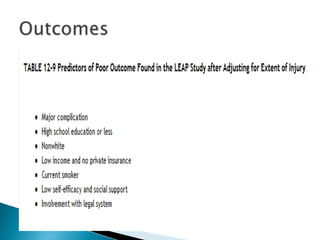
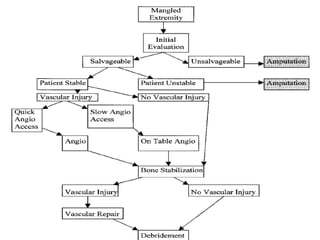
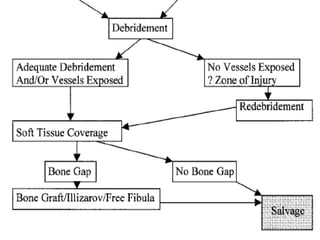
This document discusses the management of mangled extremity injuries. It covers the initial evaluation, assessment of vascular injury, principles of debridement and wound management, considerations for flap coverage vs amputation, and factors that influence functional outcomes. Scoring systems can help guide the decision between amputation and limb salvage, though the final decision requires clinical judgment based on each patient's situation. Complications like infection, non-union, and flap necrosis may still occur despite salvage attempts.