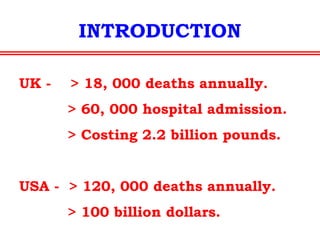
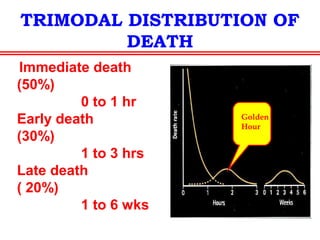
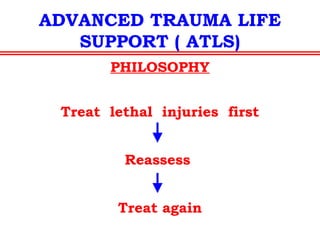
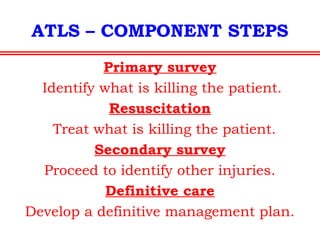
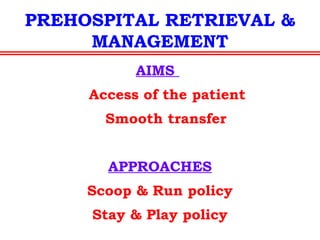
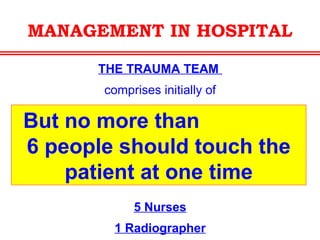
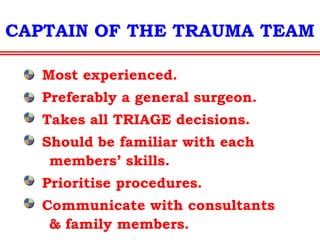
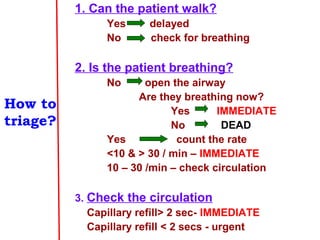
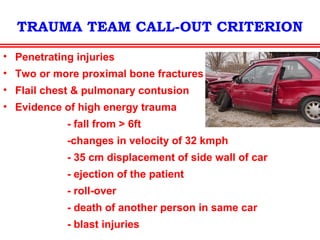
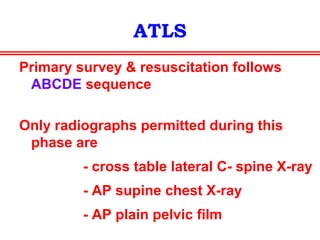
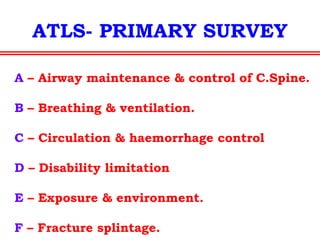
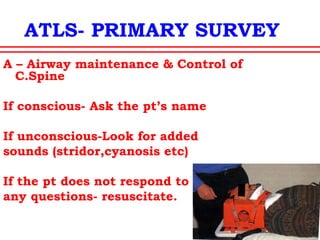
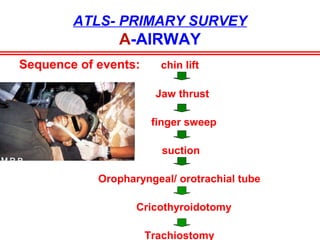
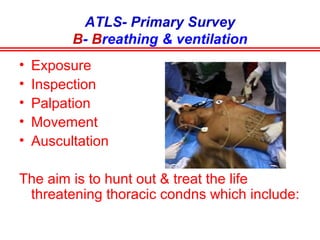
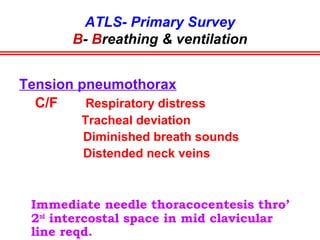
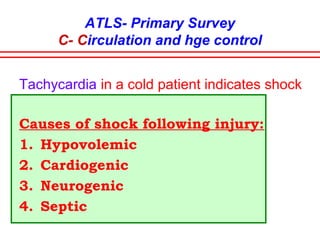
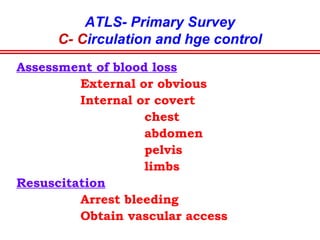
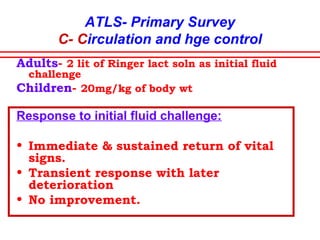
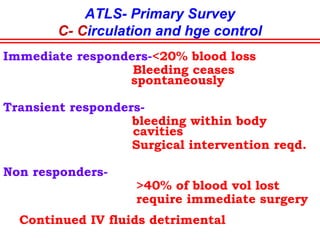
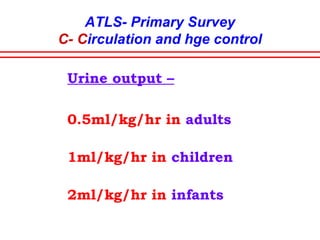
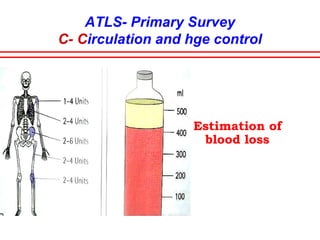
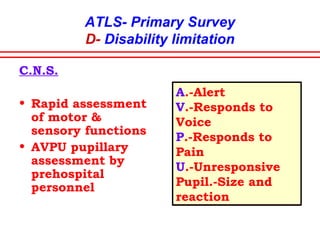
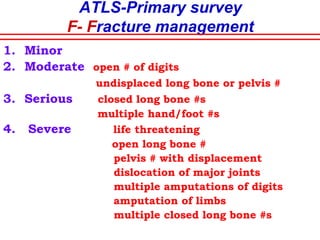
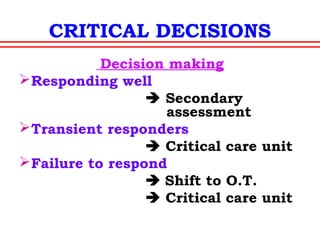
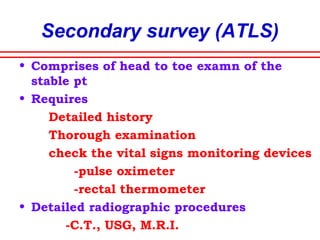
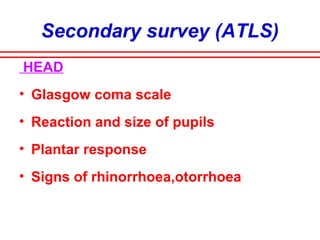
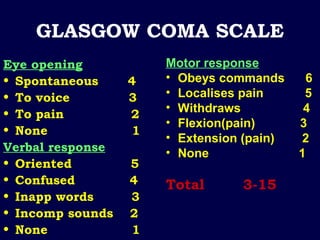
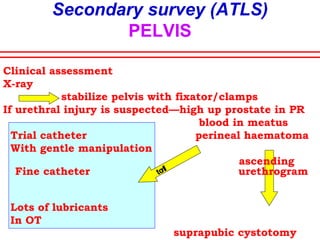
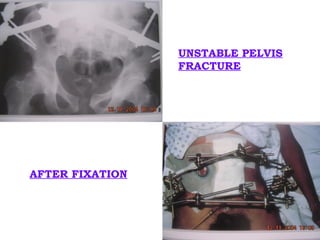
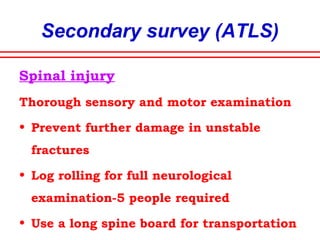
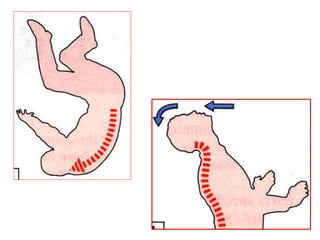
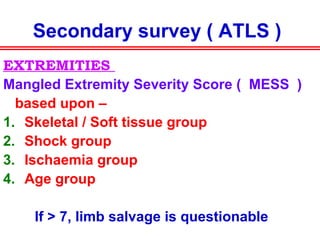
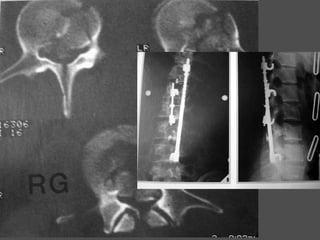
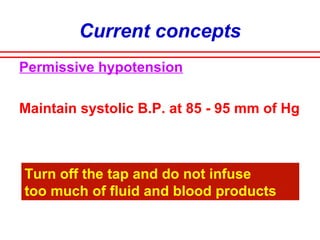
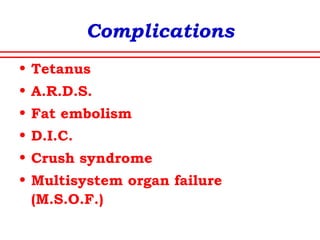
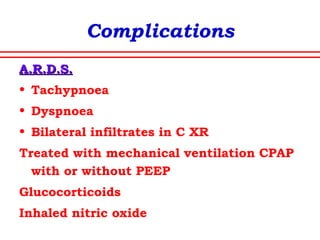
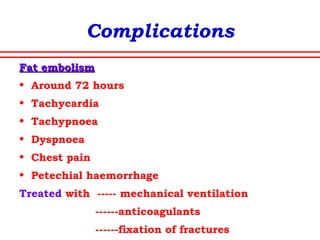
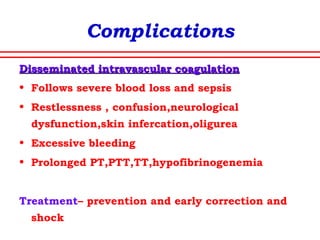
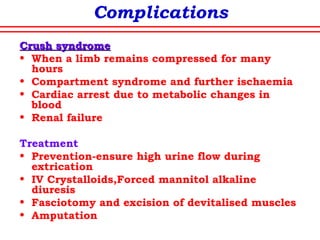
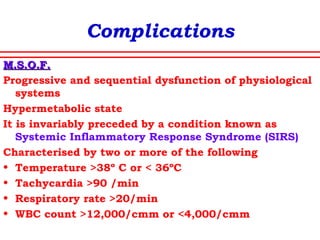
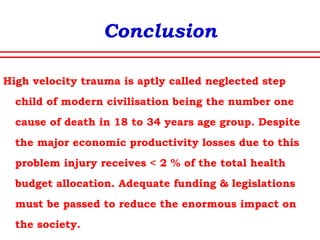
The document discusses polytrauma and its management, highlighting its significant impact on mortality and healthcare costs in both the UK and USA. It covers injury mechanisms, triage procedures, and the Advanced Trauma Life Support (ATLS) protocol, emphasizing the importance of swift intervention and management by a specialized trauma team. Additionally, it addresses complications arising from trauma, the need for a multi-specialty approach in treatment, and the necessity for improved funding and legislation to tackle high-velocity trauma effectively.