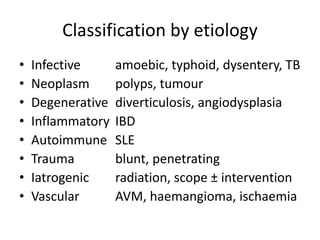
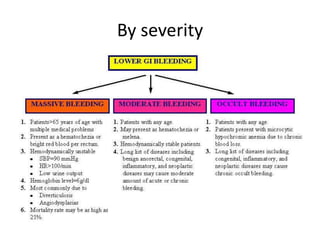
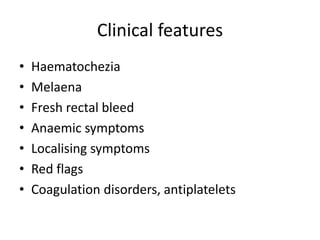
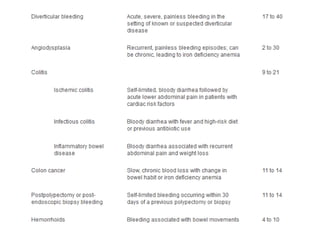
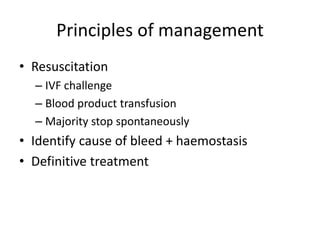
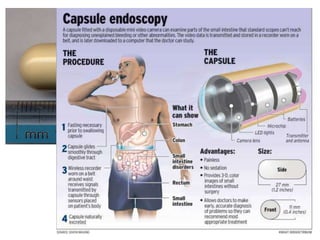
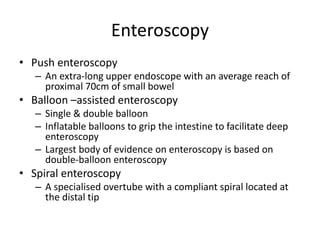
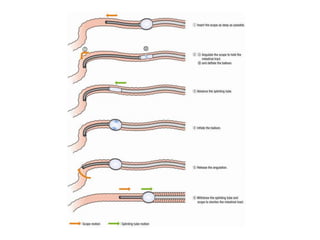
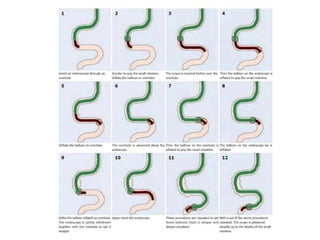
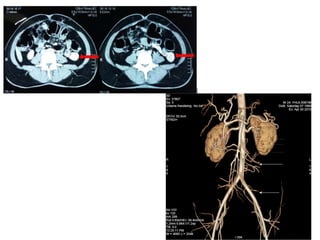
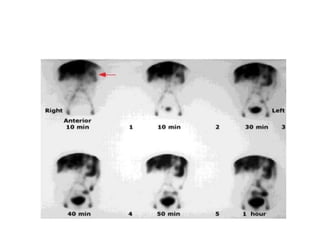
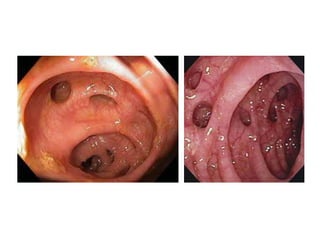
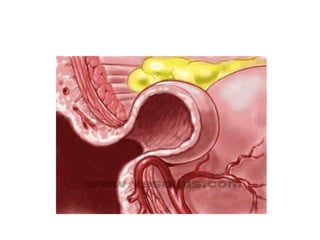
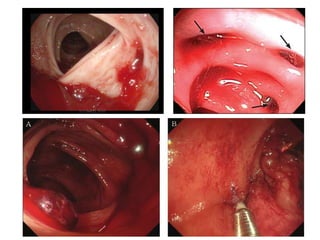
The document discusses lower gastrointestinal (GI) bleeding, focusing on its causes, clinical features, and management principles. It emphasizes diverticular bleeding as the most common cause, with potential complications and recurrence rates, and outlines various diagnostic and treatment approaches including endoscopy, imaging, and surgical interventions. Key management strategies involve resuscitation, identifying the cause of bleeding, and implementing definitive treatment based on the patient's condition.