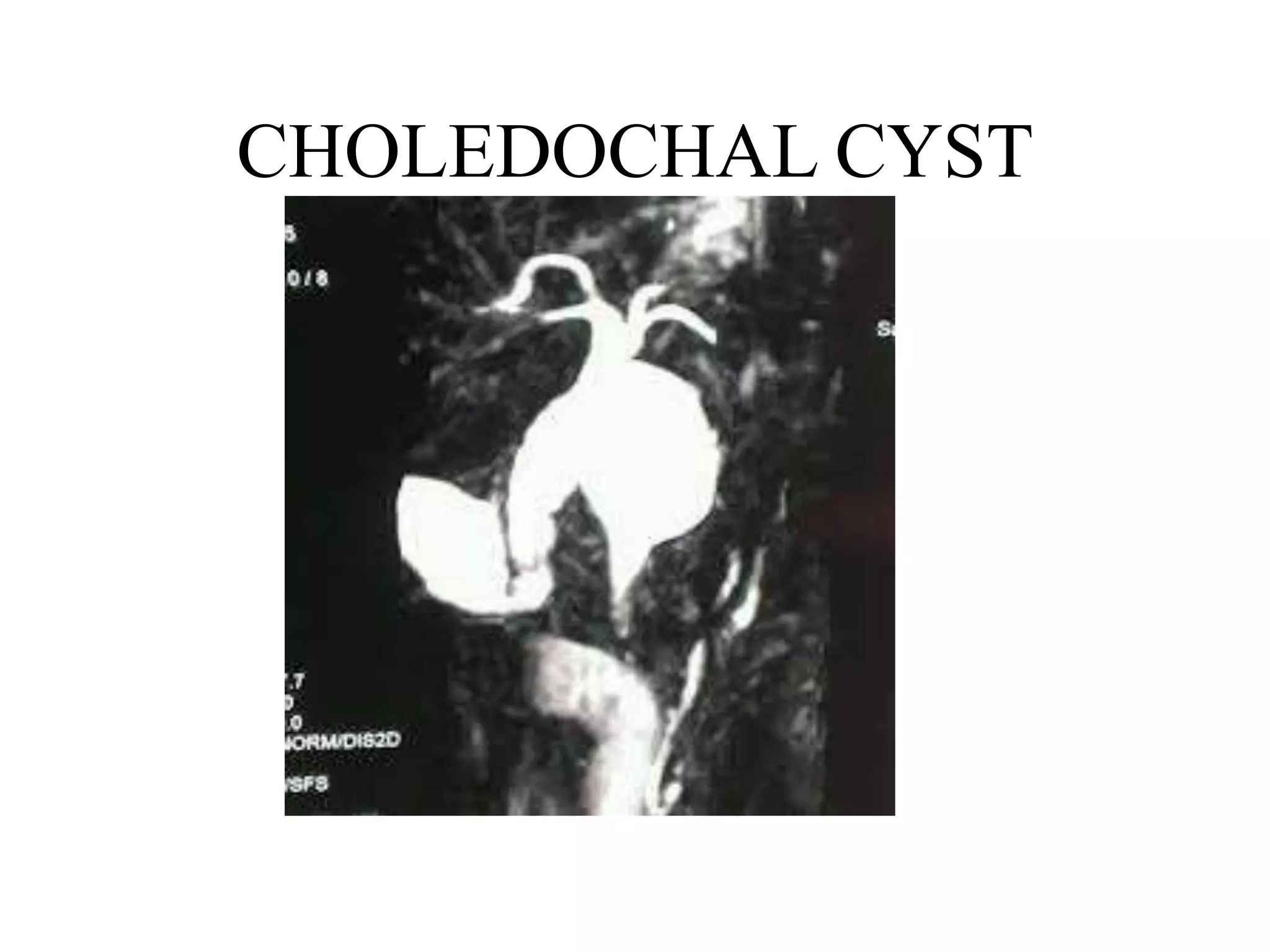
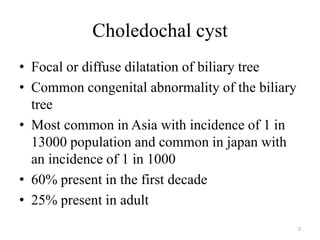
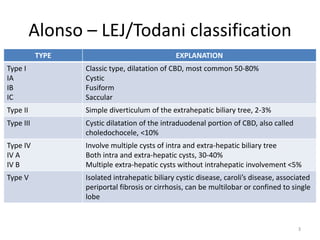
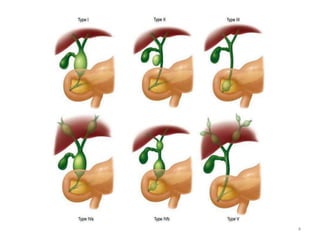
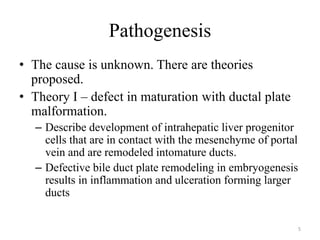
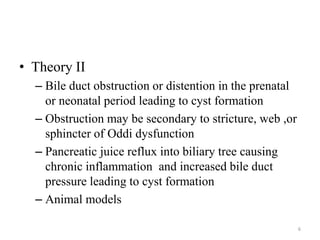
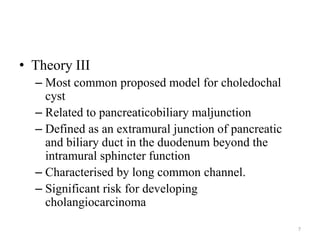
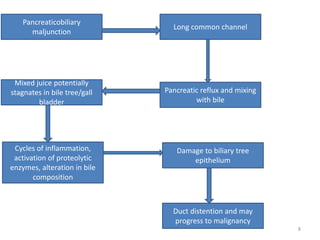
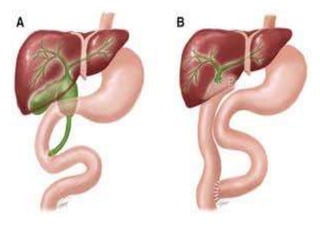
Choledochal cyst is a congenital abnormality of the biliary tree that results in dilatation of the bile ducts. It is most common in Asia, with various theories proposed for its pathogenesis including abnormalities in bile duct remodeling during embryogenesis or obstruction leading to cyst formation. Patients may present with jaundice, abdominal pain or a mass. Diagnosis is typically made using ultrasound, CT or MRCP imaging. Surgical excision of the cyst and biliary reconstruction is the primary treatment for types I-IV, while type III may be treated endoscopically and type V depends on extent of liver involvement.