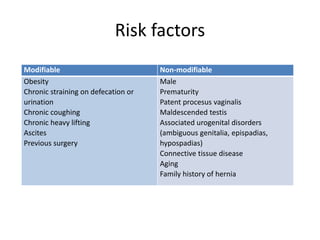
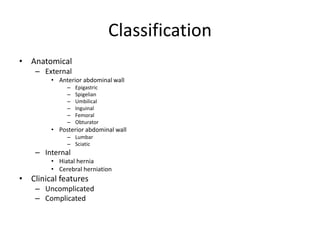
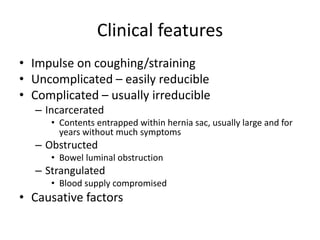
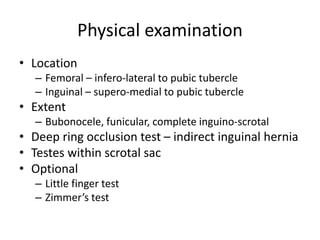
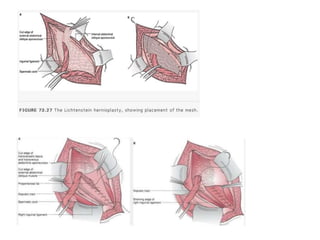
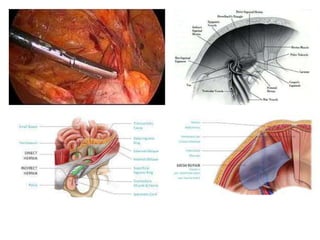
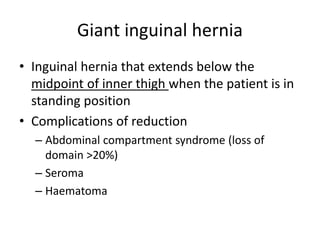
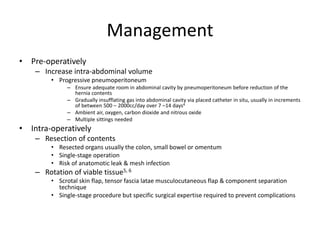
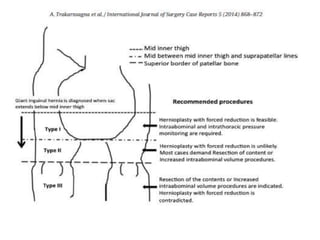
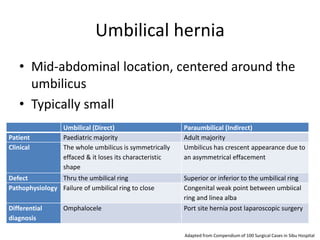
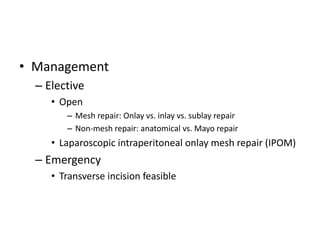
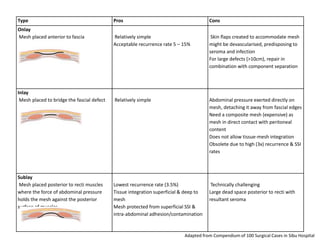
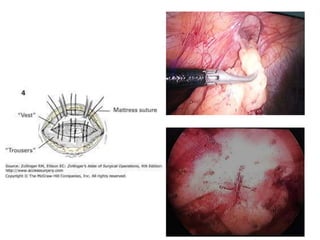
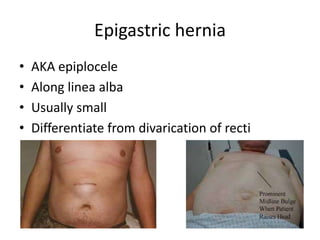
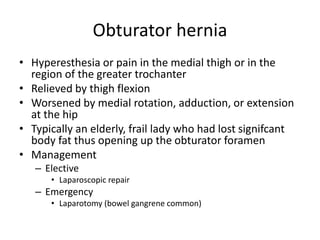
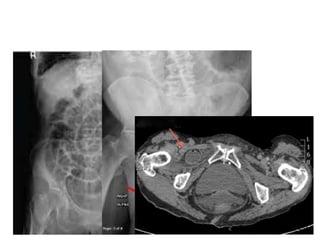
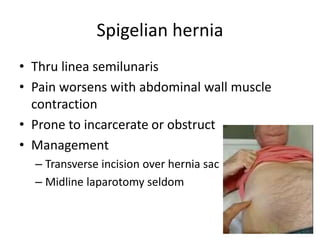
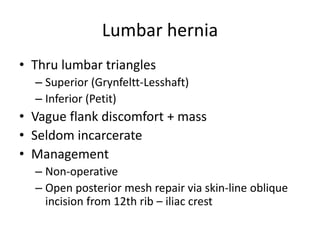
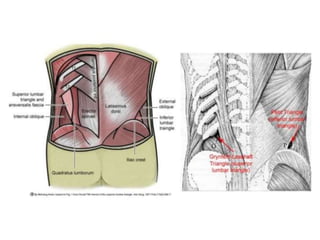
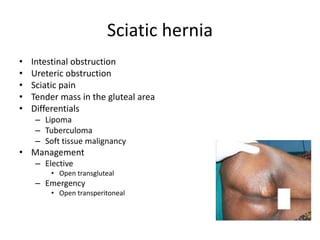
The document defines hernia as a protrusion of an organ through the body wall that contains it, discusses the most common types of hernias including their risk factors, classifications, clinical features, and management through both non-operative and operative approaches such as open and laparoscopic repair. Specific hernia configurations and other rare types are also reviewed, with comparisons in characteristics and treatments.