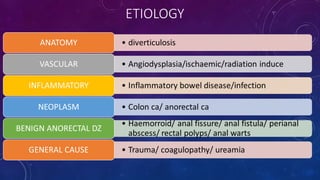
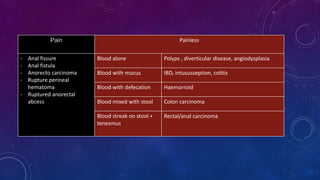
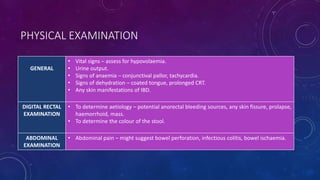
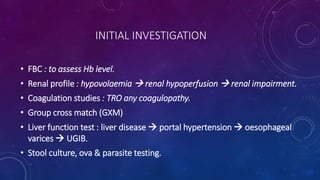
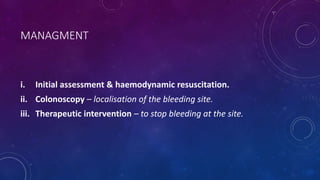
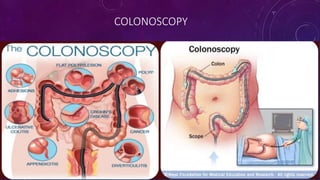
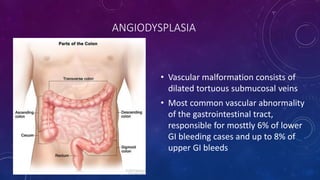
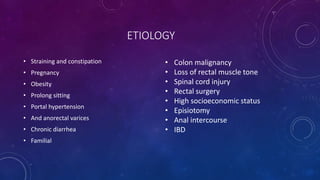
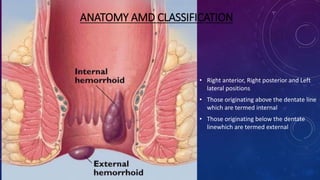
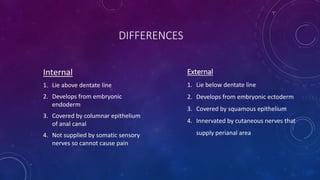
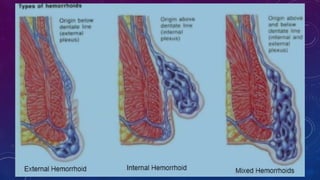
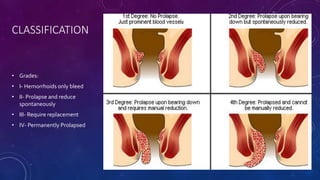
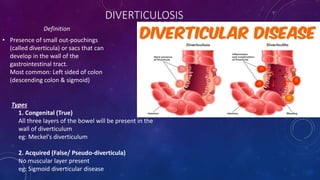
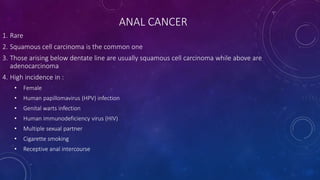
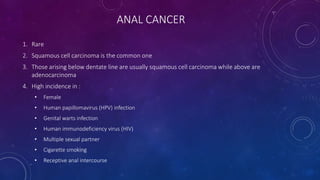
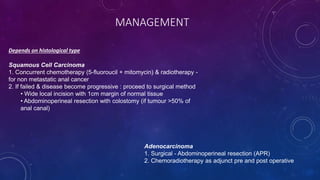
Lower gastrointestinal bleeding (LGIB) refers to blood loss originating from a site distal to the ligament of Treitz. Common causes of LGIB include hemorrhoids, diverticulosis, angiodysplasia, and anal cancers. Hematochezia is the typical presentation of LGIB. Initial workup includes examination, blood tests to check for anemia and coagulopathy, and colonoscopy for diagnosis and potential therapeutic intervention to stop bleeding. Management depends on the cause but may include conservative measures, nonsurgical options like banding or surgical procedures like hemorrhoidectomy.