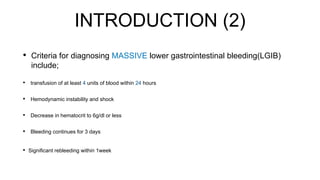
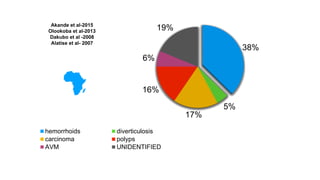
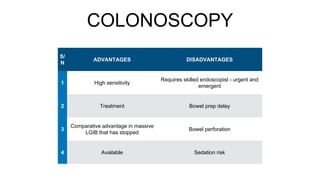
Massive lower gastrointestinal bleeding is a life-threatening condition defined by transfusing at least 4 units of blood in 24 hours, hemodynamic instability, or a hematocrit of less than 6g/dl. The main causes are diverticulosis (60%), unknown (13%), hemorrhoids (11%), and neoplasia (9%). Management involves resuscitation, risk assessment, blood transfusions, endoscopy for diagnosis and treatment, and angiography for patients with ongoing bleeding or when endoscopy fails to identify the source. Colonoscopy has high sensitivity but requires bowel preparation, while angiography can localize active bleeding but the patient must be stable. Endoscopic treatments include clips, thermal coagulation, and injections.