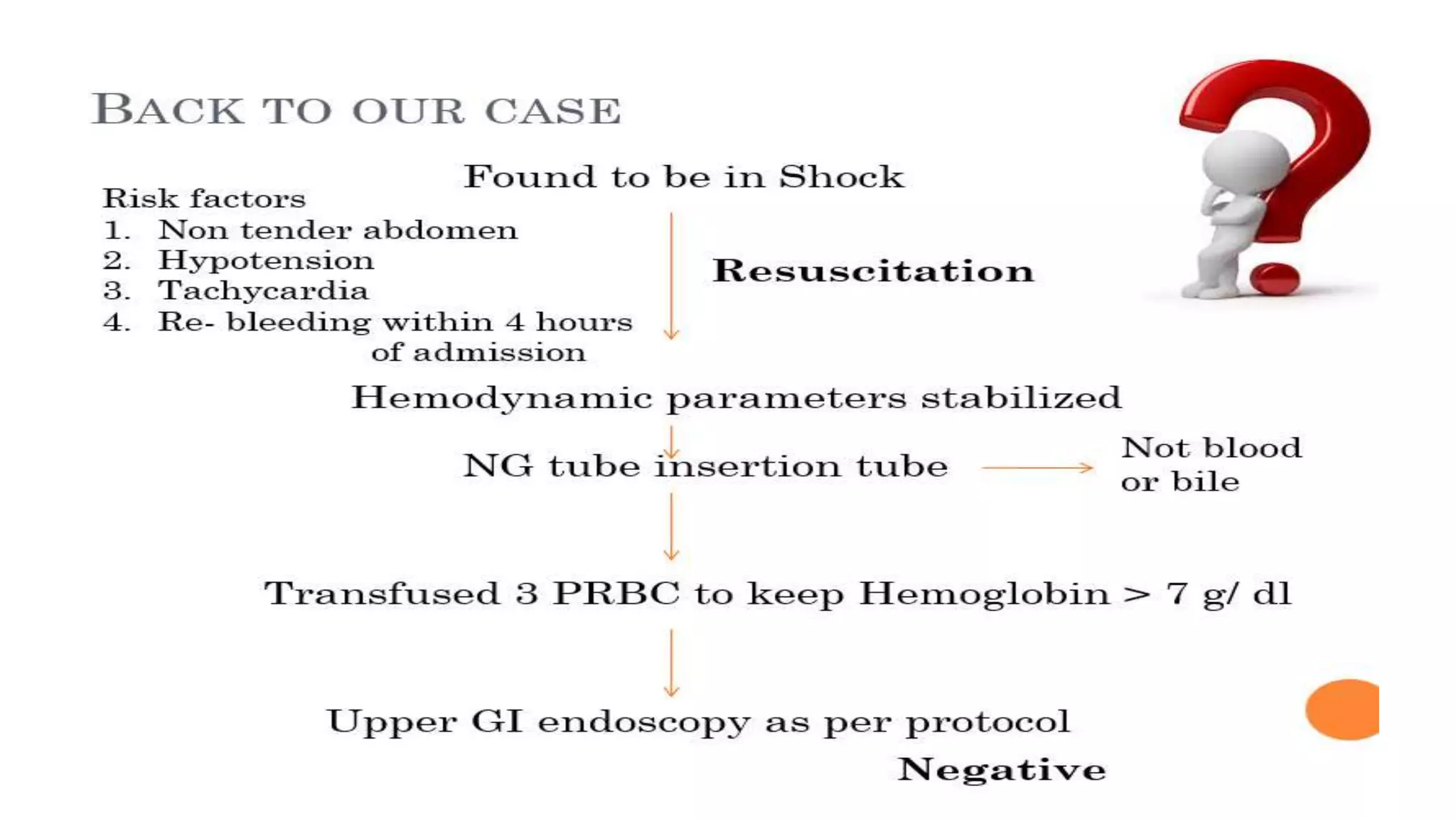
This document provides an overview of lower gastrointestinal bleeding (LGIB), including its definition, etiology, clinical features, diagnostic and therapeutic approaches. It discusses how LGIB accounts for 20% of gastrointestinal bleeding cases and can be safely managed in an outpatient setting once initial resuscitation and risk evaluation is complete. Colonoscopy is highlighted as the first-line investigation, while angiography and surgery are reserved for more severe or refractory cases. The overall mortality rate of LGIB is reported to be less than 5%.