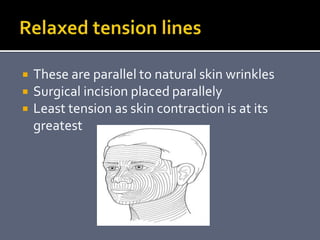
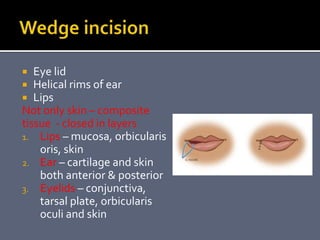
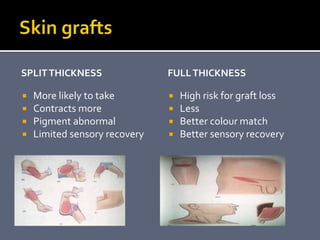
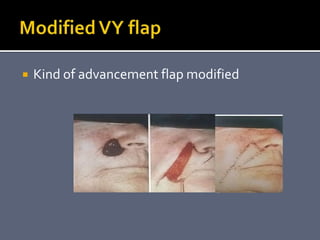
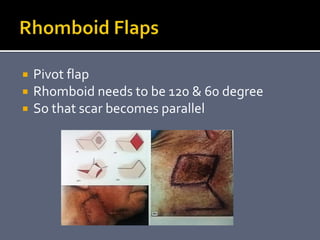
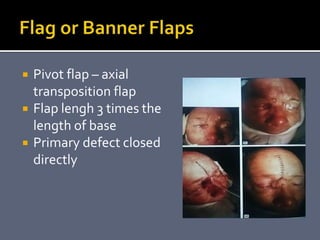
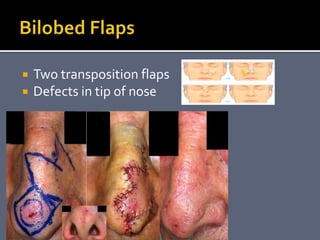
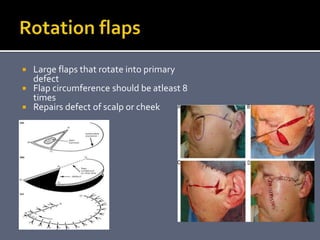
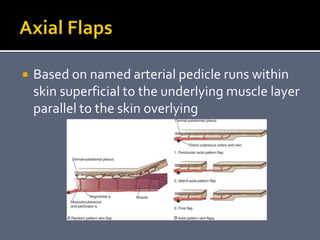
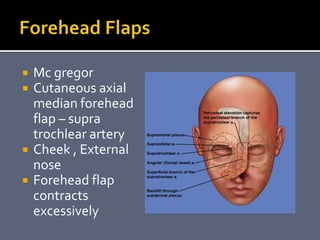
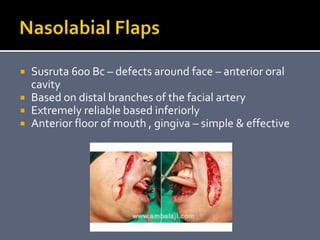
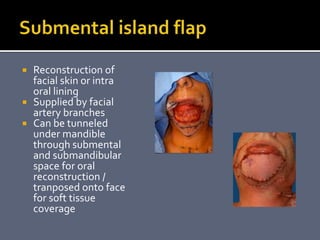
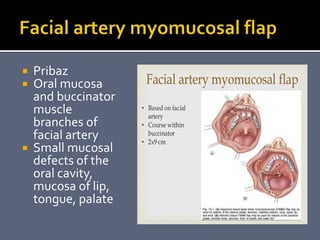
This document discusses various techniques for reconstructing skin and soft tissue defects in the head and neck region. It describes different types of grafts, local flaps, regional flaps, and free flaps that can be used including split thickness grafts, full thickness grafts, axial pattern flaps, transposition flaps, pedicled flaps like pectoralis major and latissimus dorsi flaps. Careful preoperative planning is important when using local flaps for head and neck reconstruction.