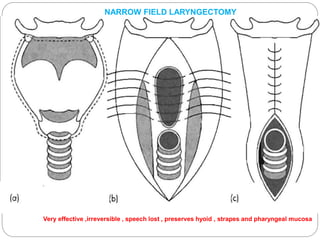
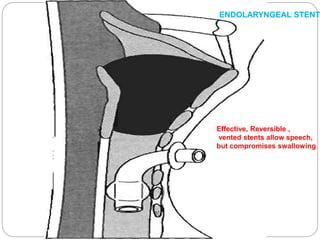
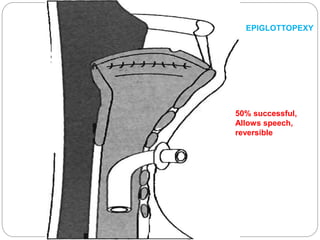
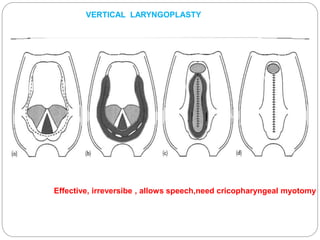
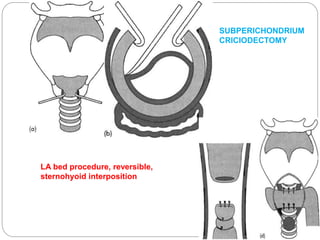
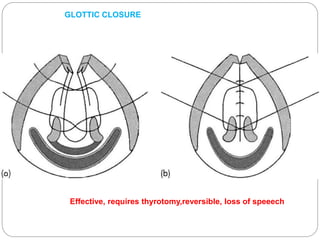
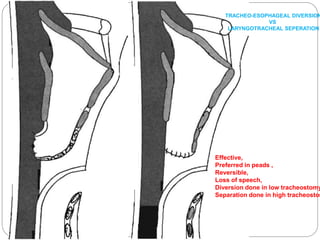
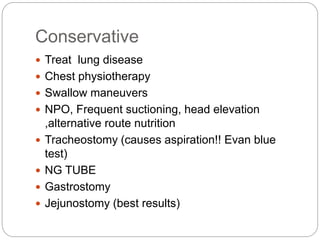
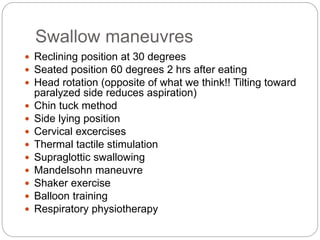
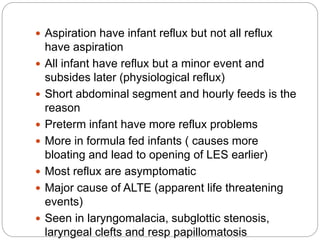
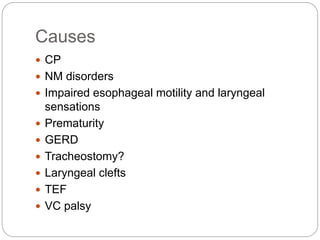
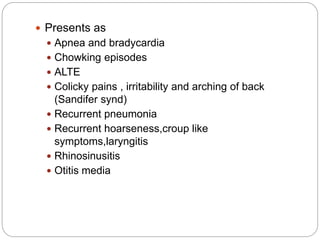
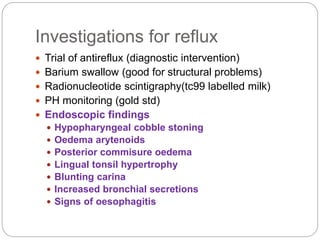
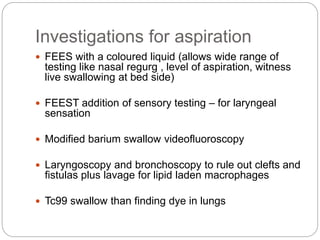
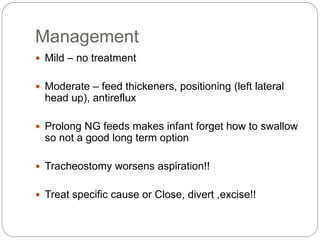
The document outlines the definition, causes, symptoms, examinations, and management of intractable aspiration, emphasizing laryngeal penetration of gastric secretions. It discusses various conditions leading to aspiration, diagnostic methods, and treatment options, including conservative strategies and surgical interventions. Additionally, it addresses specific concerns regarding aspiration in neonates and related investigations.