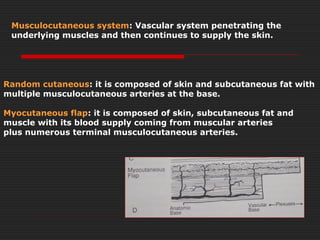
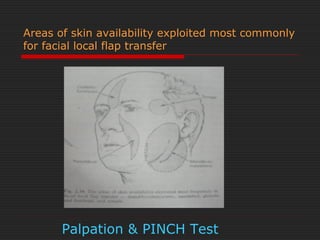
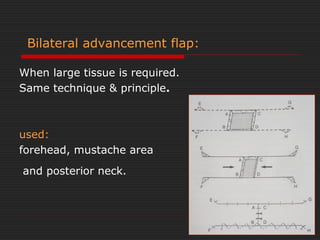
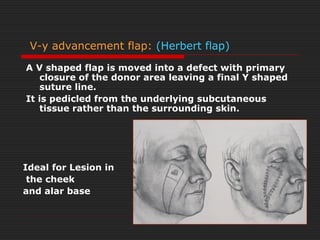
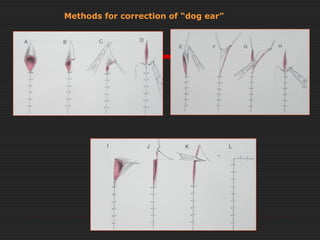
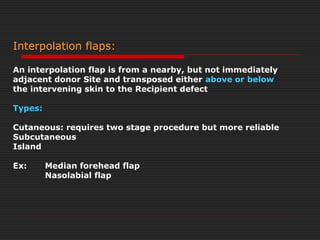
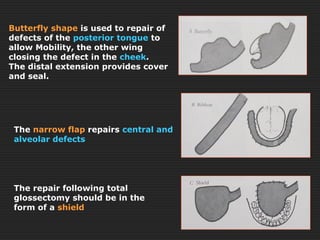
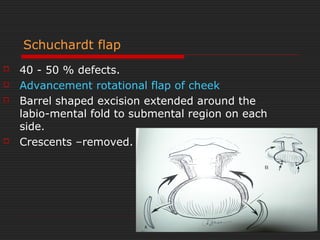
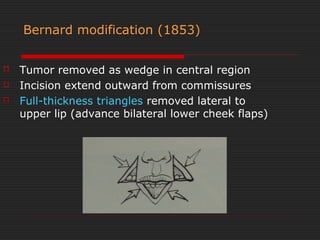
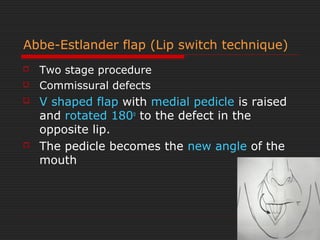
Local flaps involve moving tissue from one area to another to repair wounds and defects. There are various types of local flaps classified by their movement (advancement, pivot, transposition), blood supply (axial, random), and composition (skin, muscle, etc.). Common local flaps used in facial reconstruction include advancement flaps, rotation flaps, transposition flaps, and interpolation flaps which are taken from nearby donor sites. The document provides detailed descriptions of various local flap techniques for reconstructing different areas of the face like the lips, nose, and cheeks.