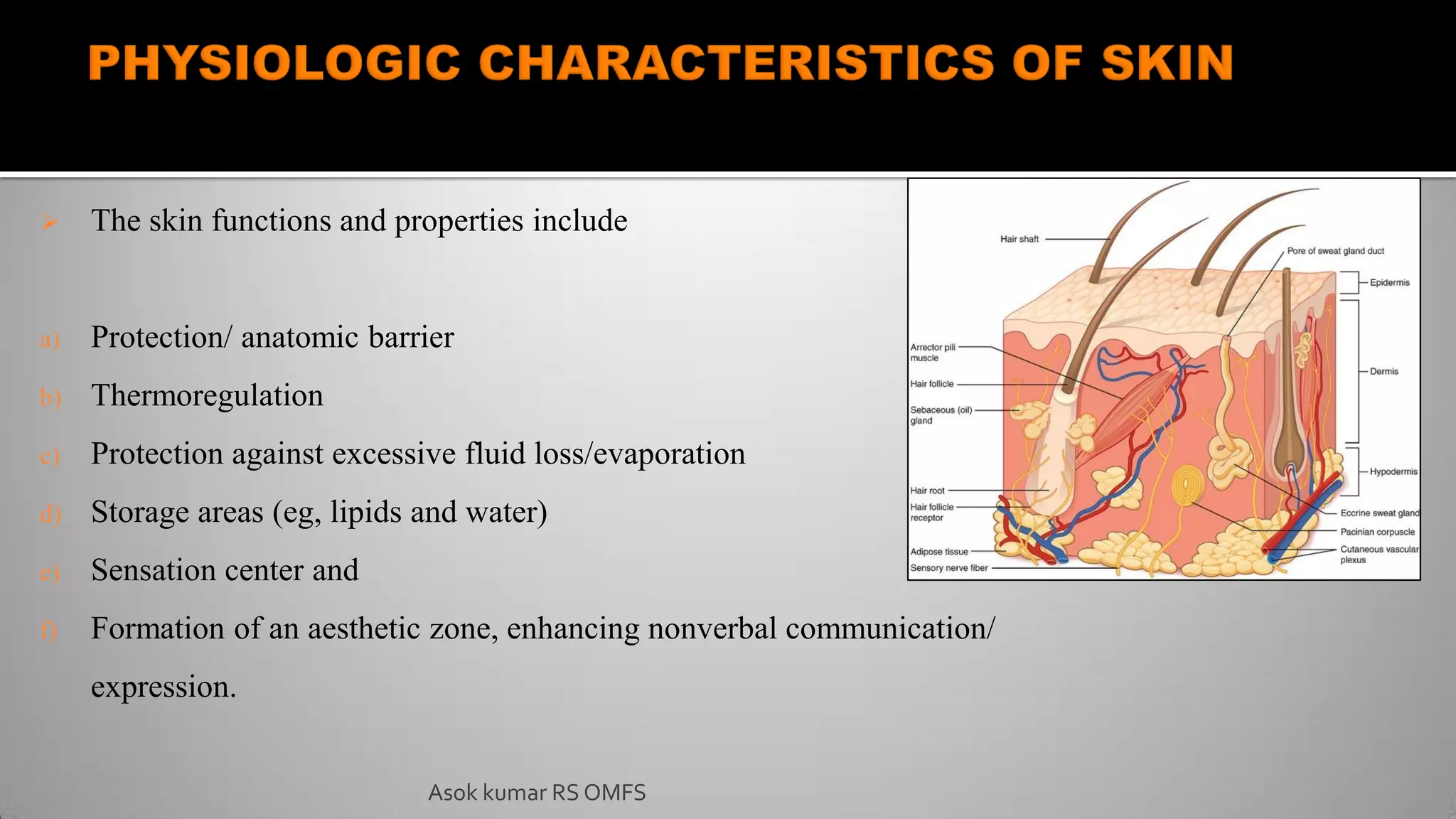
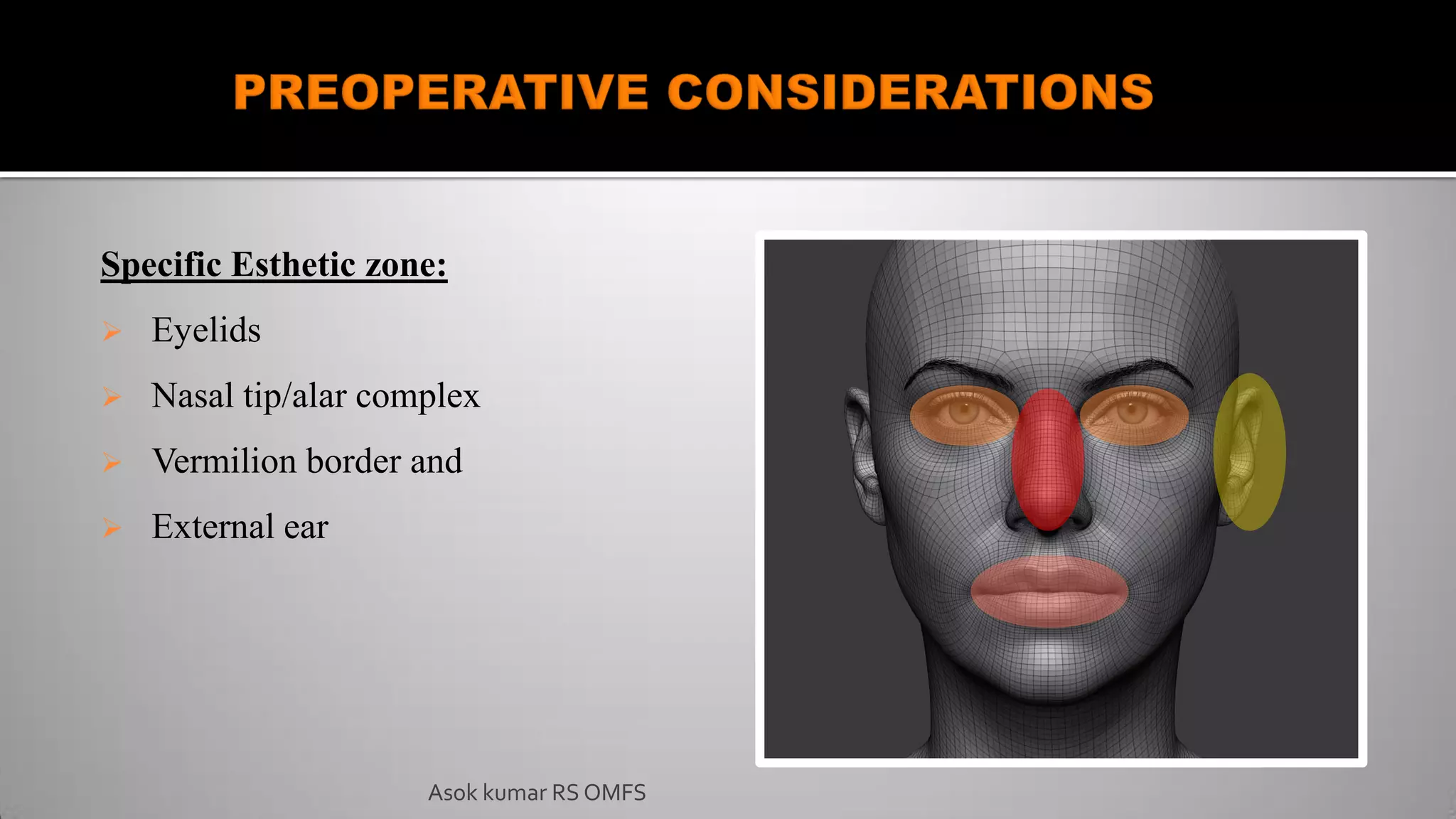
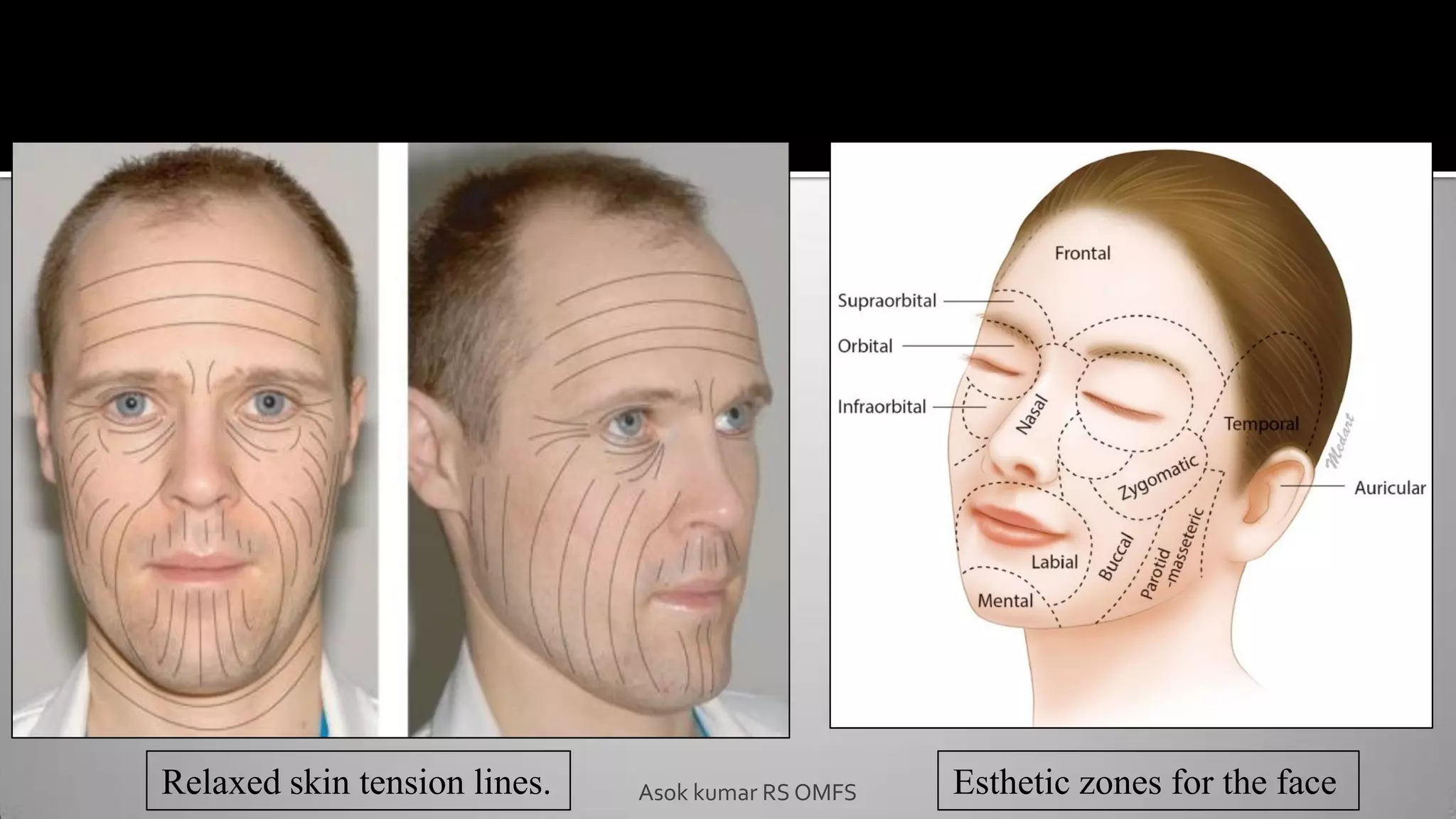
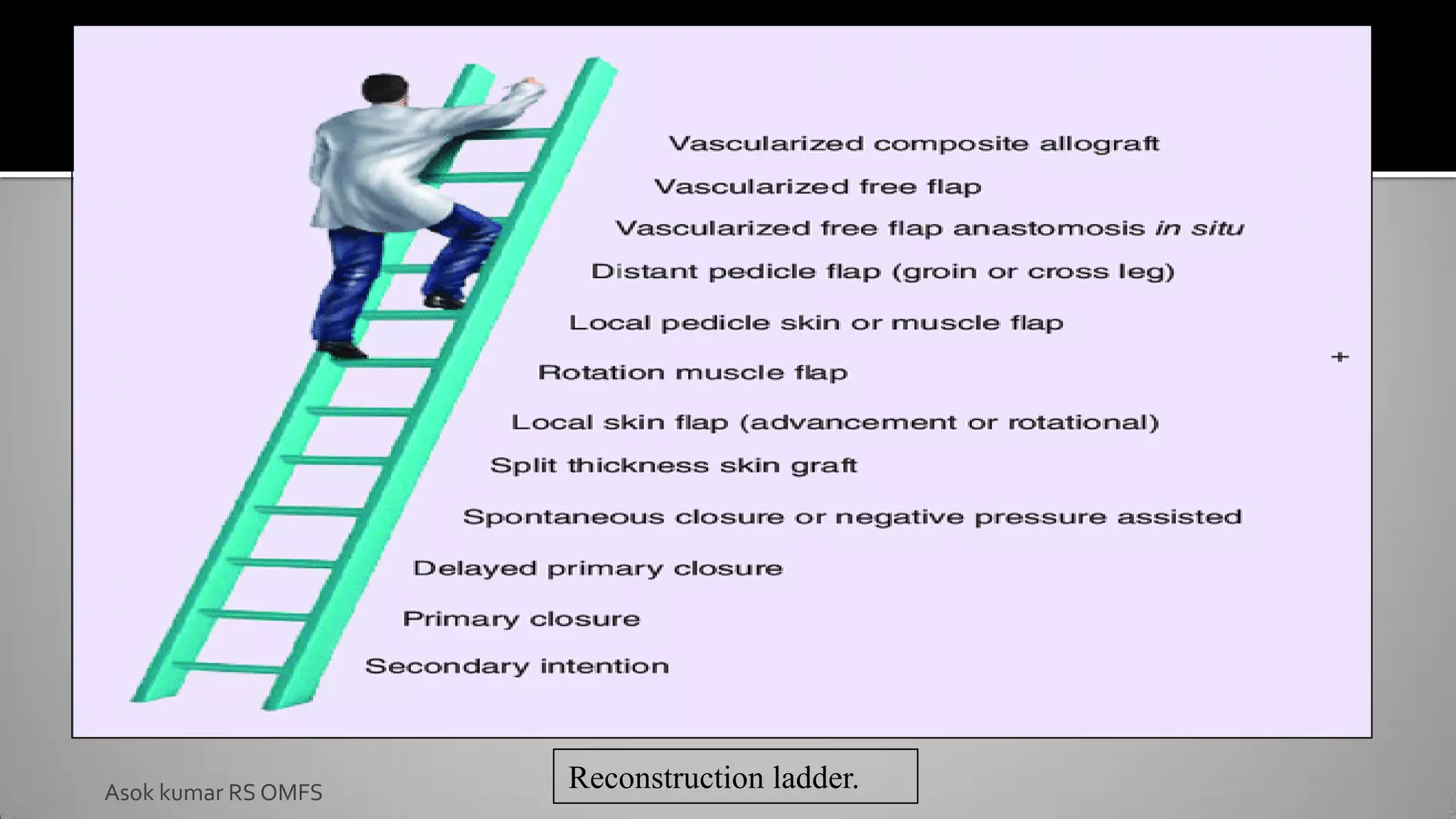
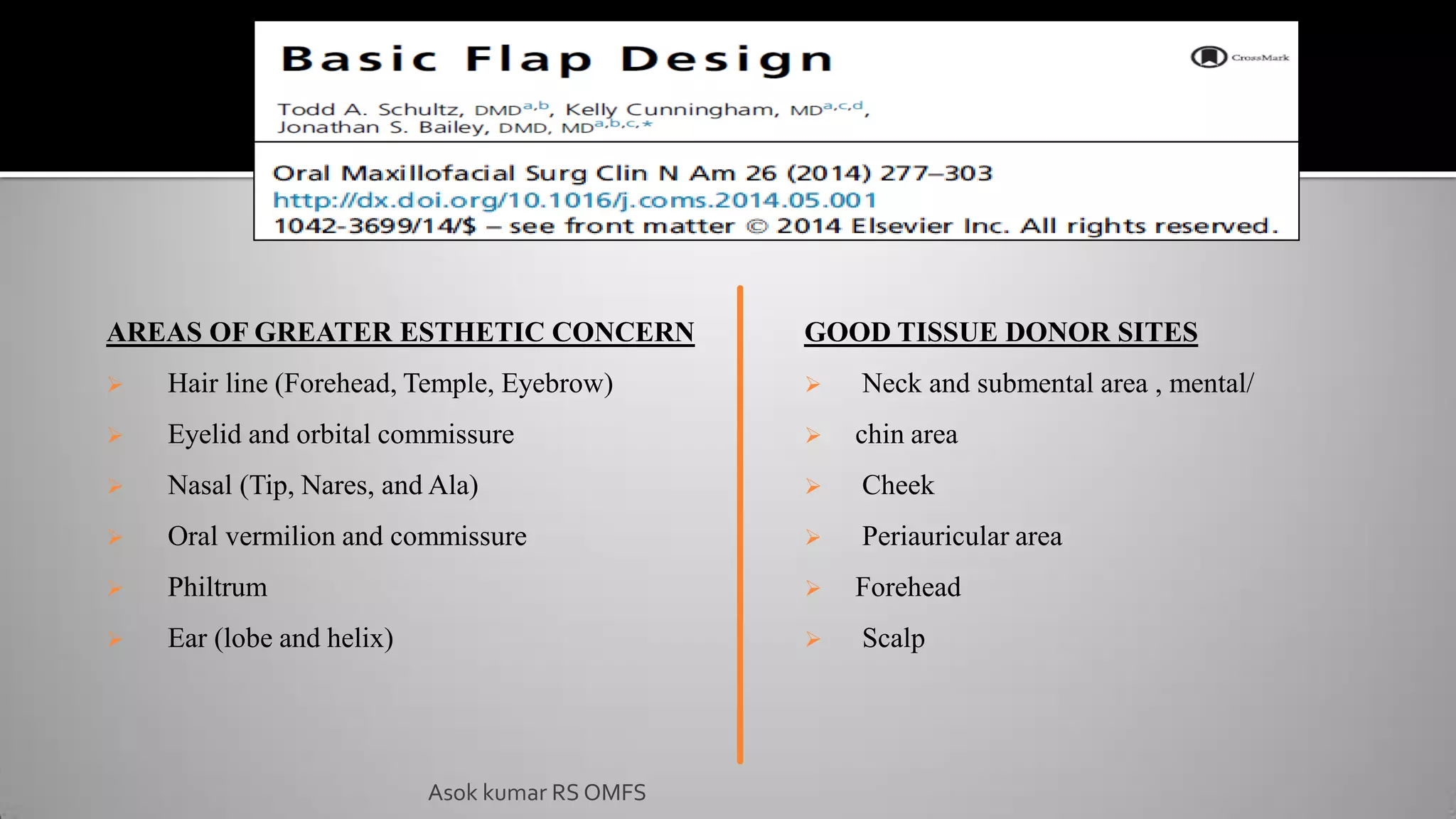
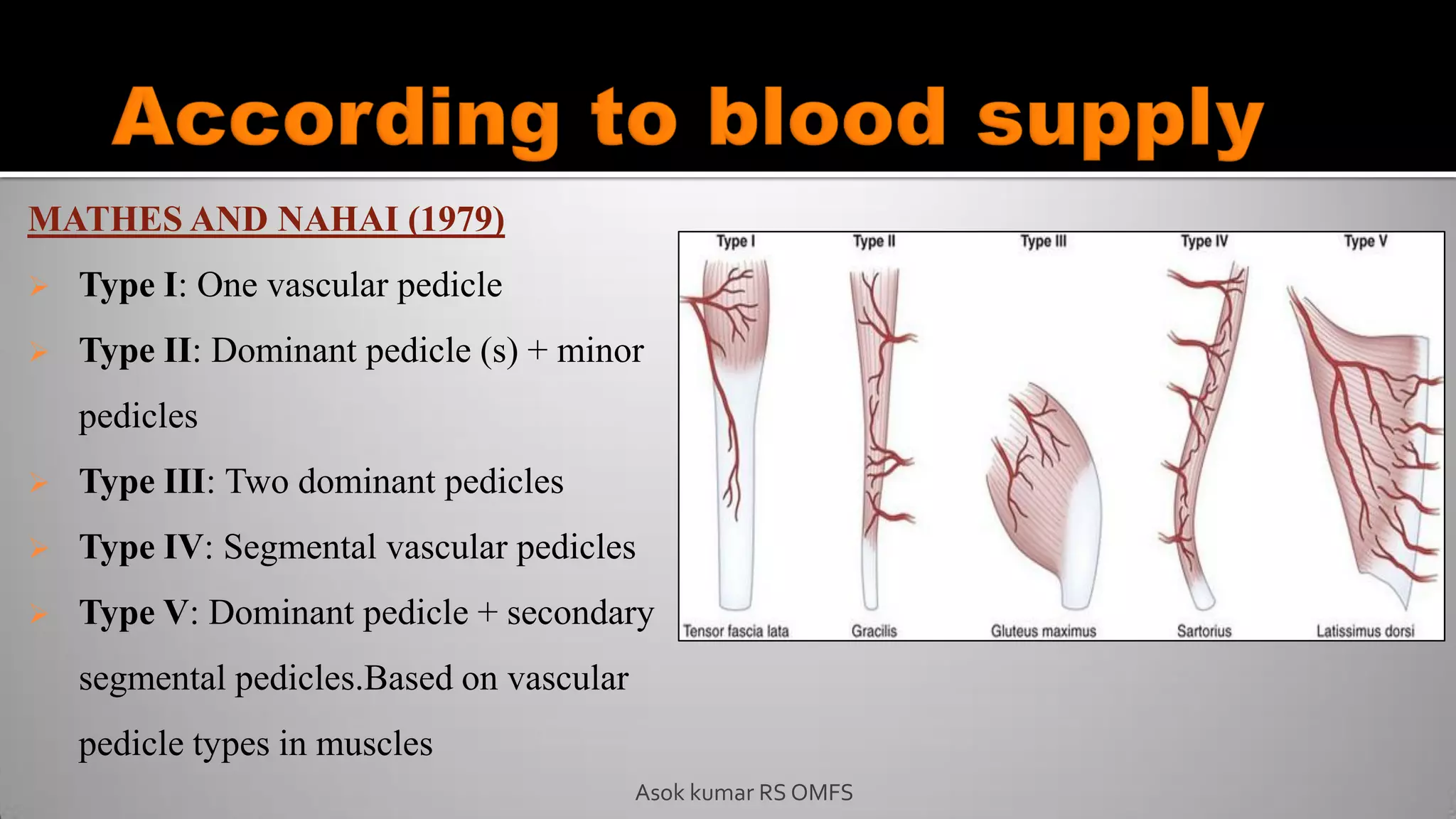
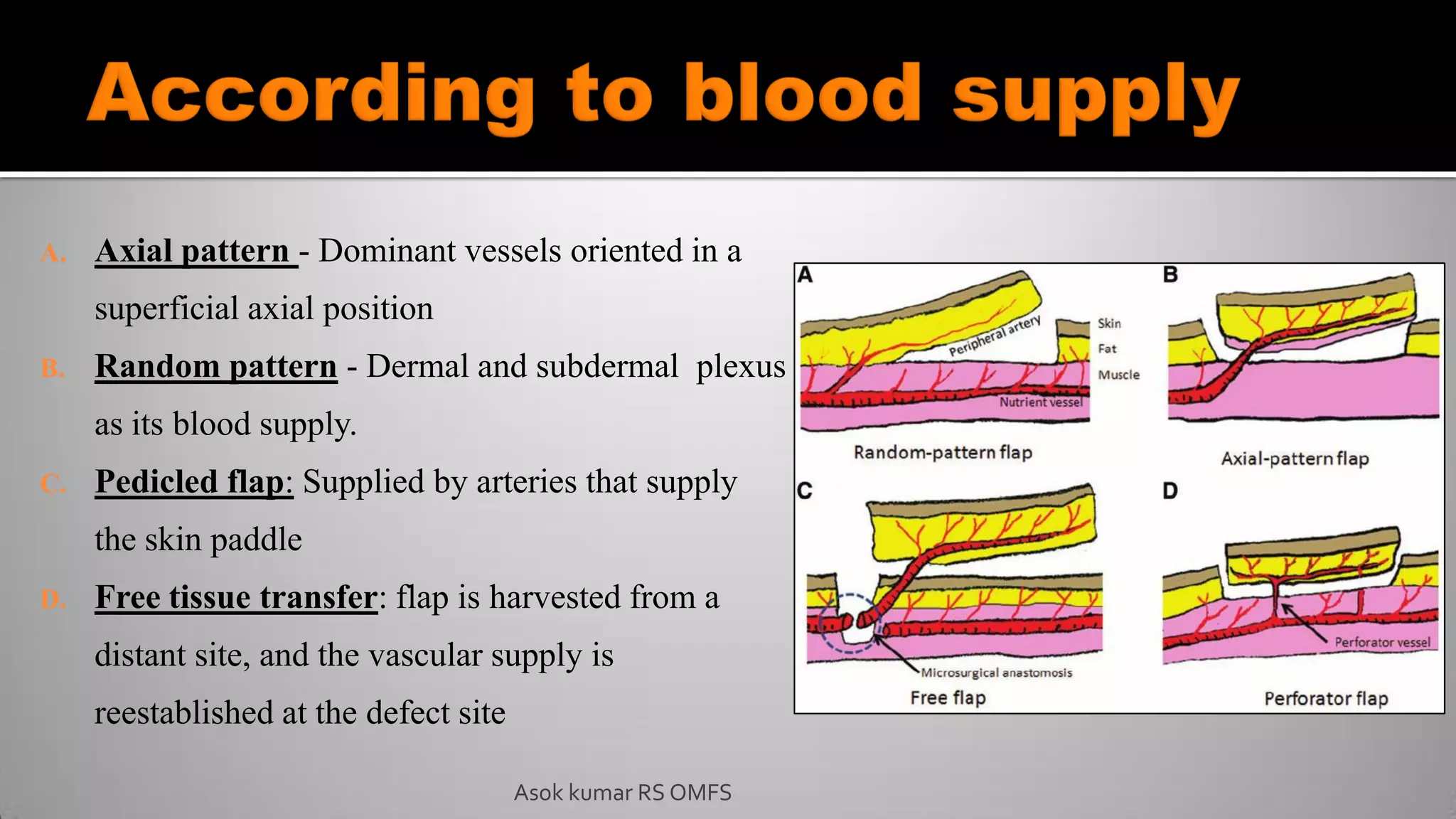
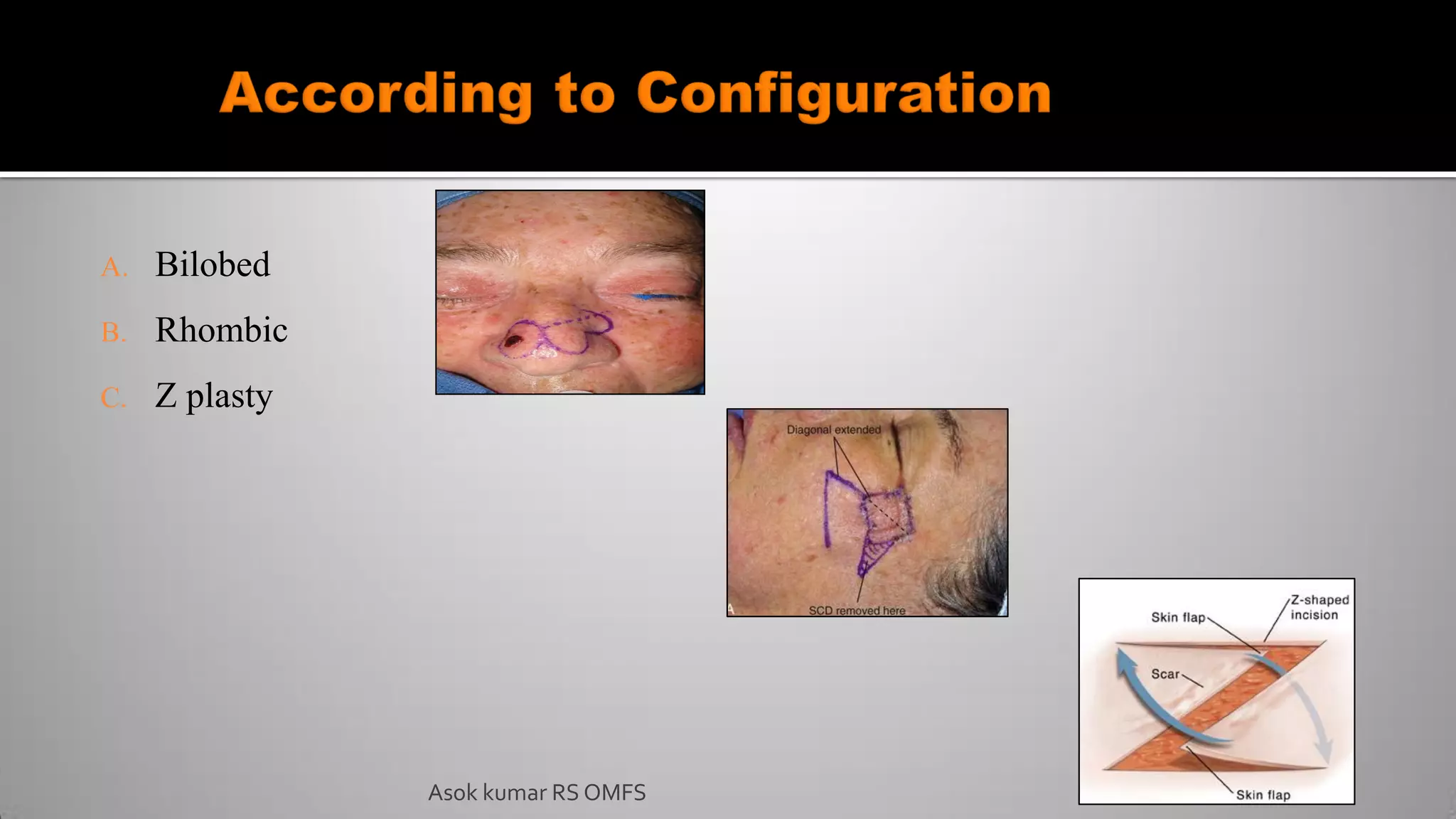
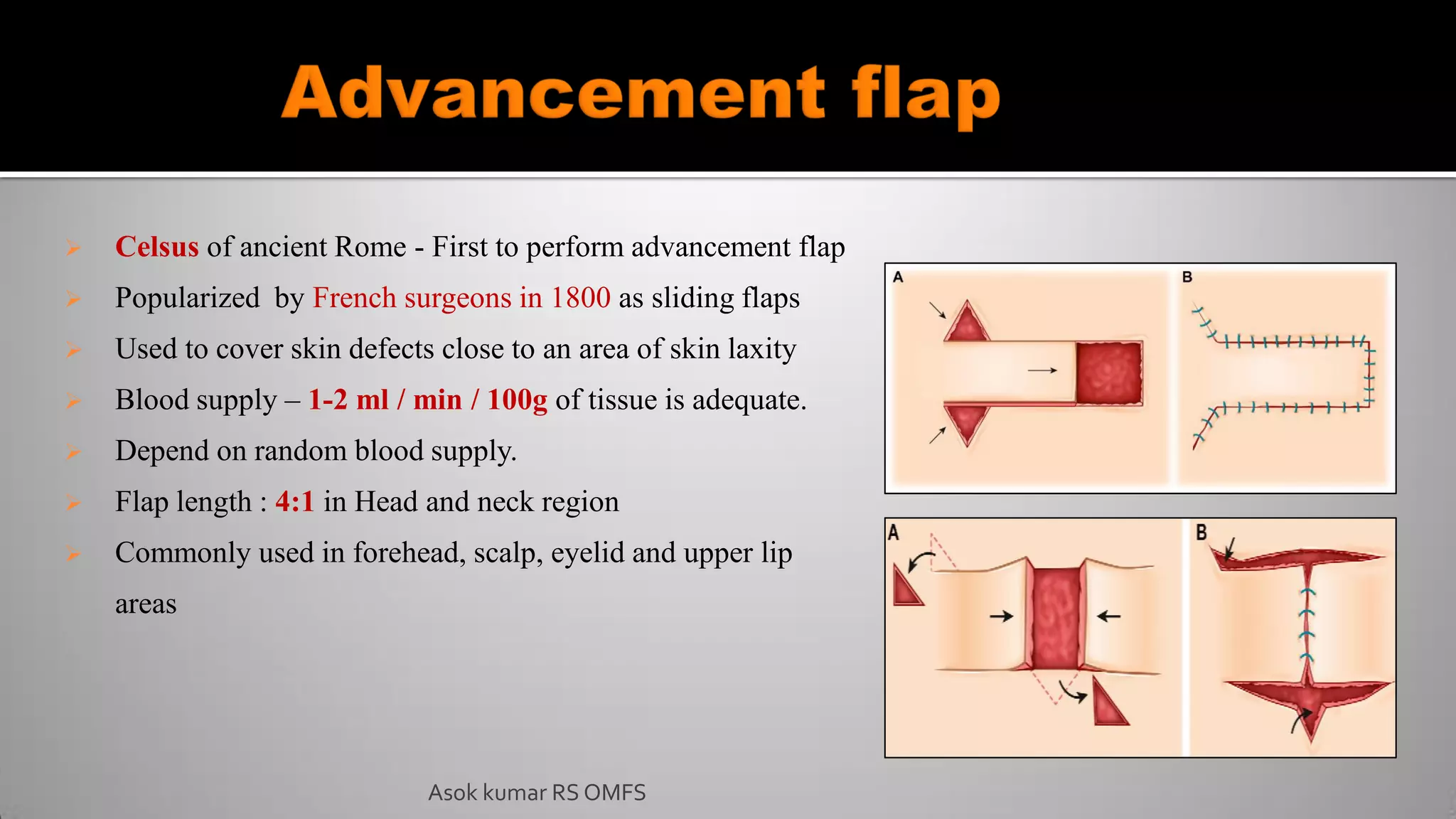
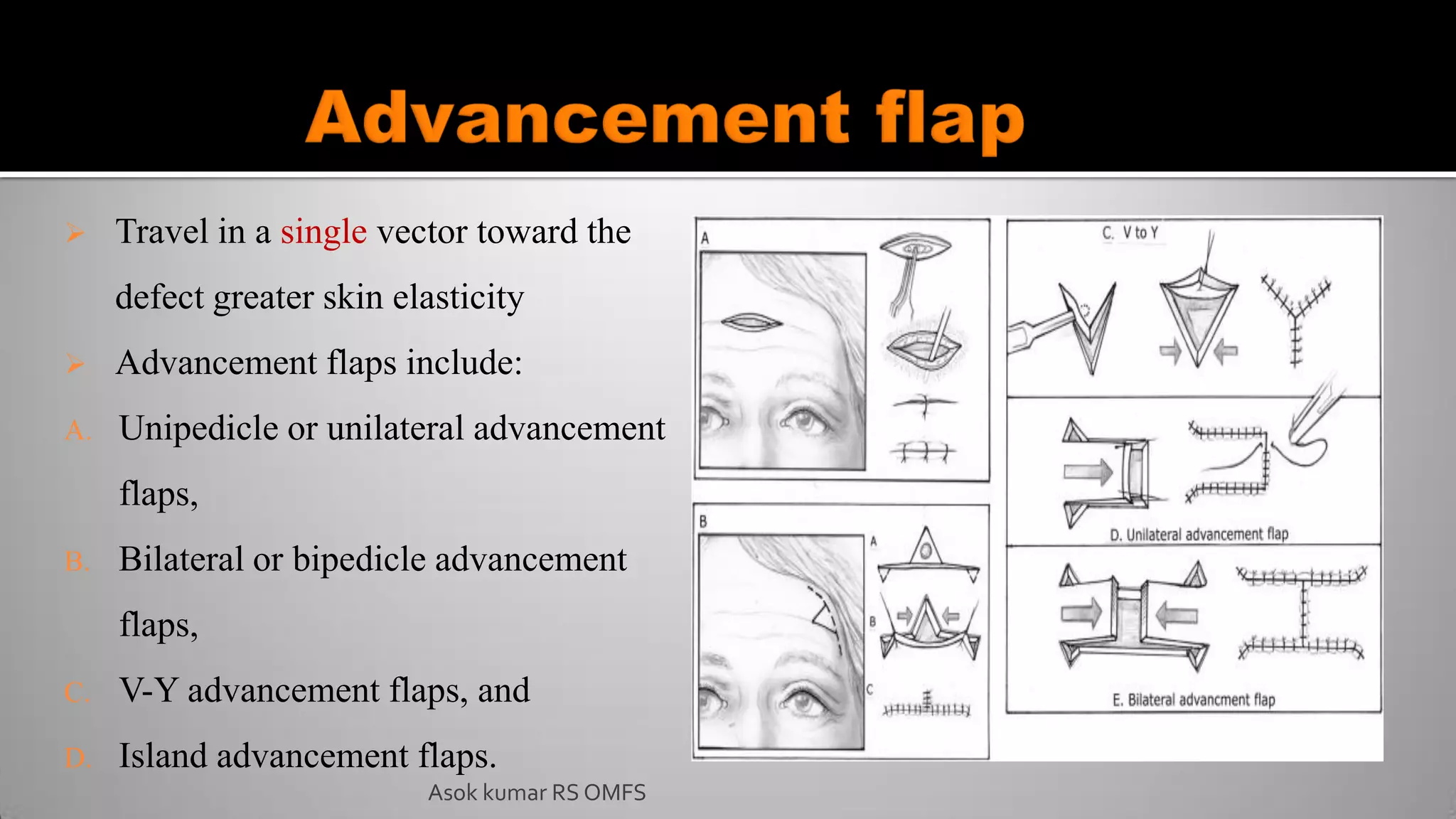
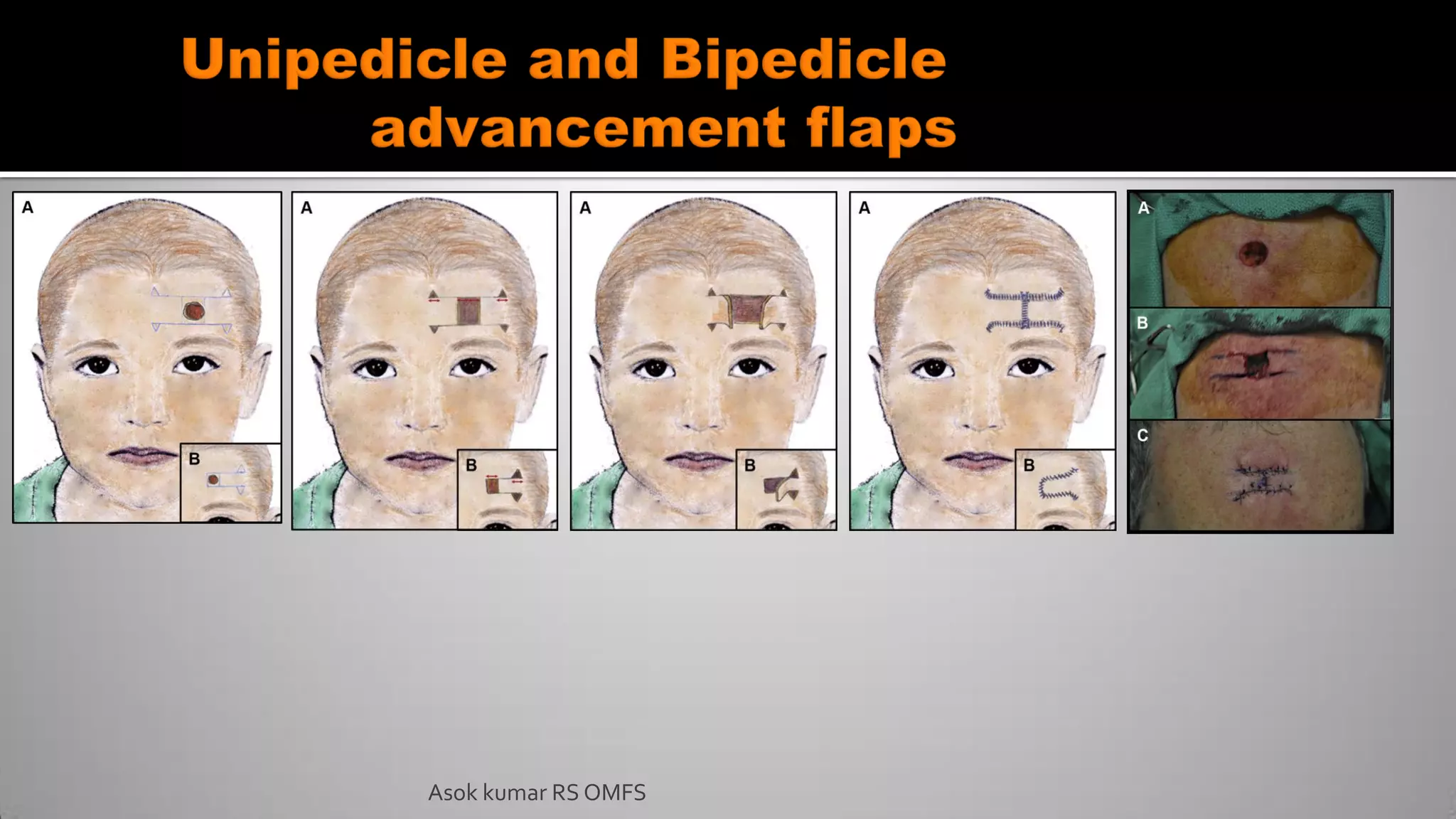
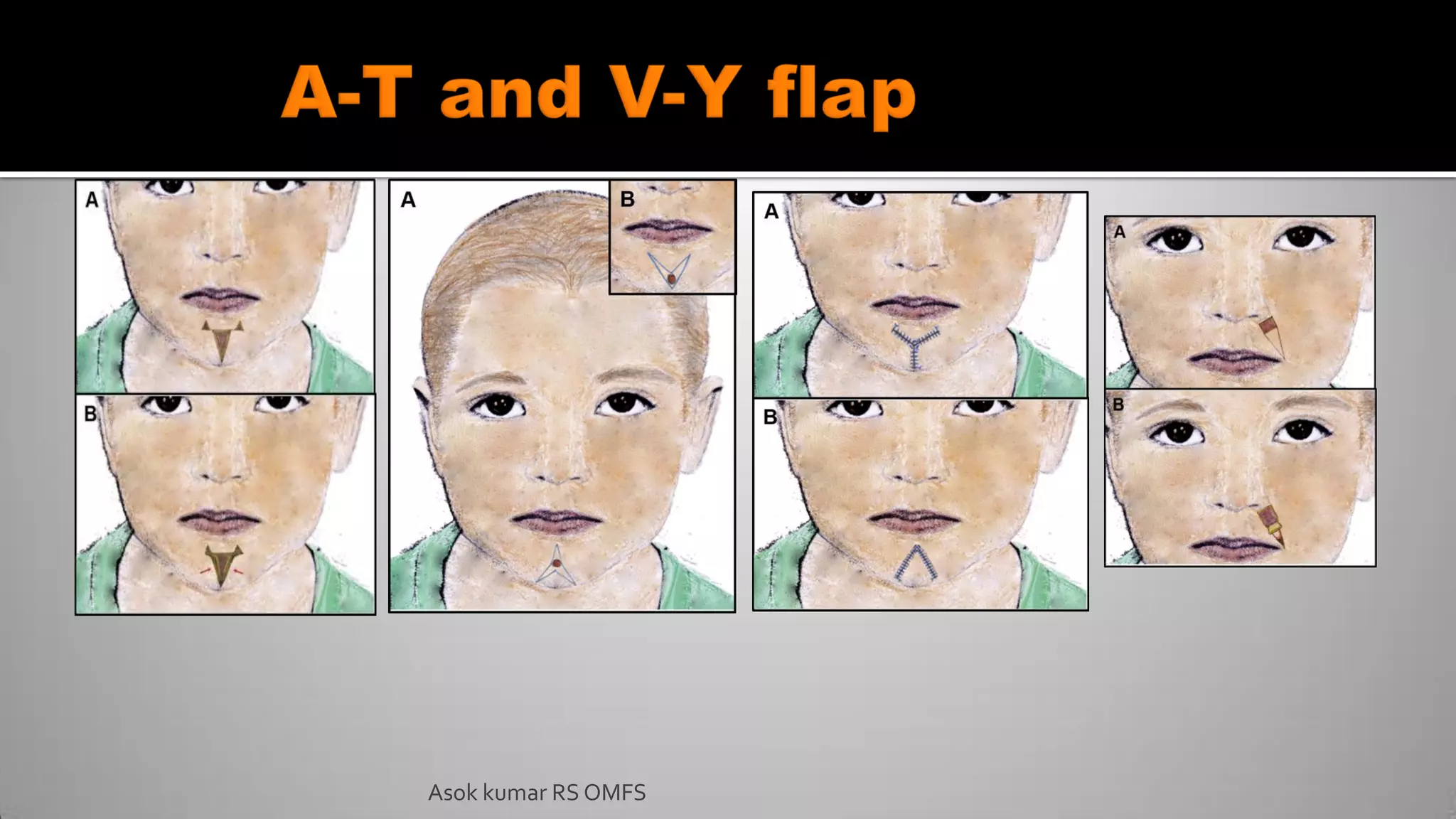
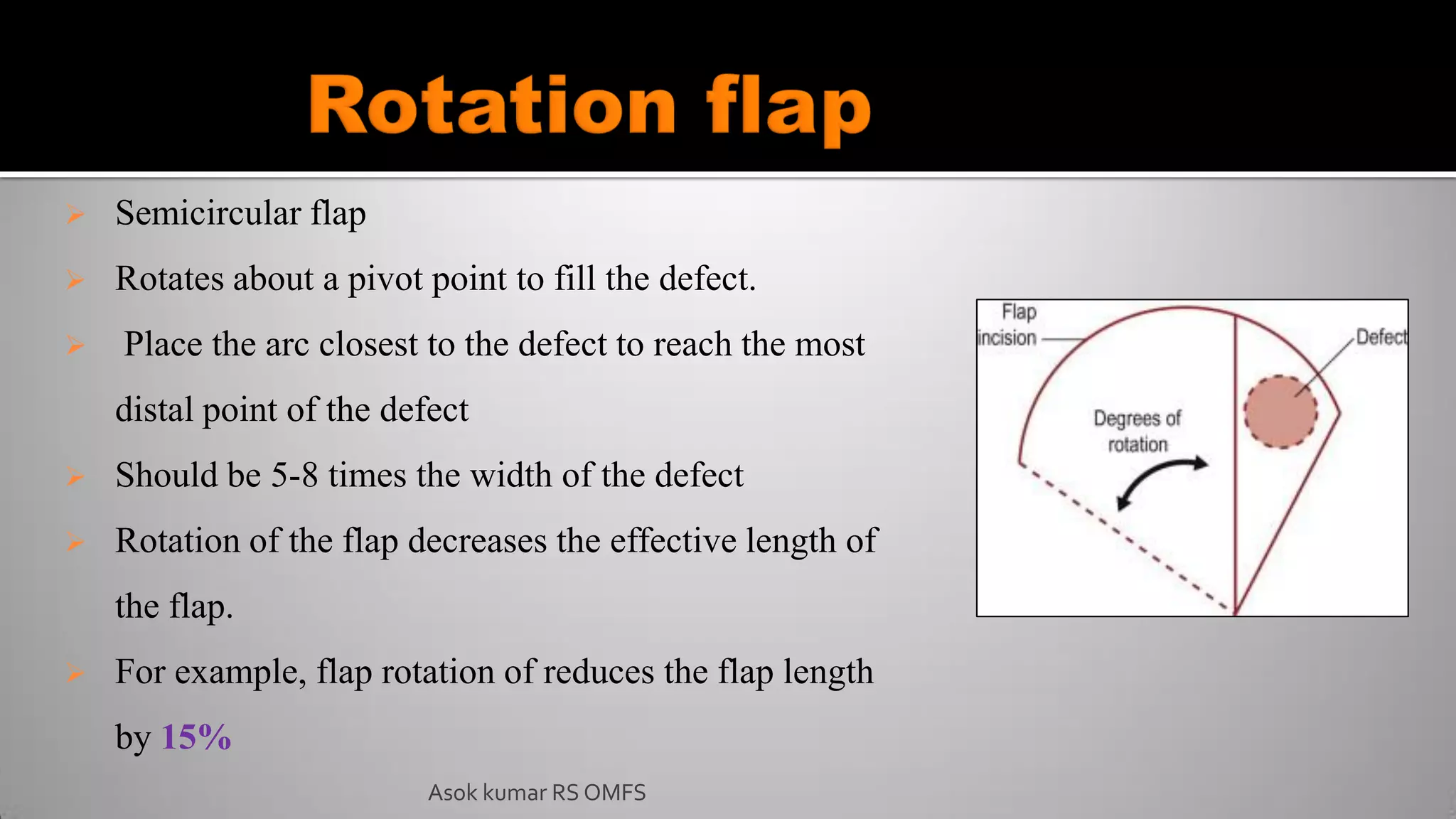
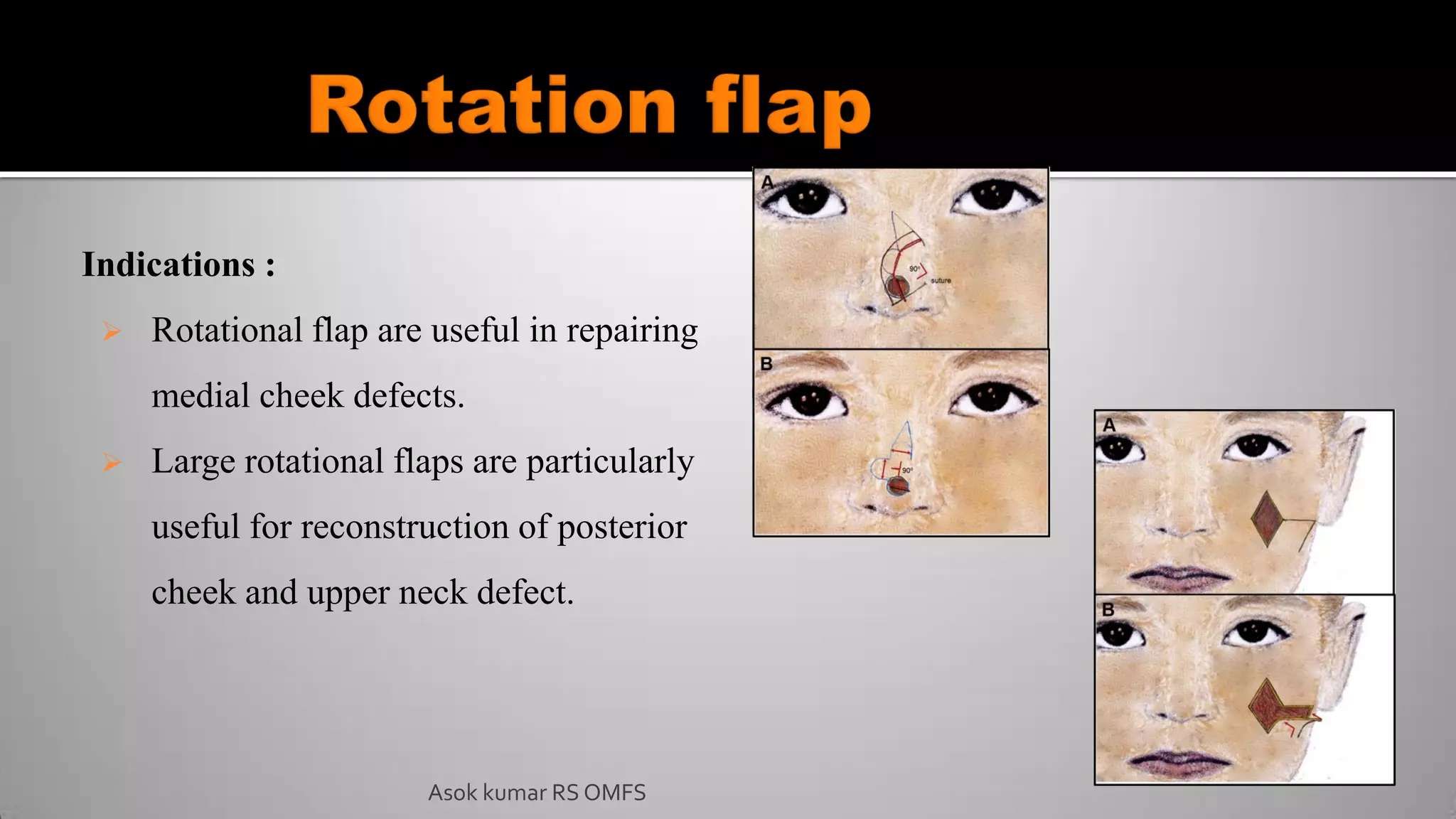
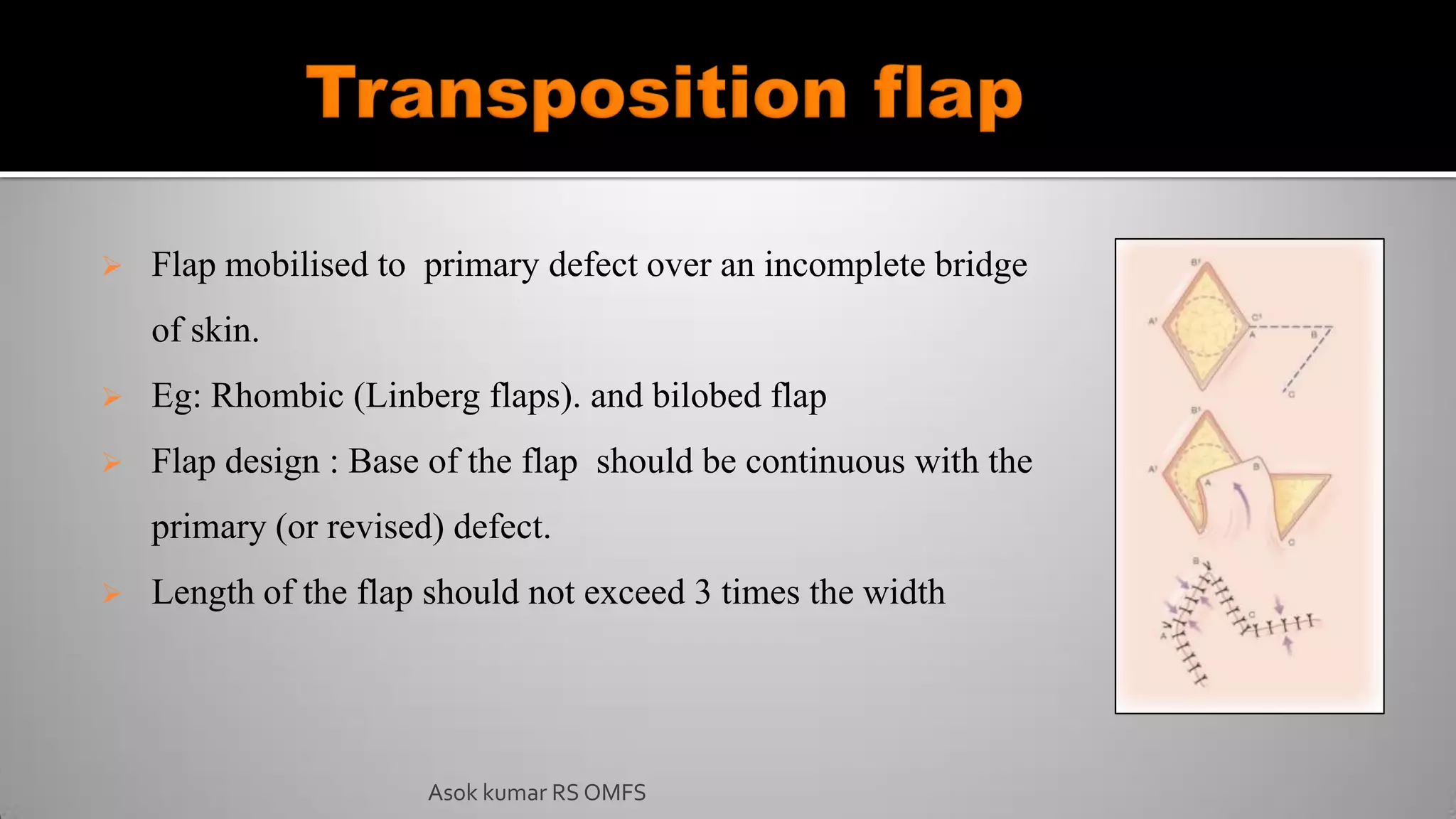
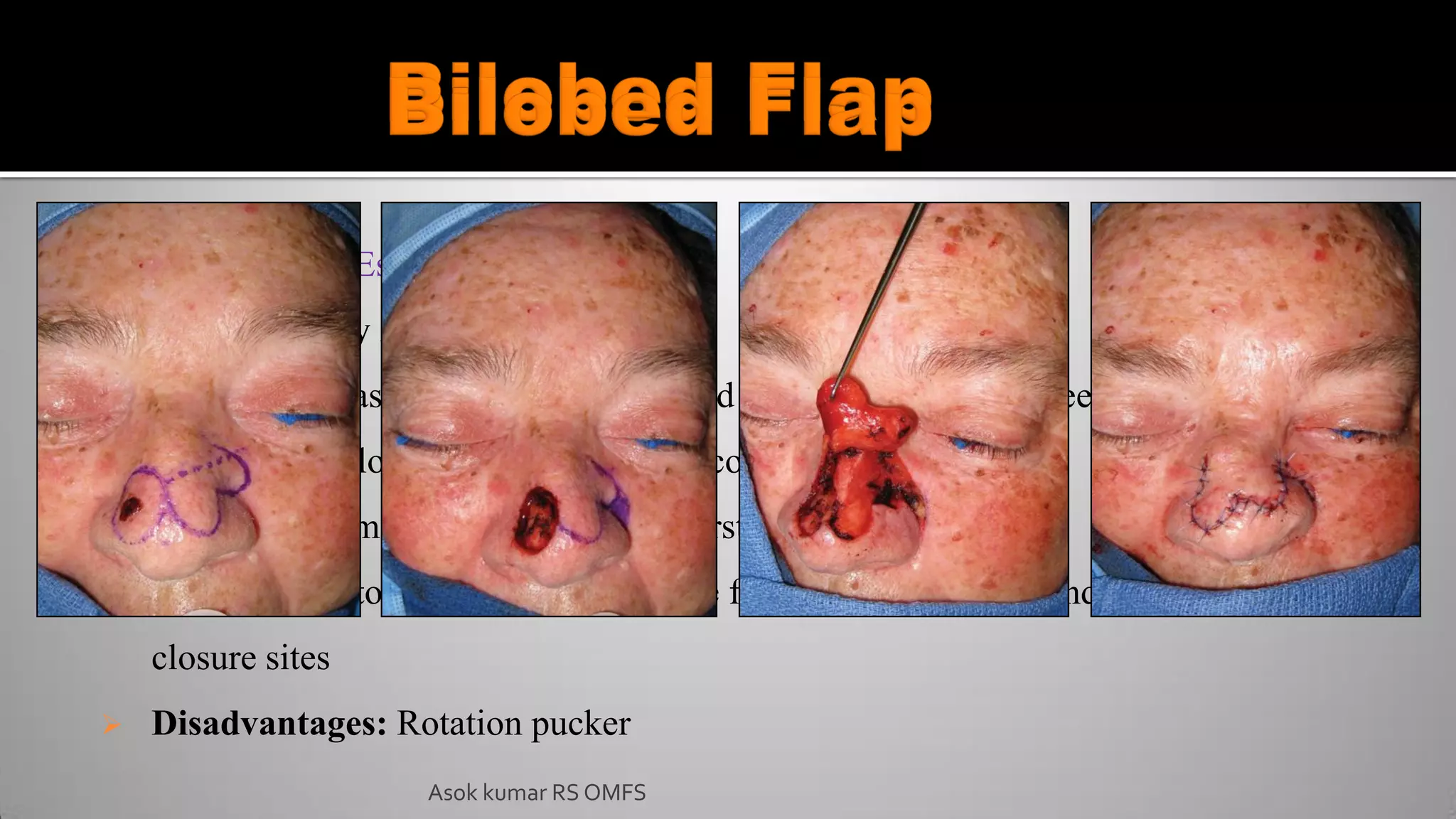
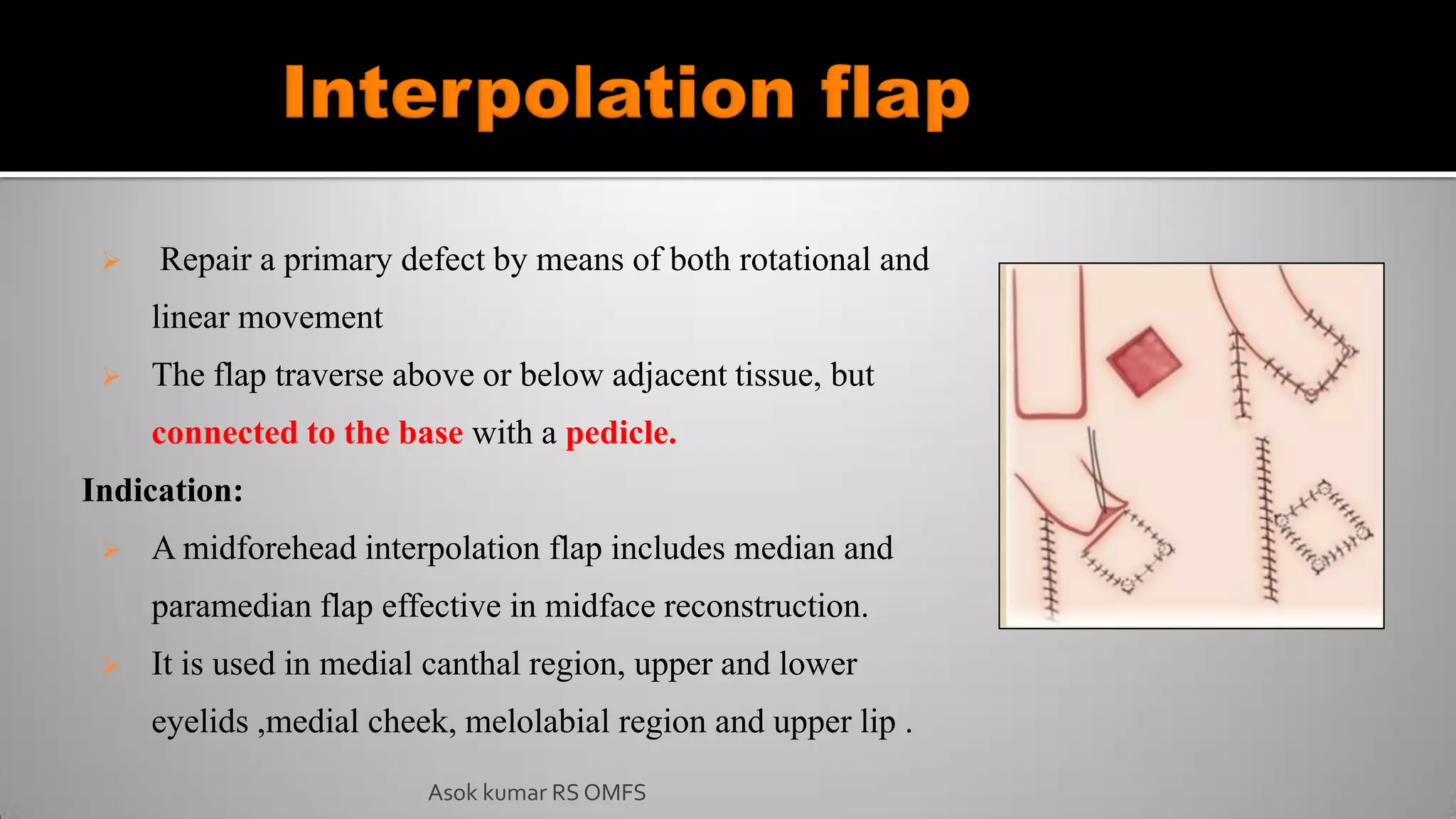
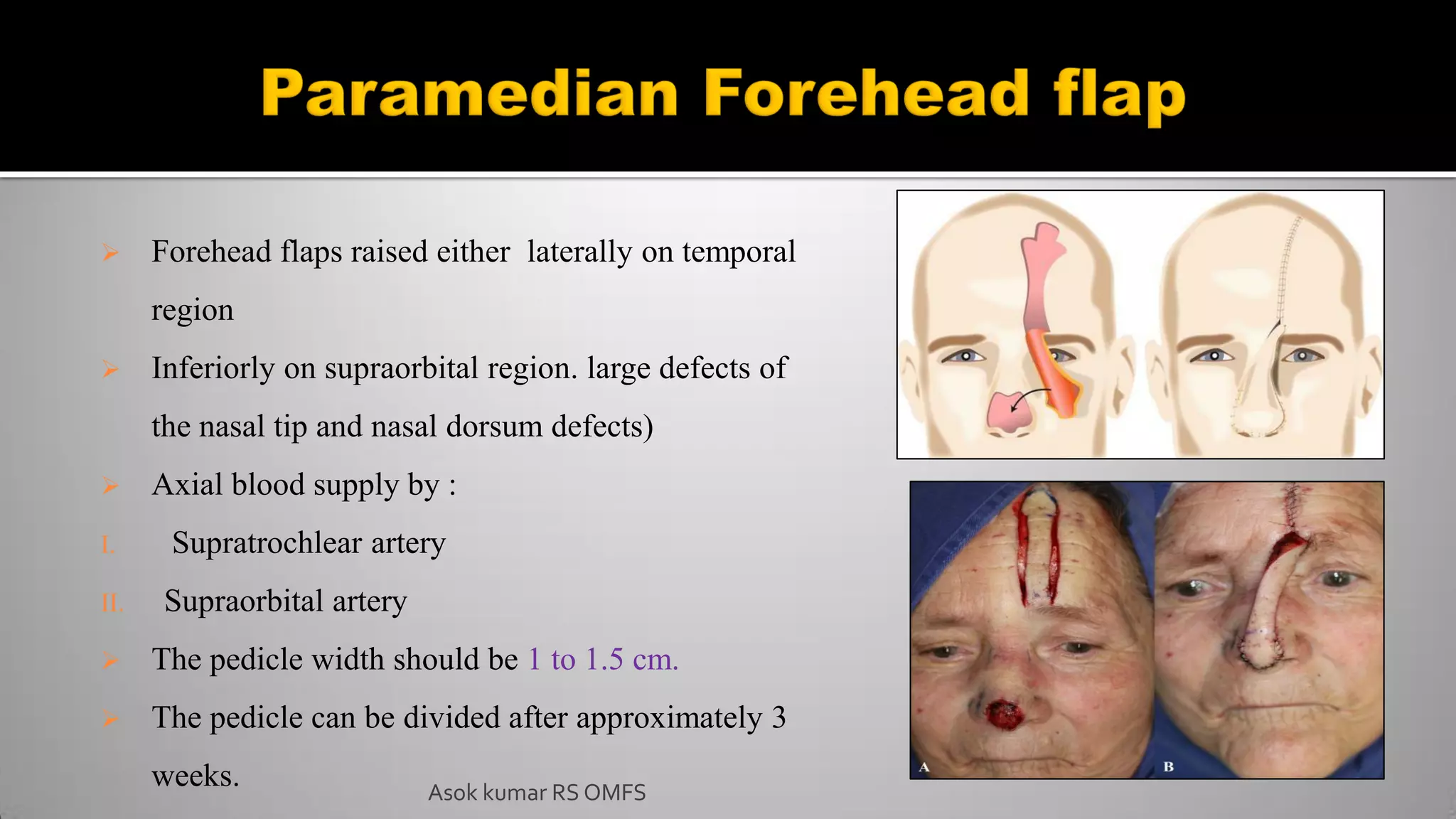
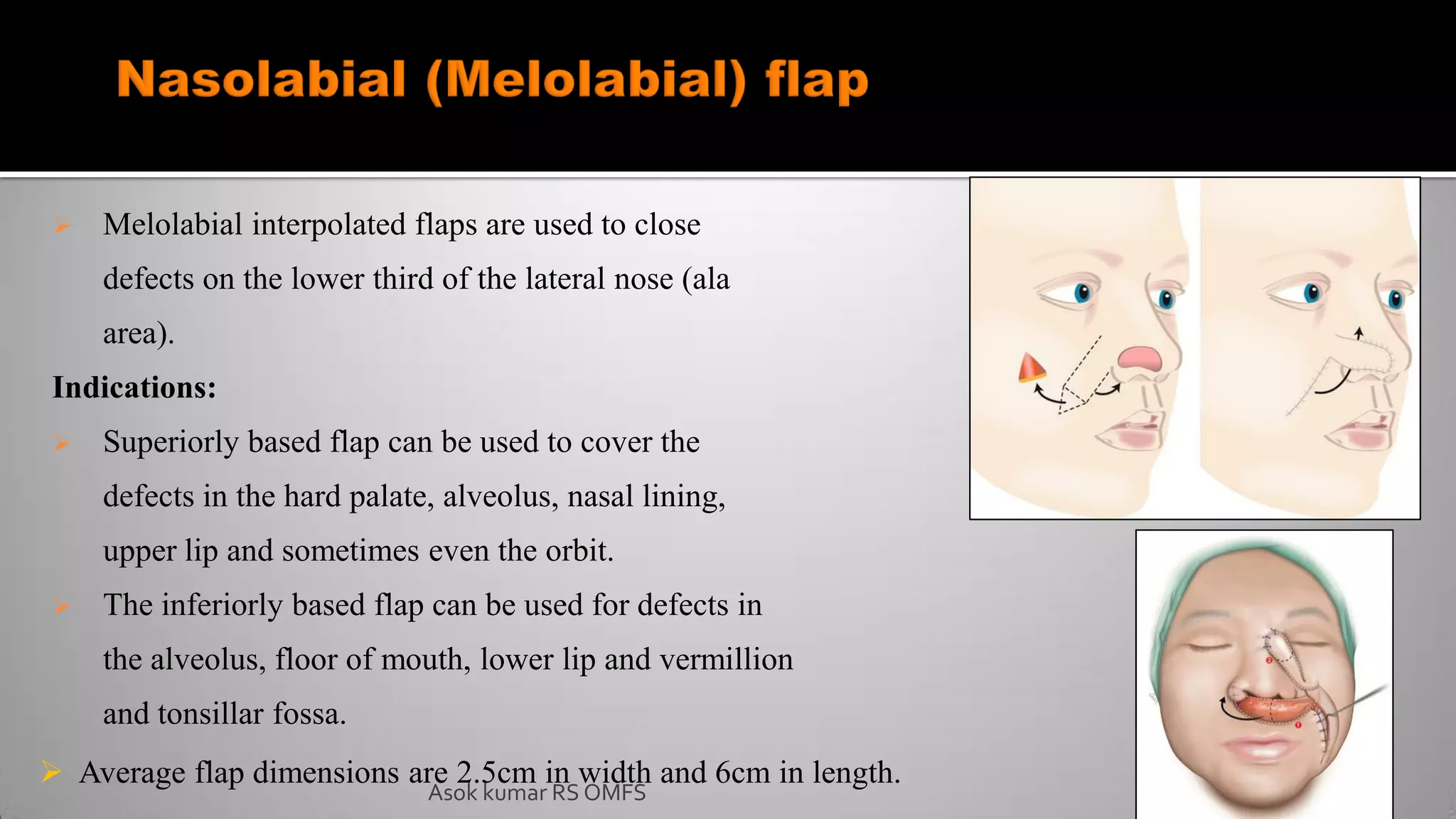
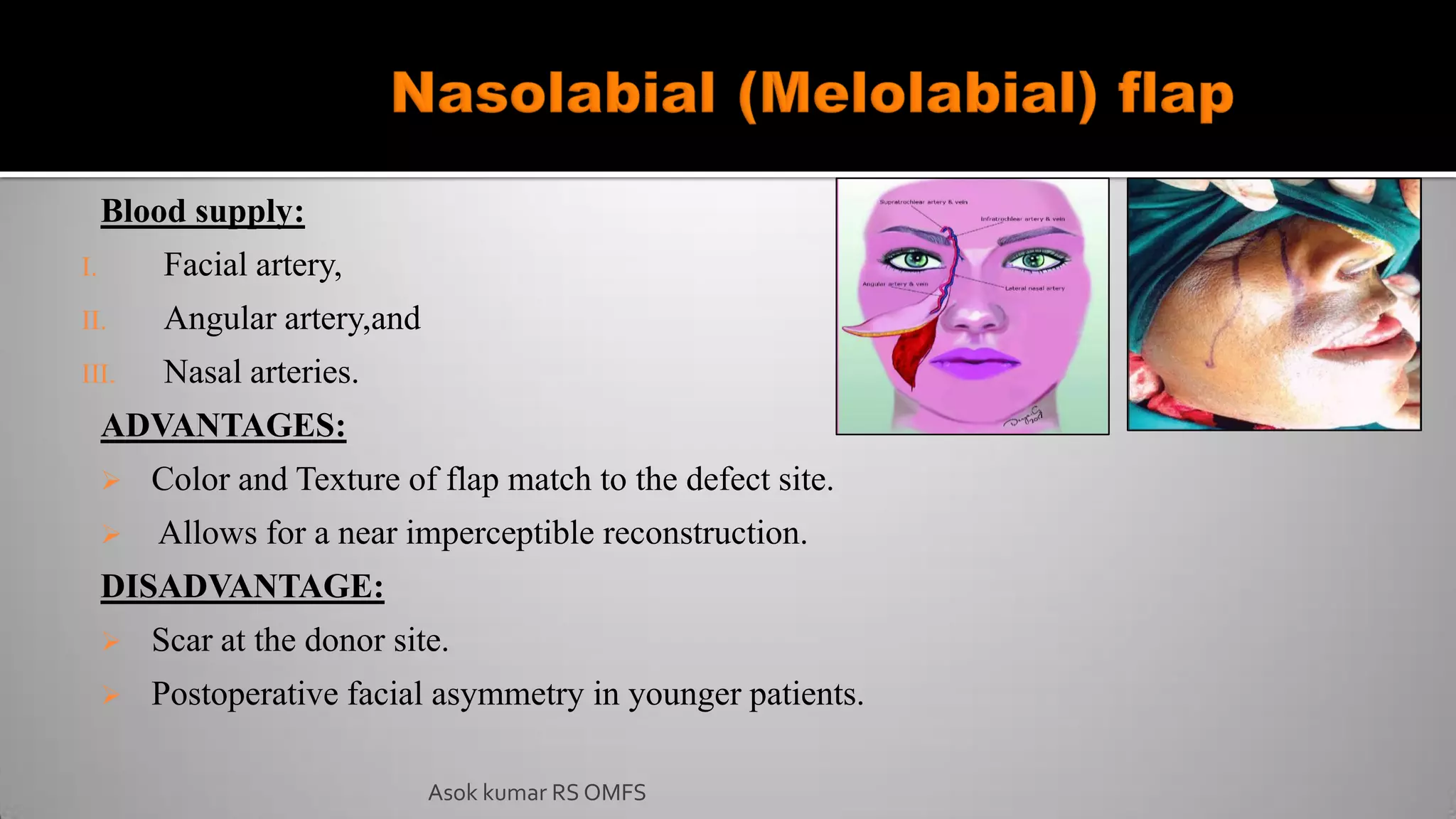
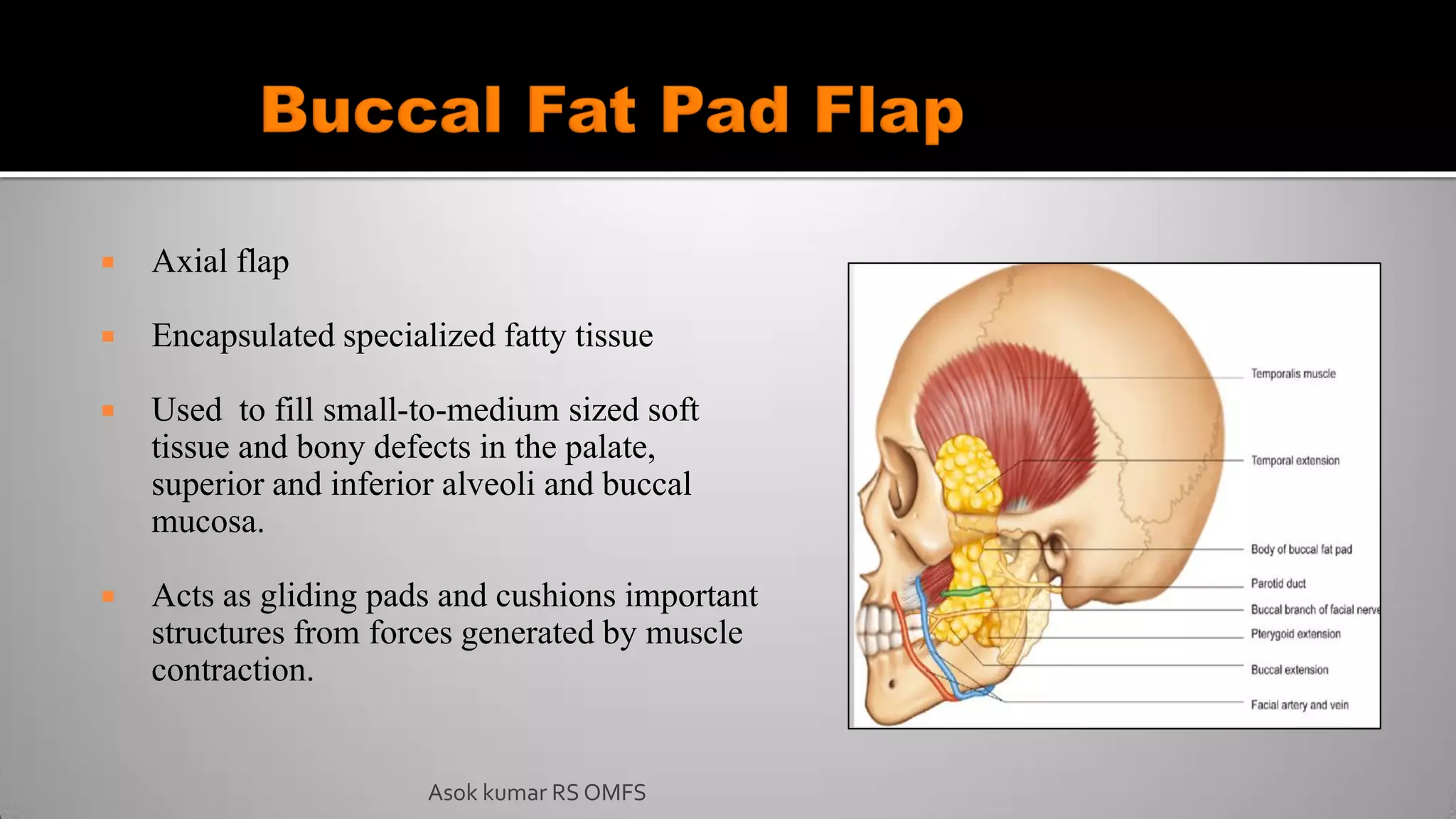
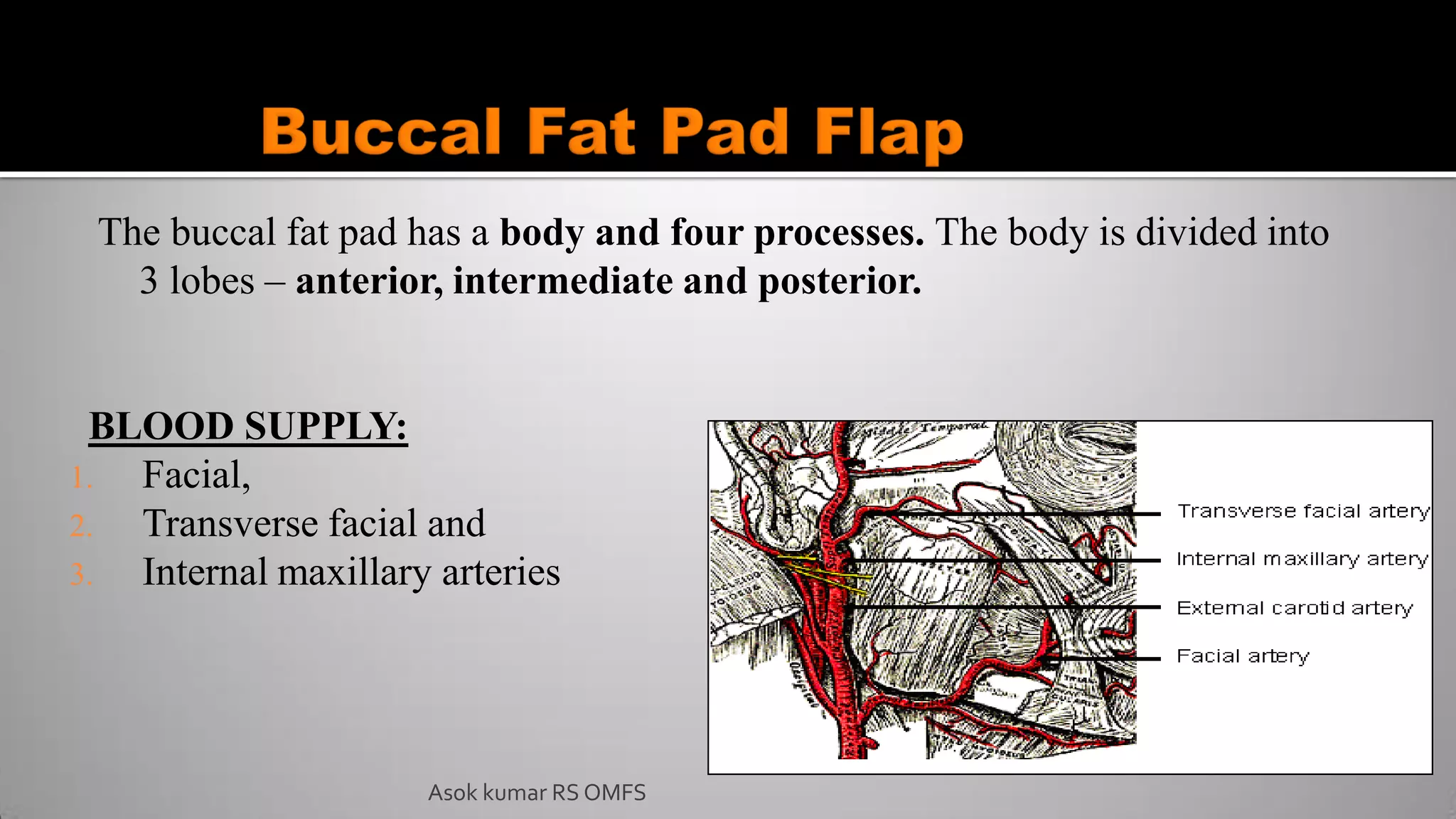
This document discusses the history and types of flaps used in reconstructive surgery. It begins by defining a flap as a unit of tissue transferred from a donor site to a recipient site while maintaining its own blood supply. It then discusses the origins of flaps dating back to 600 BC and highlights some important developments over time, including the first use of forehead and cheek flaps for nasal reconstruction. The document outlines different ways flaps can be classified, such as by blood supply, location, tissue content, configuration, and transfer method. Specific flap types are defined, such as advancement, rotational, and interpolated flaps. Key considerations for flap design like tension lines and esthetic zones are also reviewed.