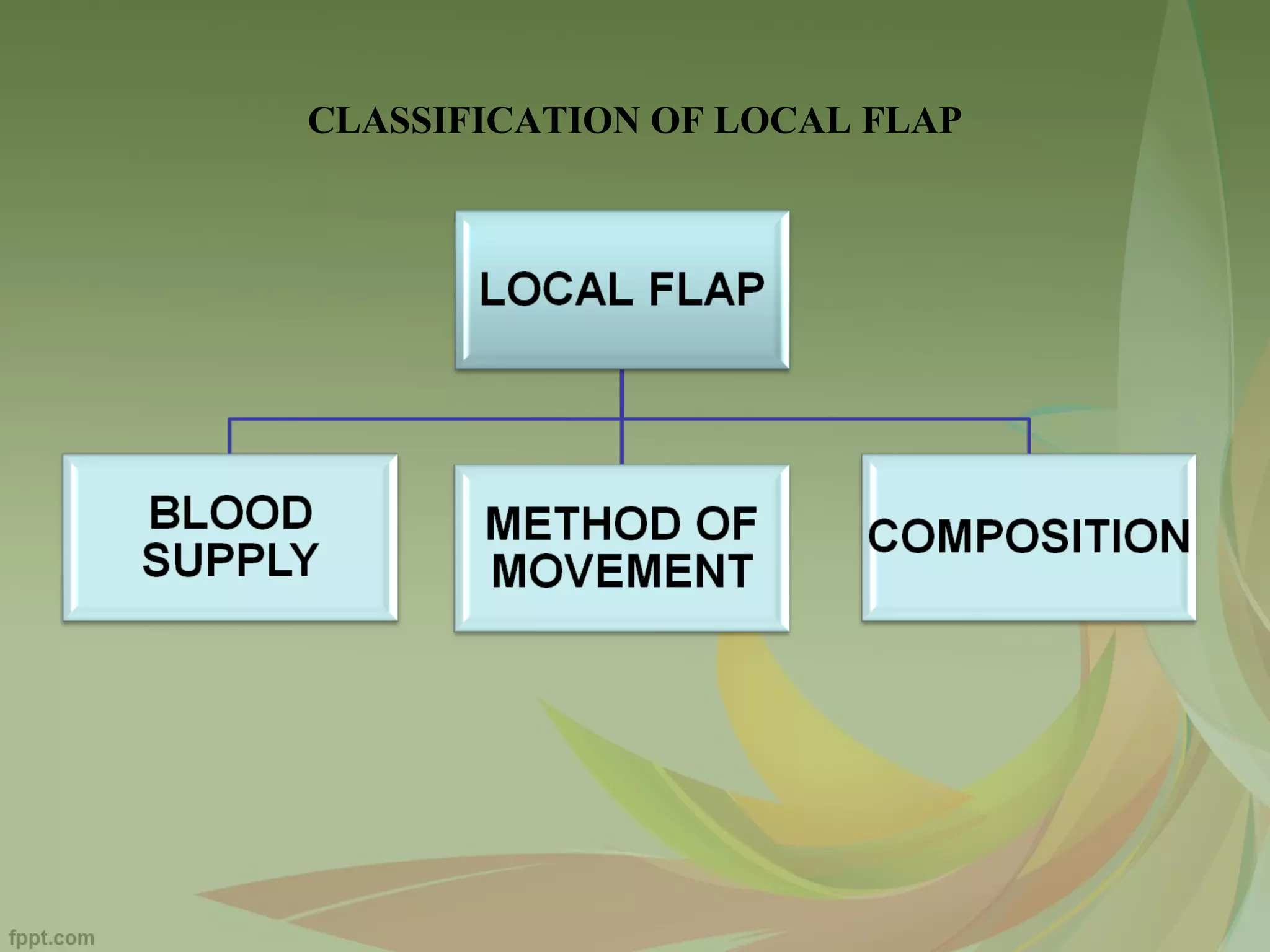
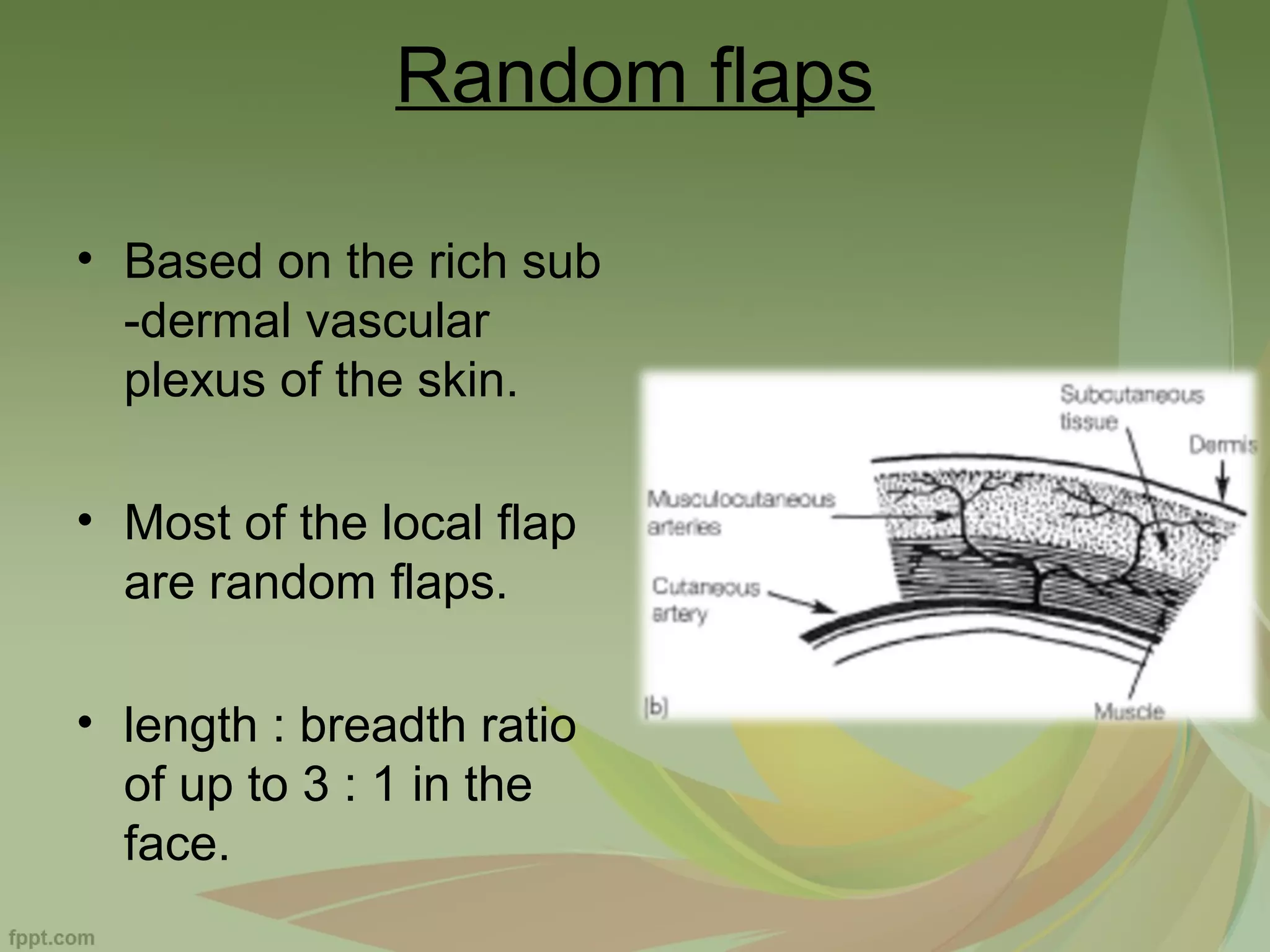
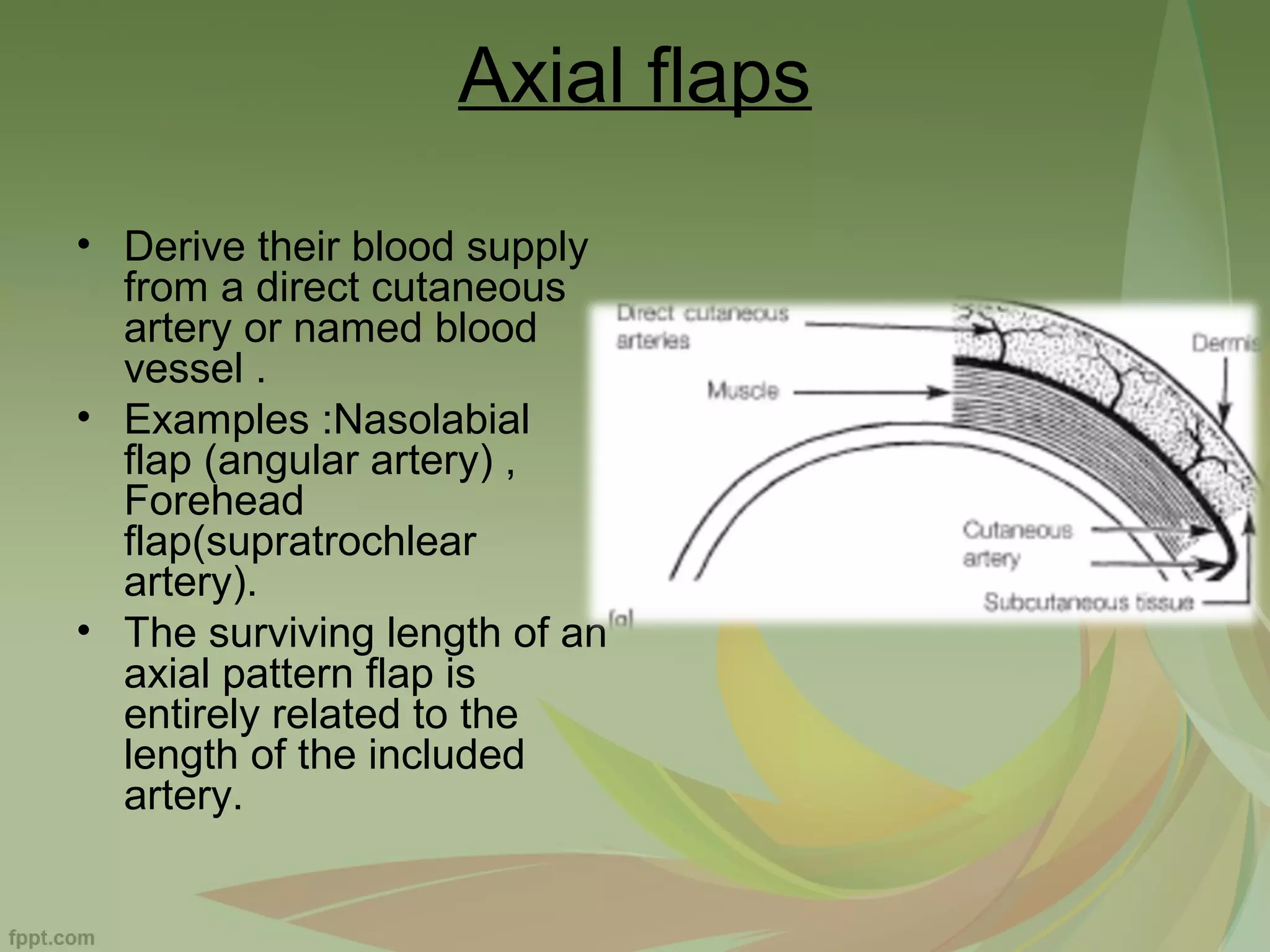
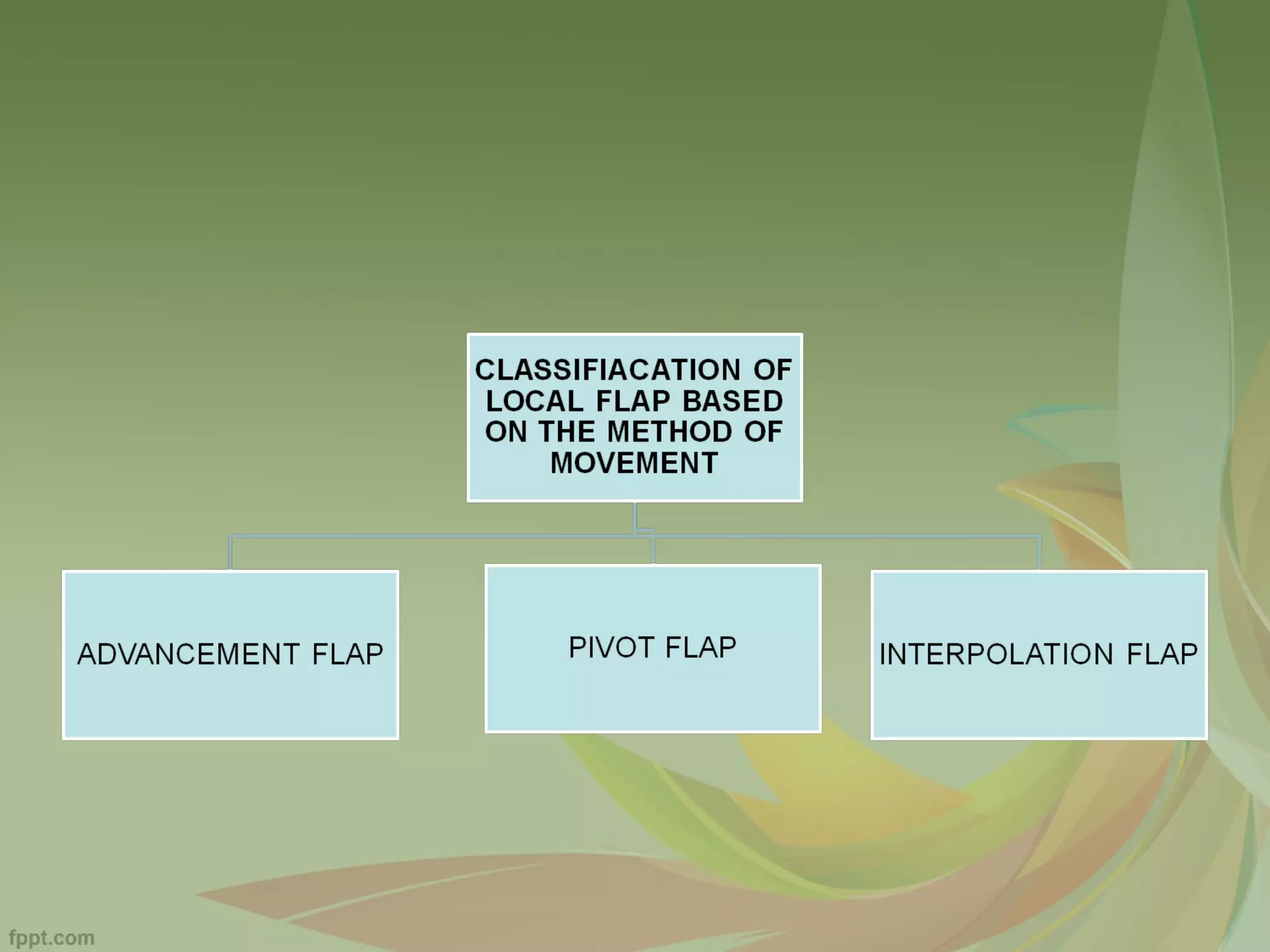
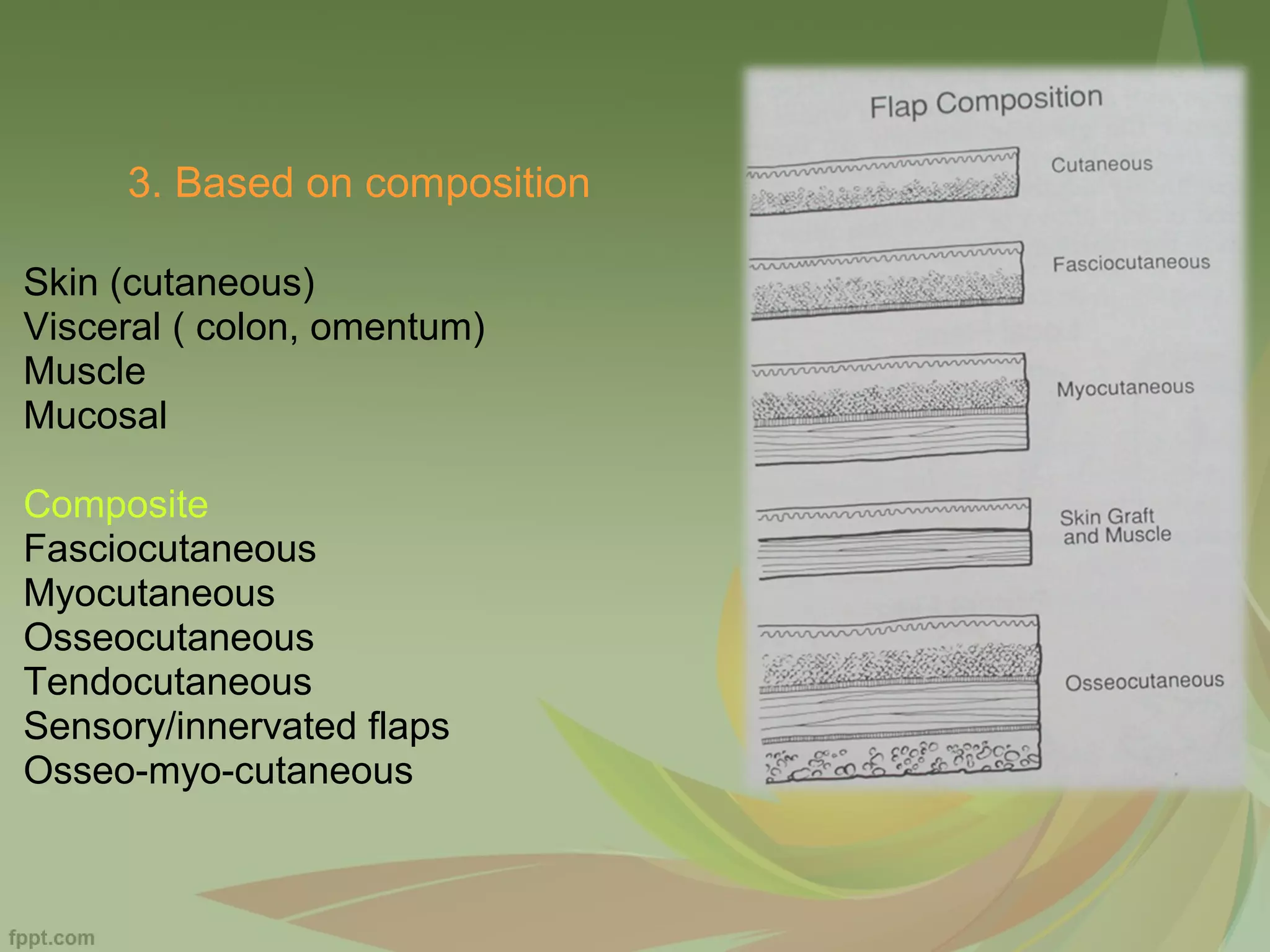
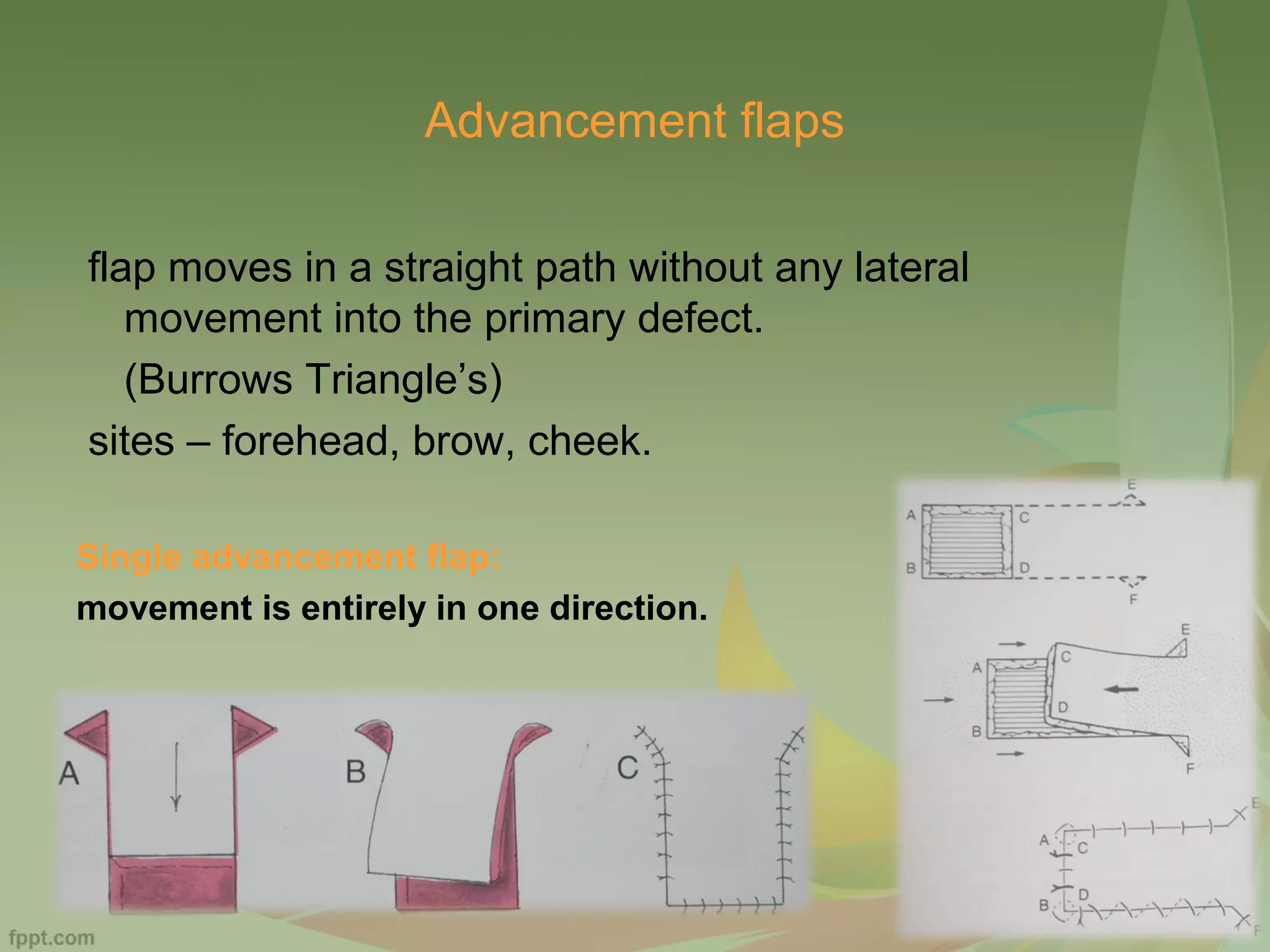
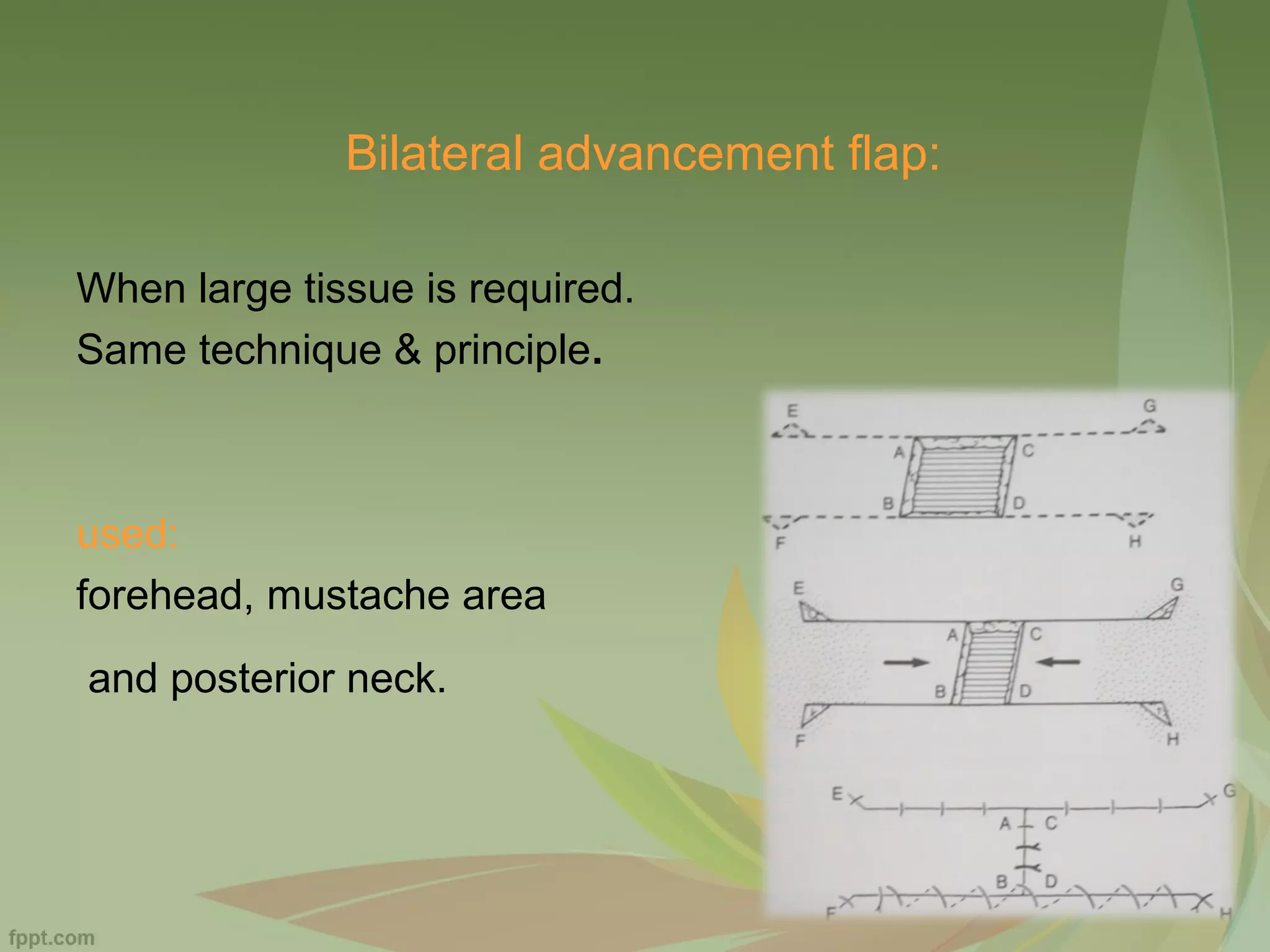
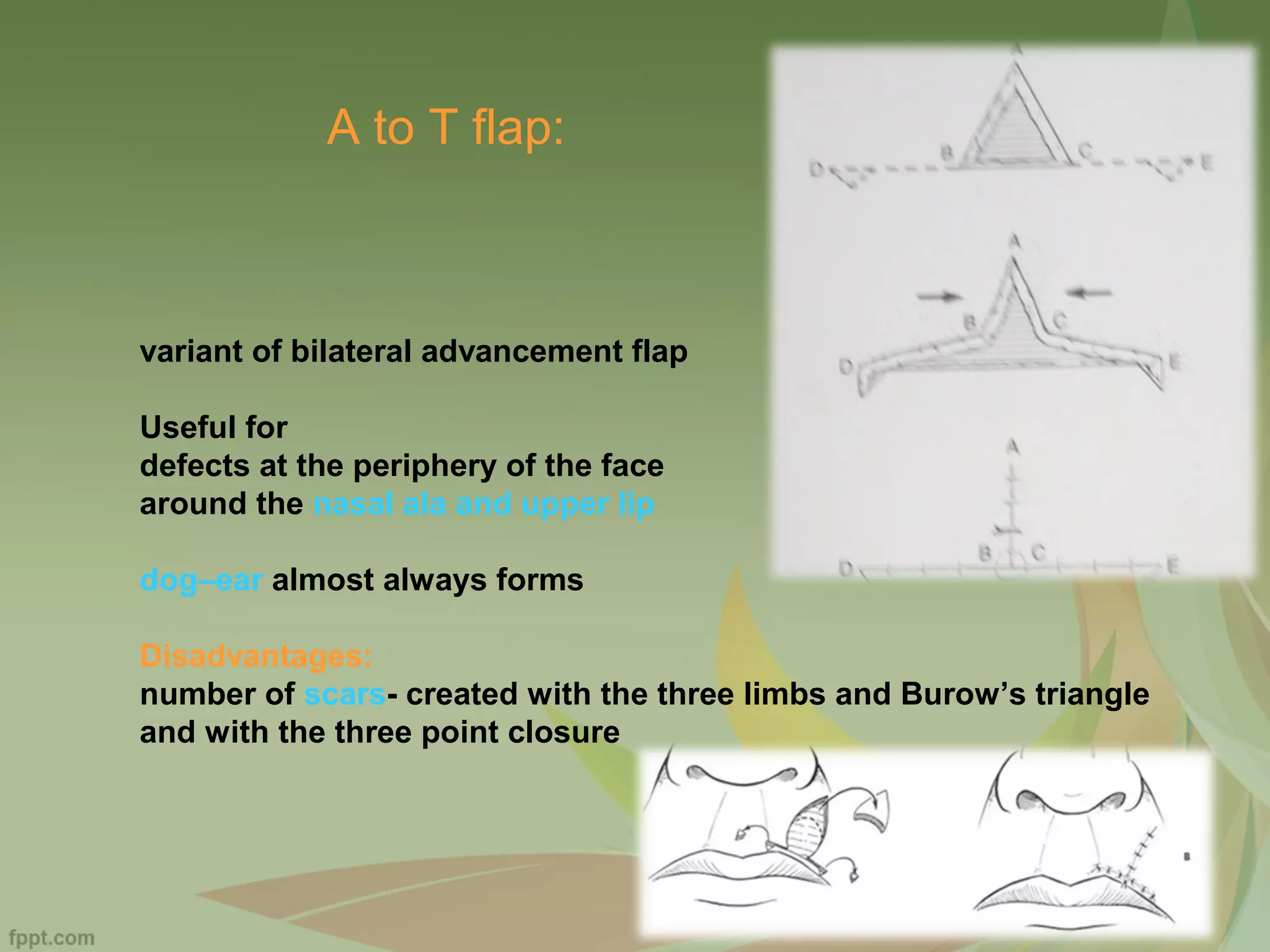
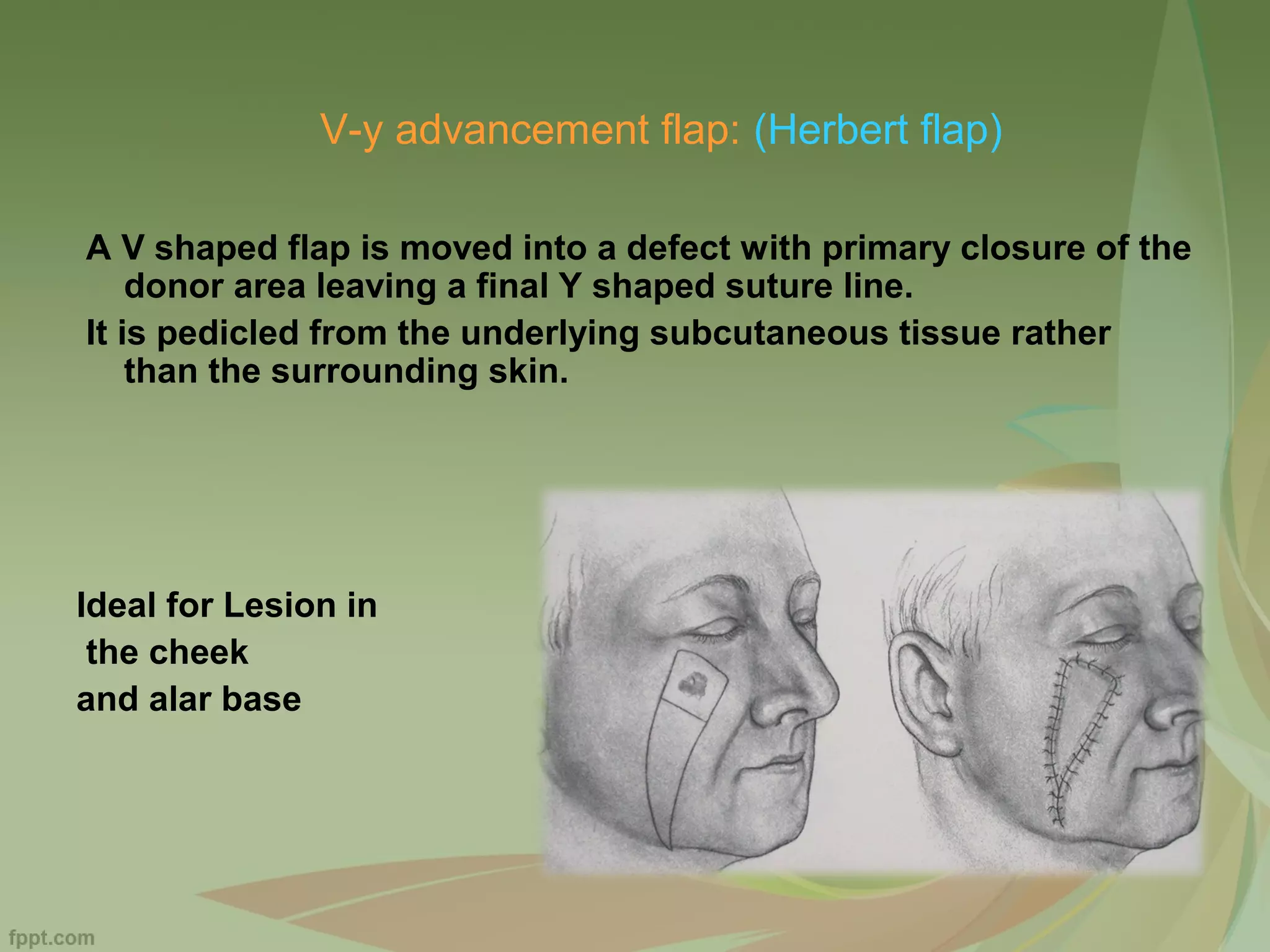
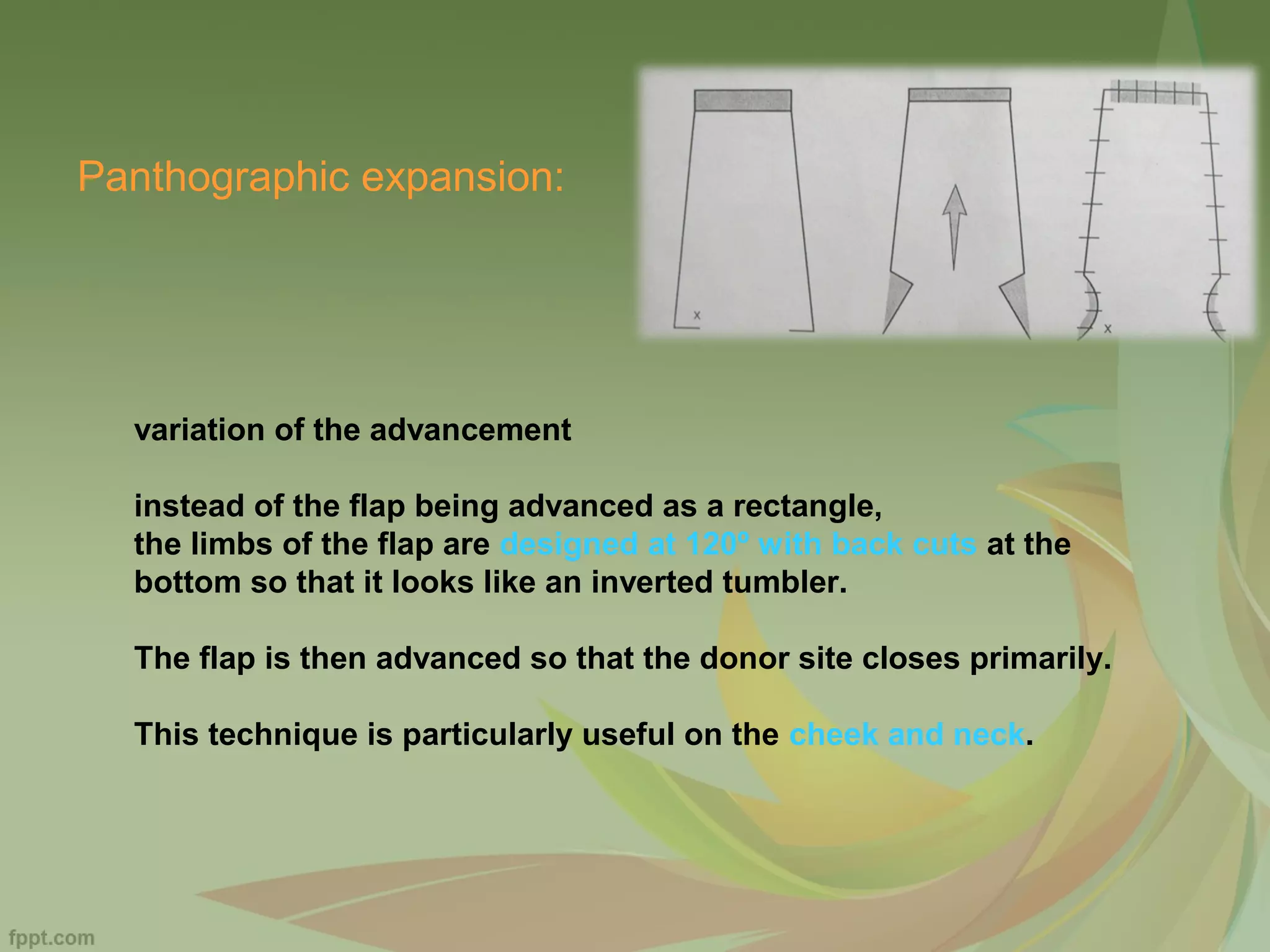
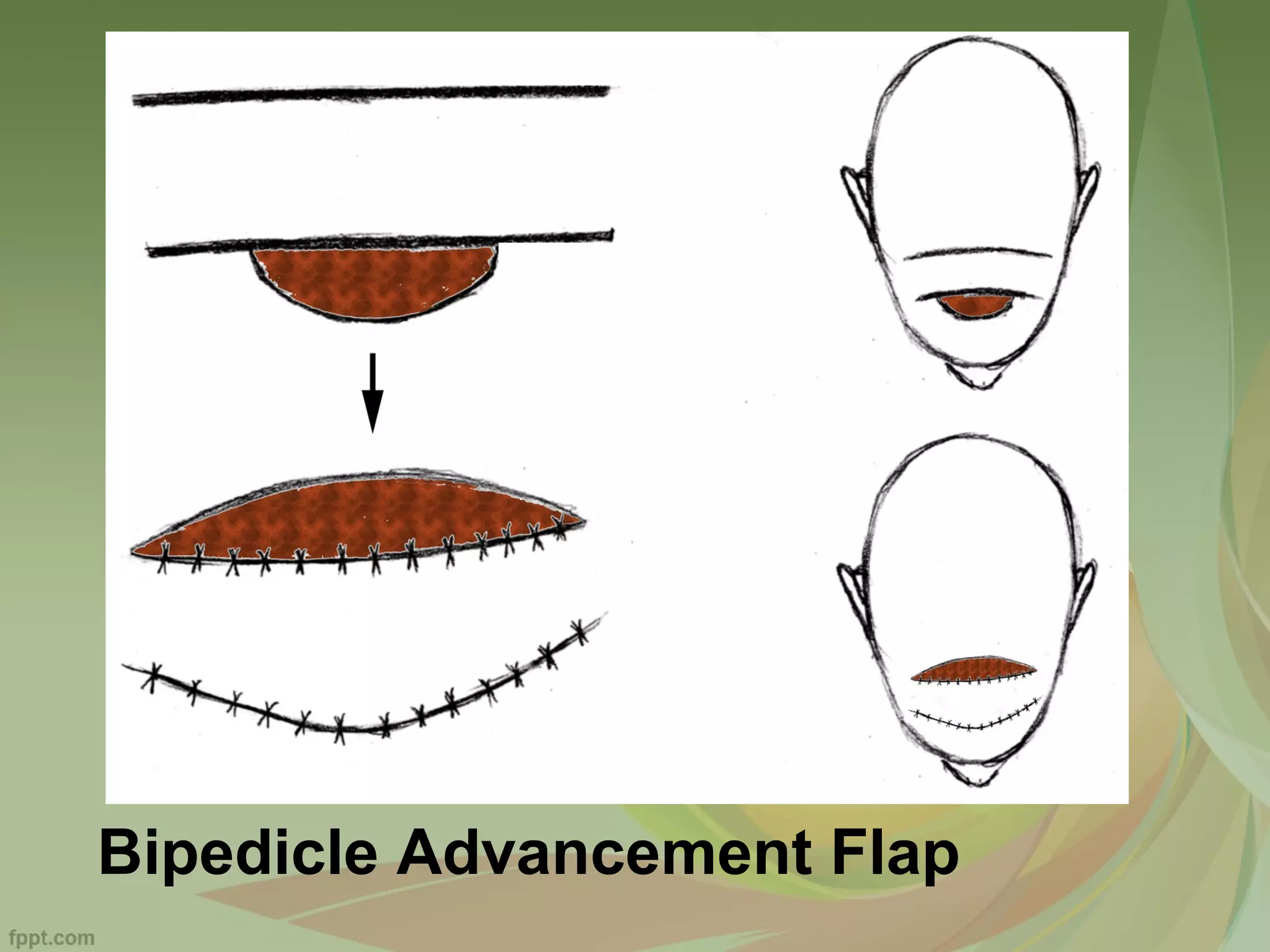
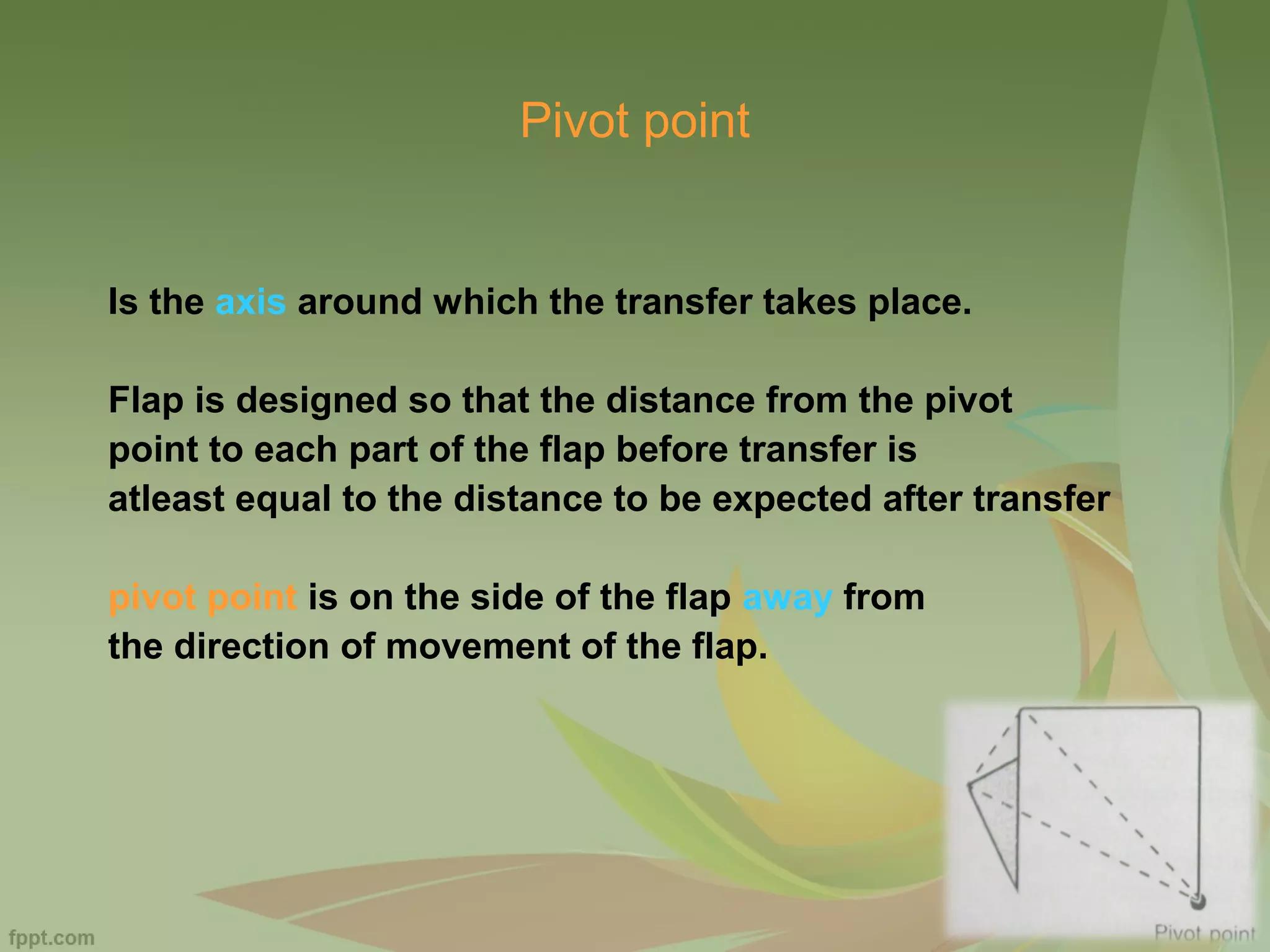
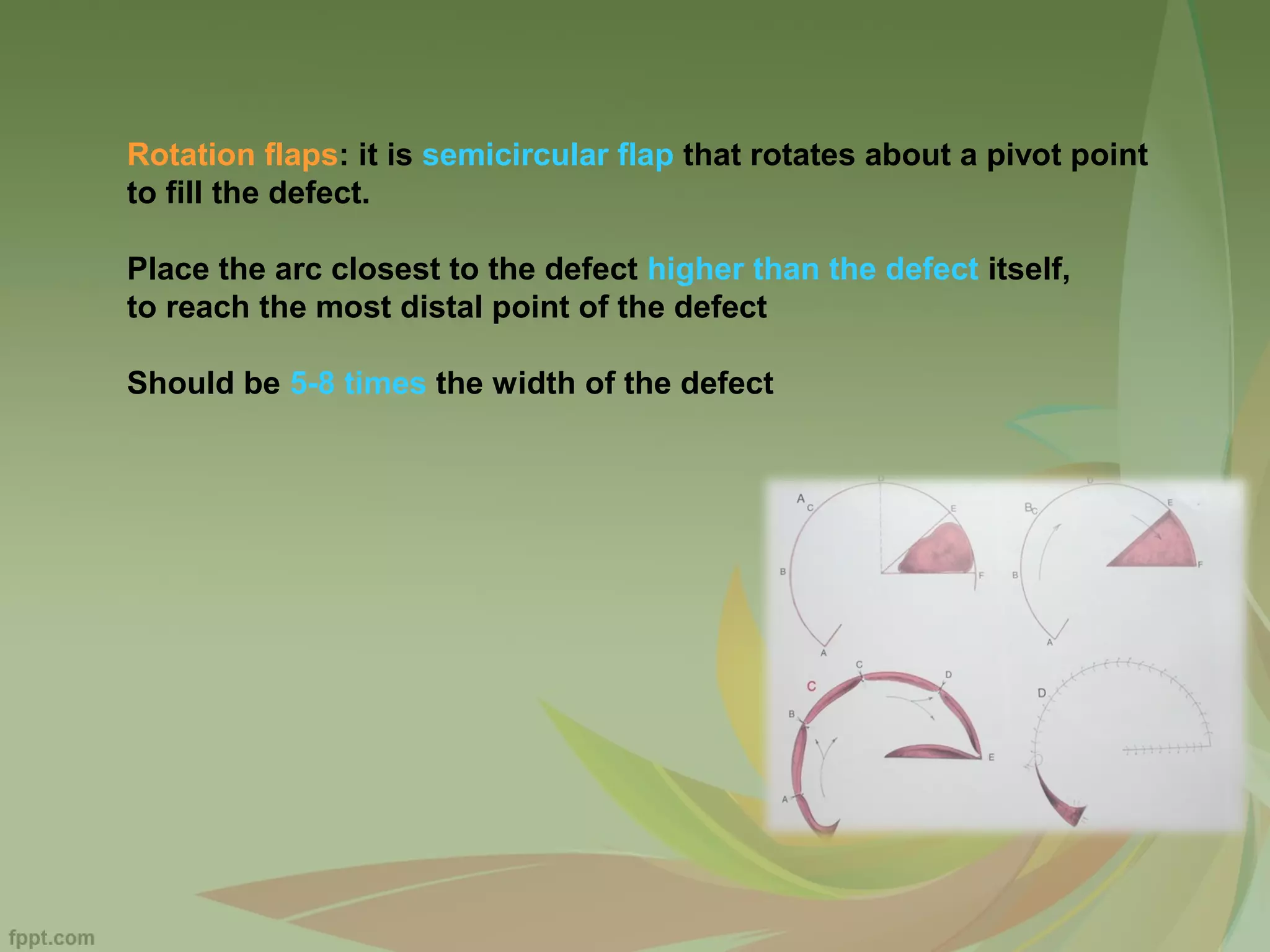
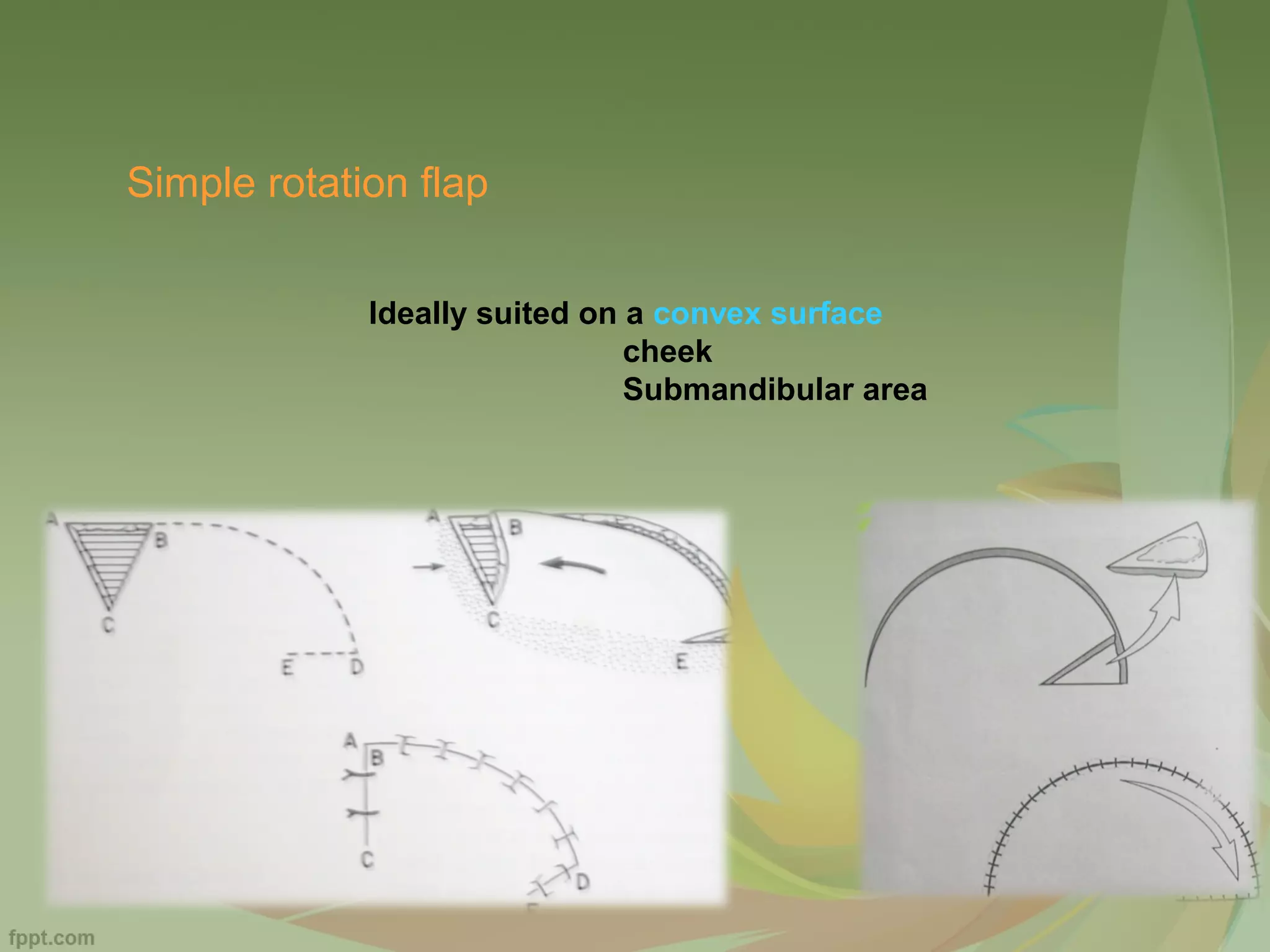
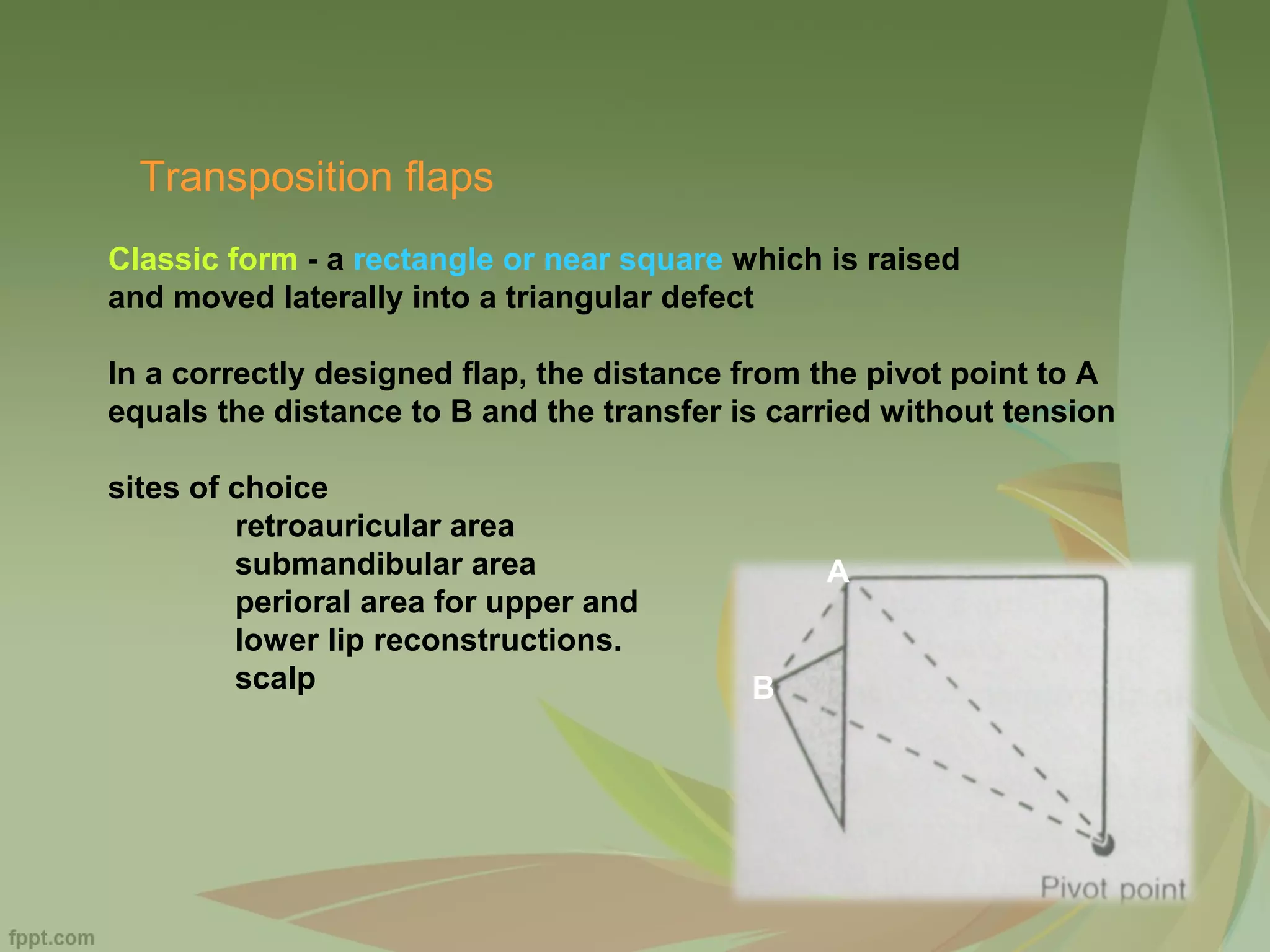
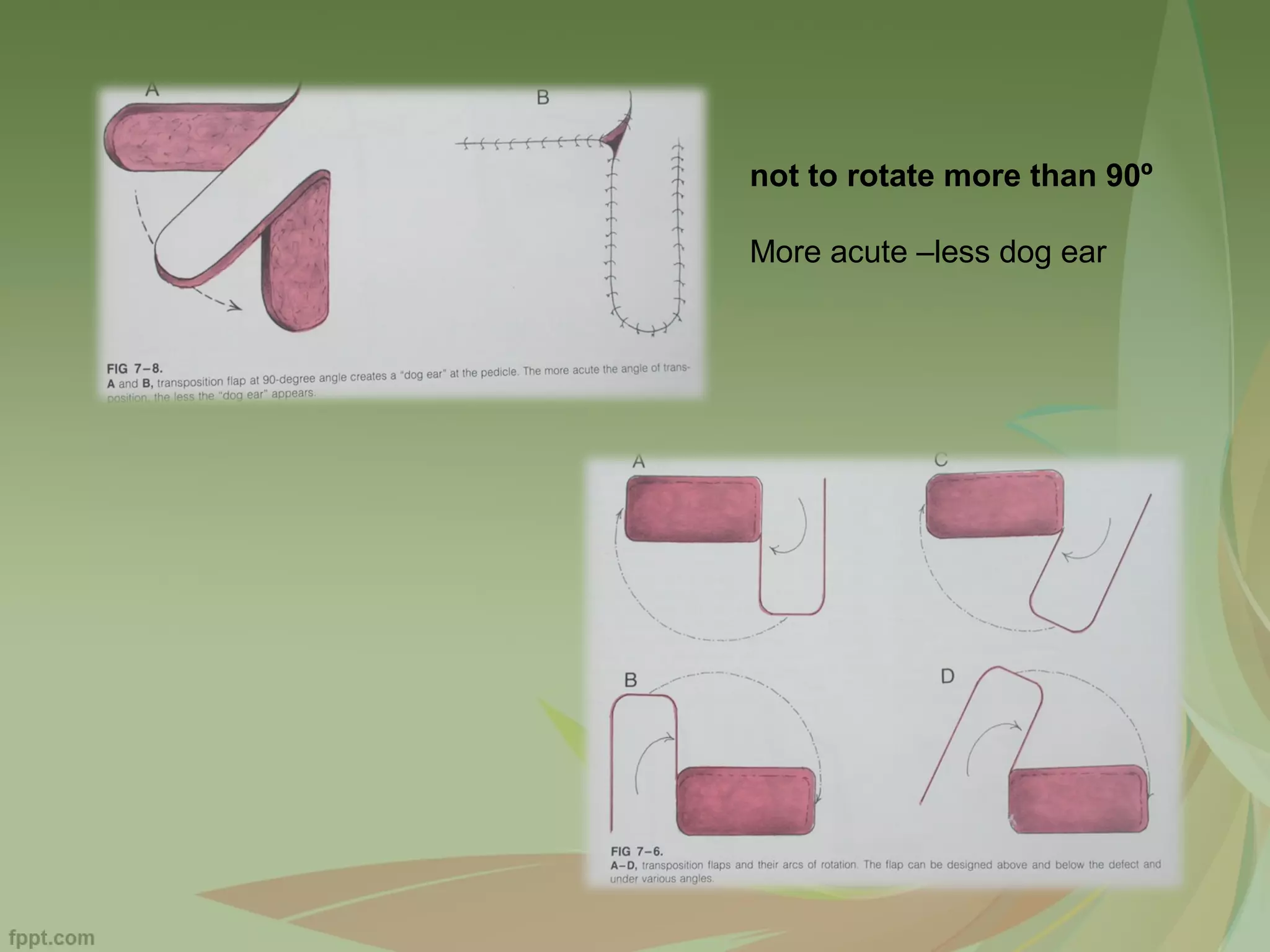
A flap is a unit of tissue transferred from one site to another while maintaining its own blood supply. Flaps are classified based on their location as local or distant. Local flaps can be random, which rely on subdermal vessels, or axial, relying on named vessels. Flaps are also classified based on their composition, such as skin, muscle, or bone flaps. When planning local flaps, goals include color and thickness match, sensory preservation, and minimal secondary defects. Common local flap techniques include advancement, rotation, and transposition flaps to close facial defects. Complications can be prevented through proper planning to avoid tension and including a flap margin.