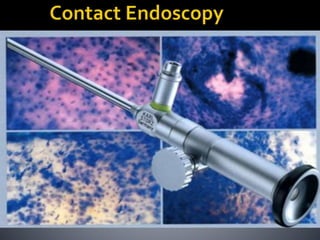
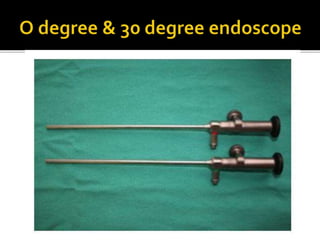
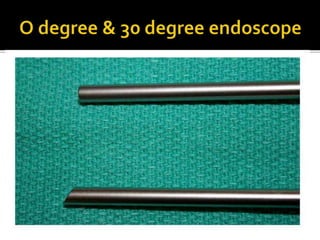
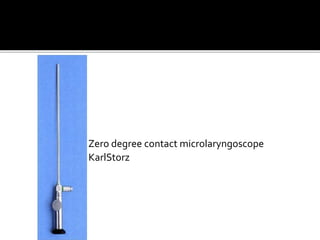
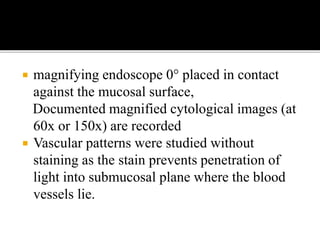
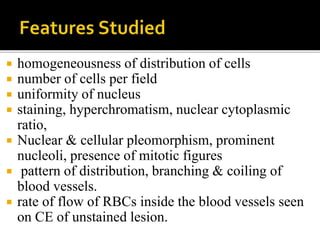
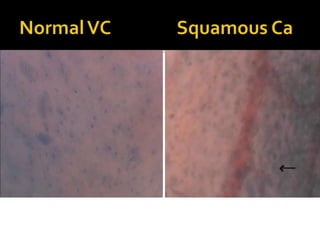
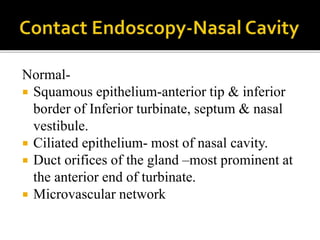
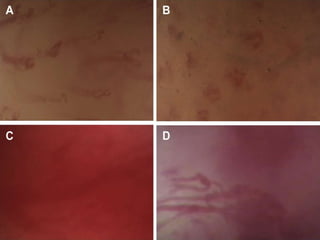
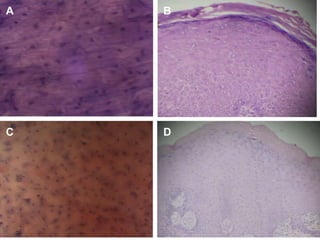
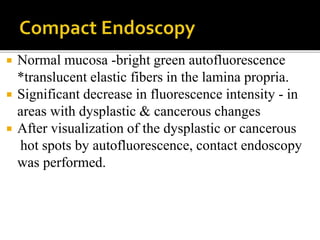
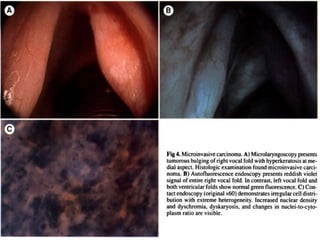
This document describes contact endoscopy (CE), a non-invasive optical technique that uses a magnifying endoscope to provide real-time visualization and examination of the cellular architecture and vascular patterns of mucosal tissues. CE allows in vivo assessment of precancerous and cancerous lesions without biopsy. Several contact endoscope models from Karl Storz are described. The document outlines CE's applications in examining various head and neck tissues and its ability to detect abnormalities. The benefits of CE include its non-invasive nature, ability to examine large areas quickly, and provision of immediate results.