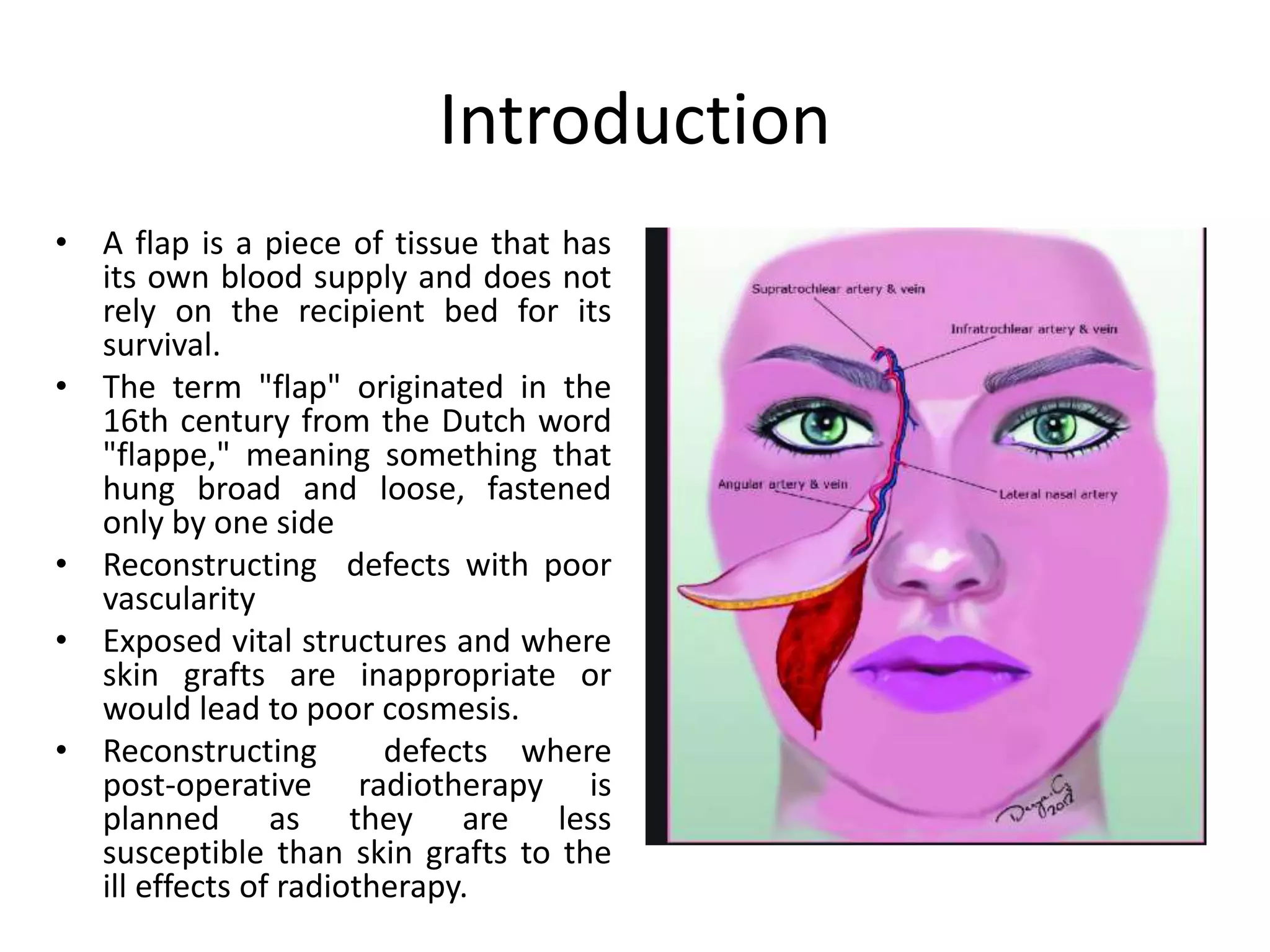
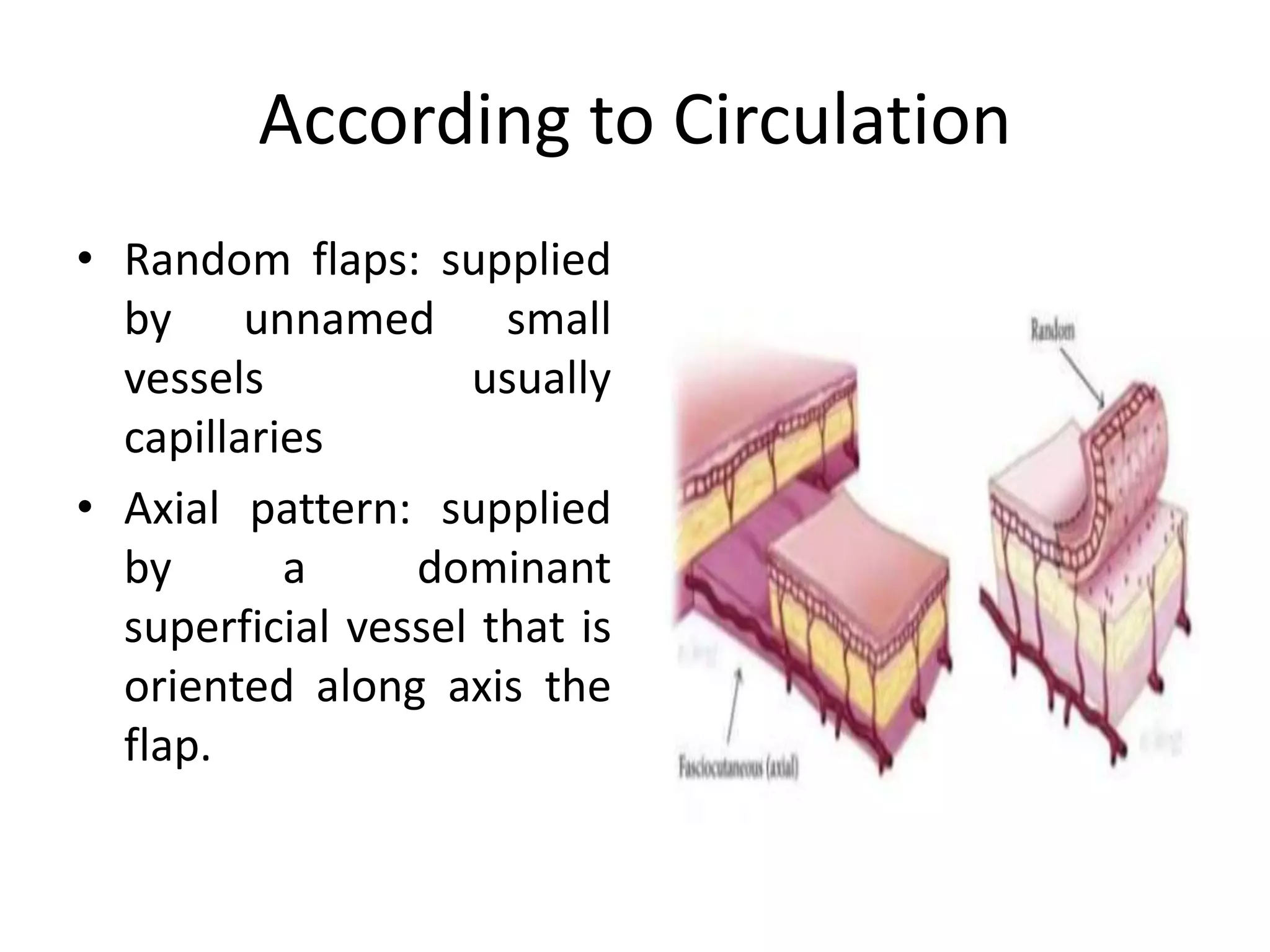
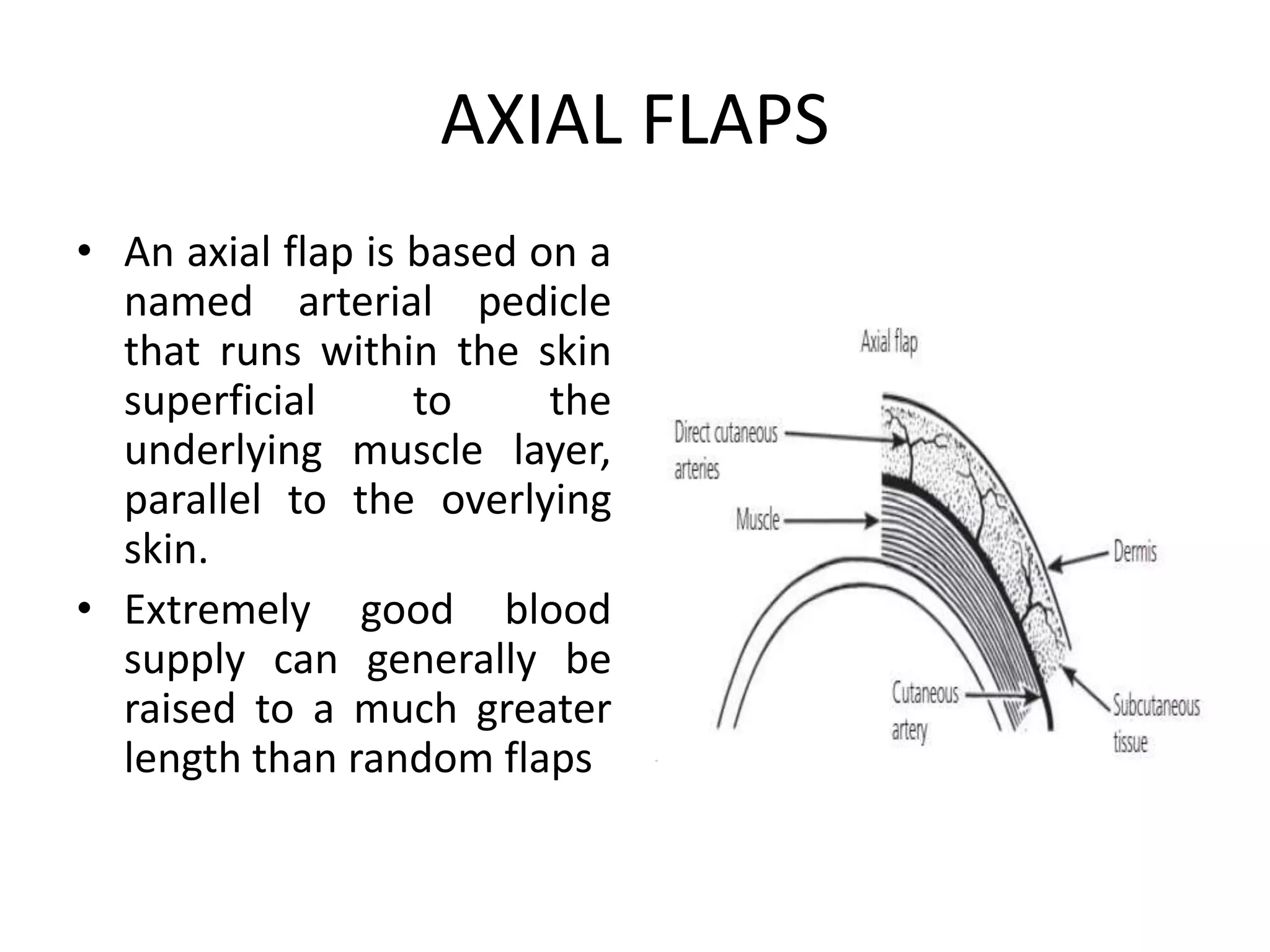
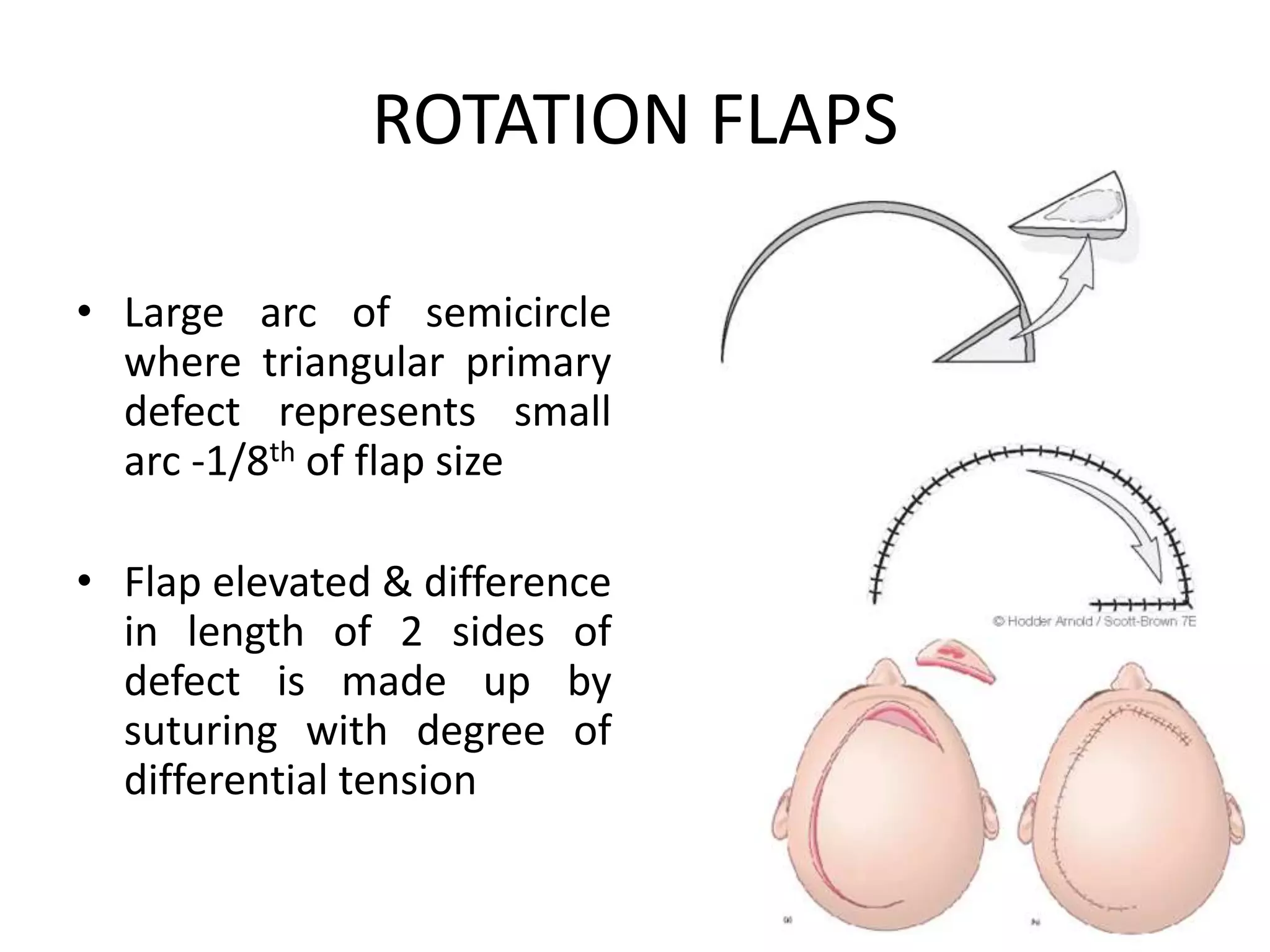
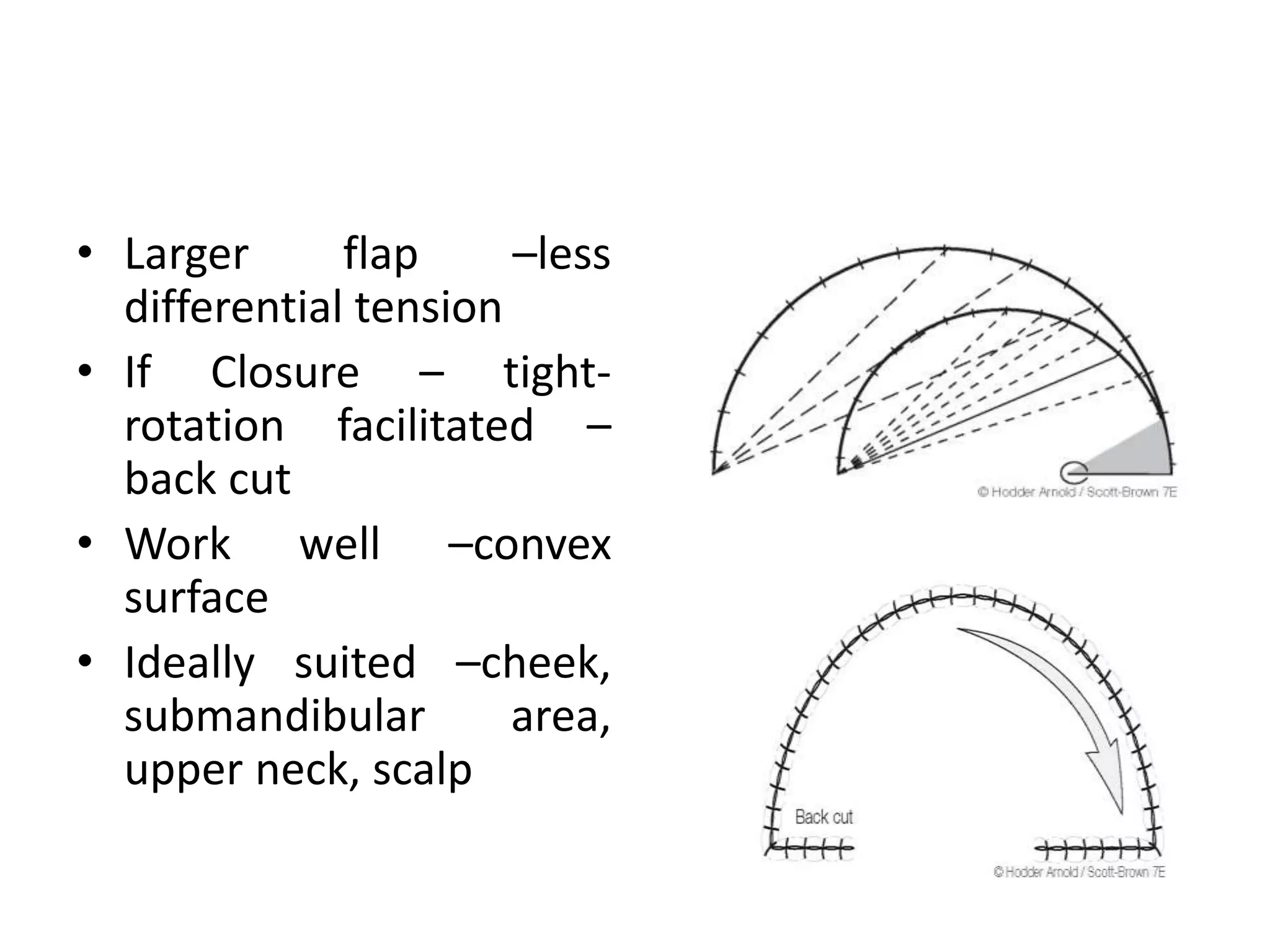
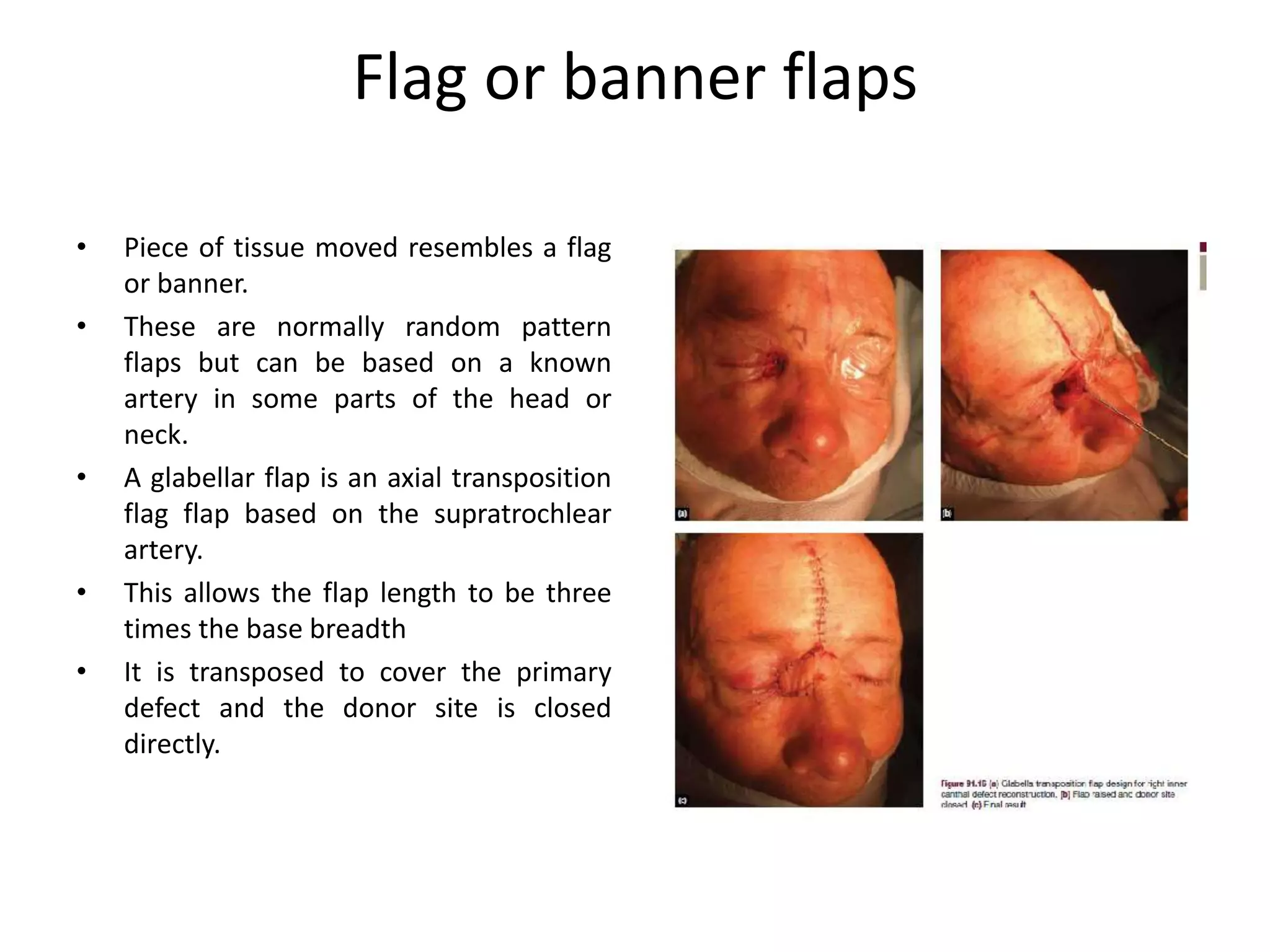
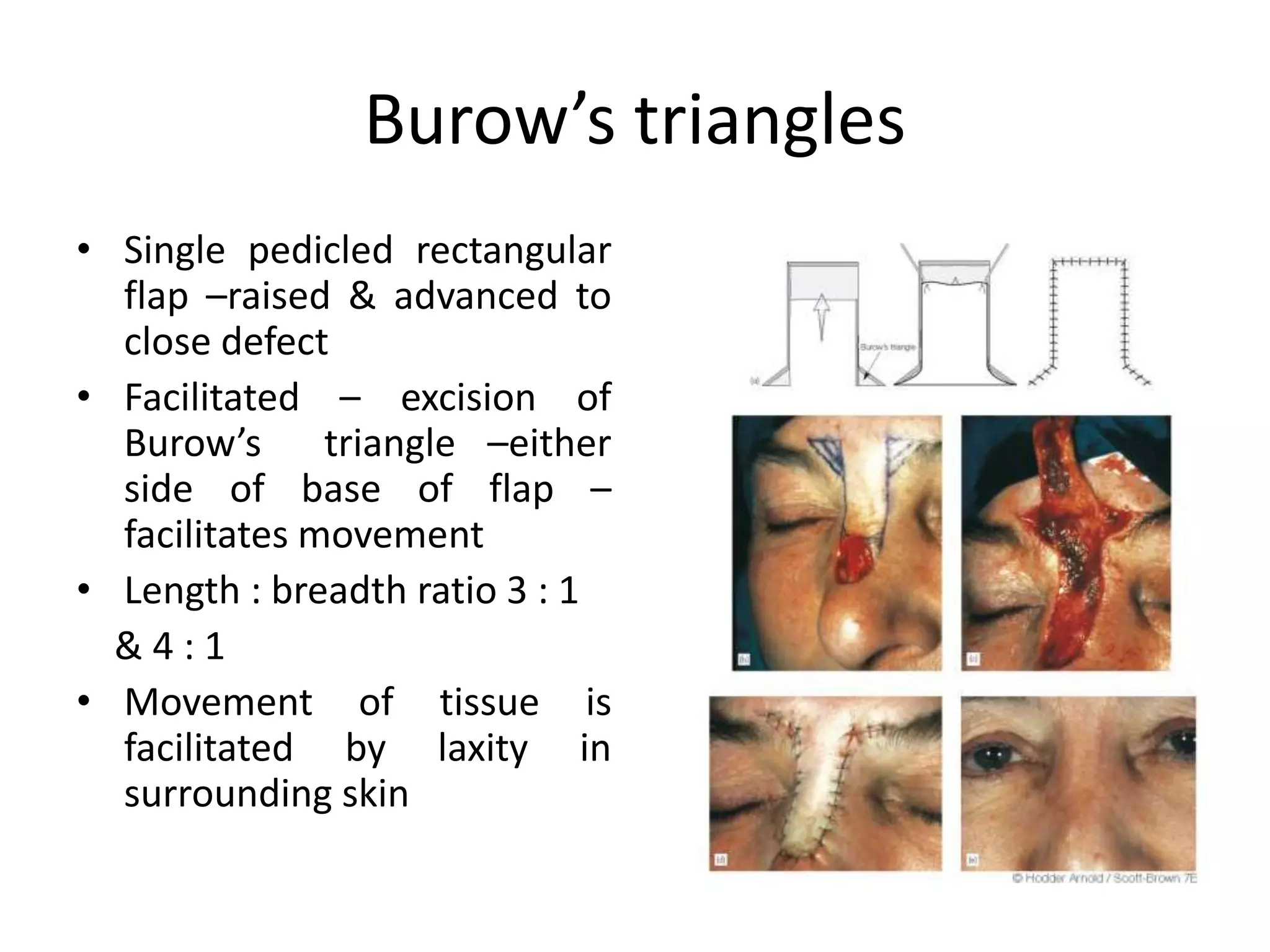
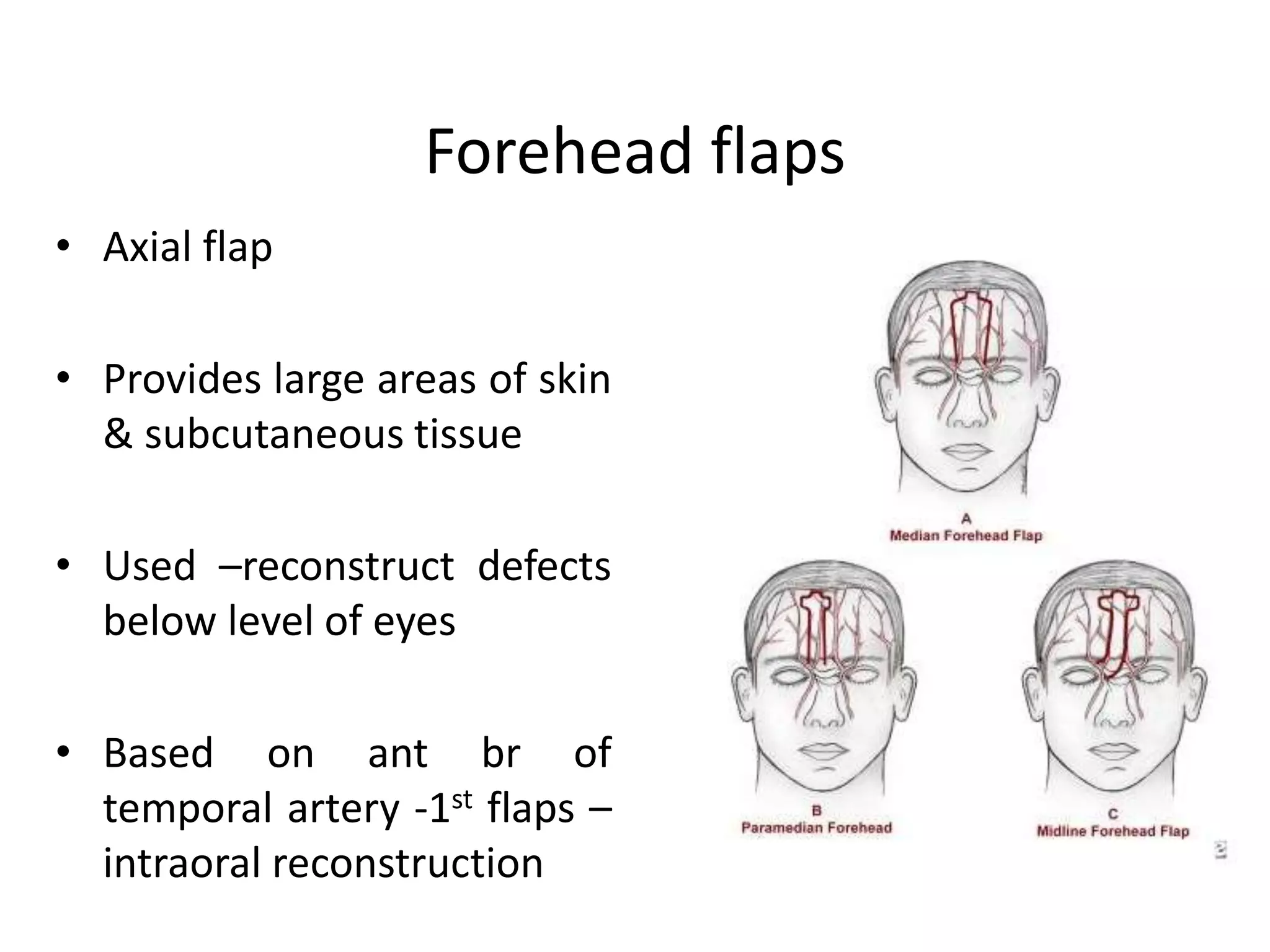
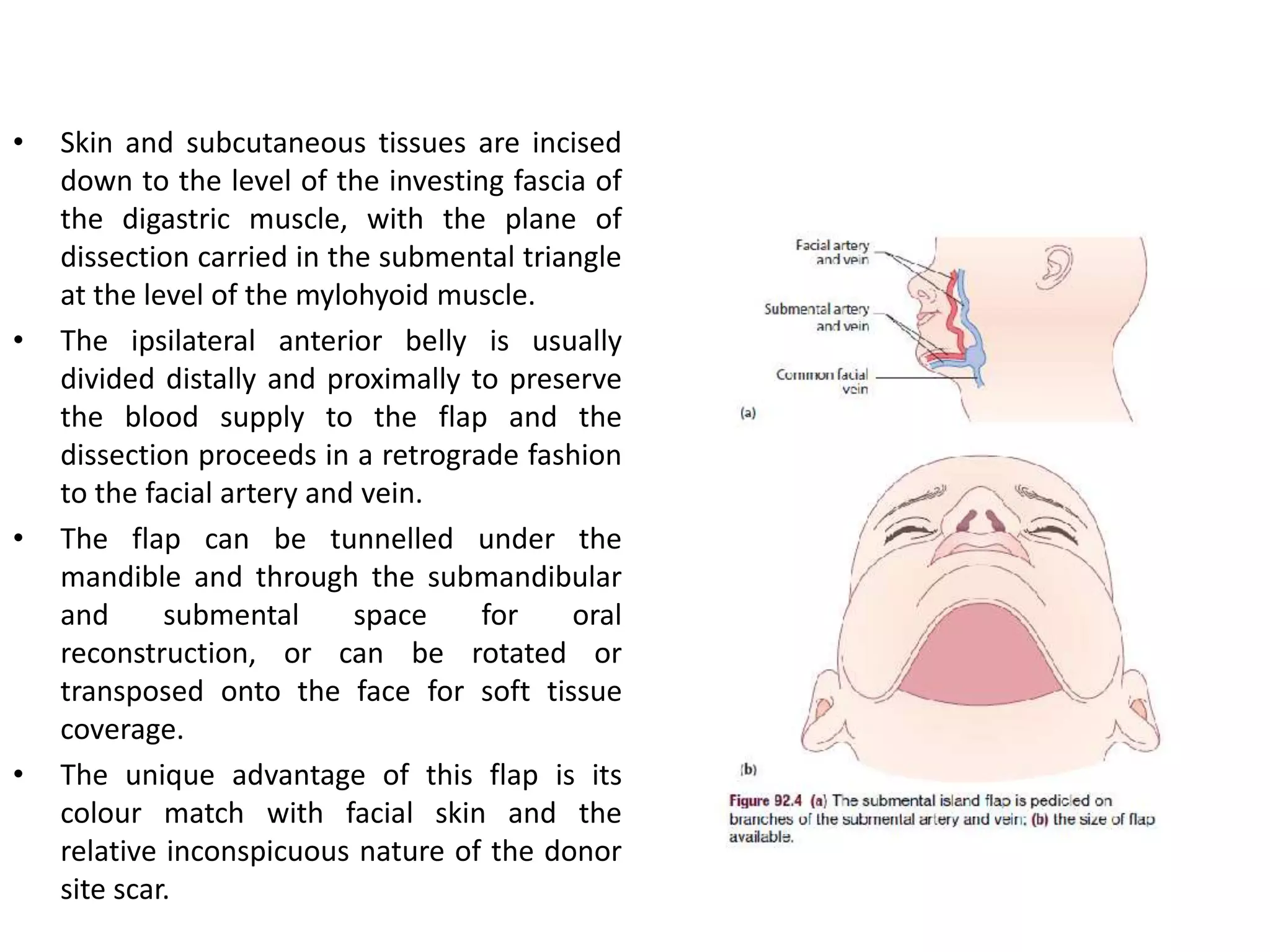
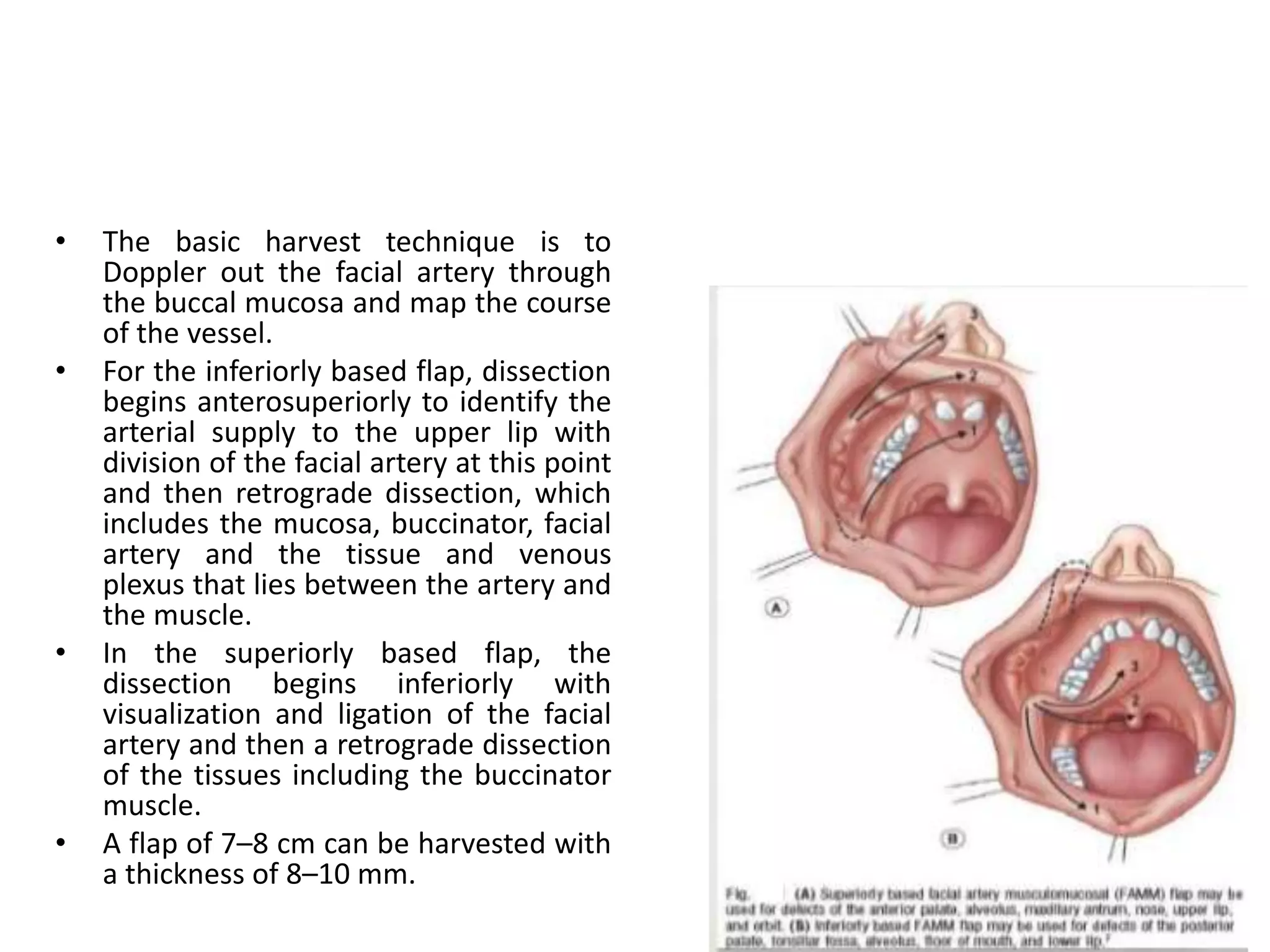
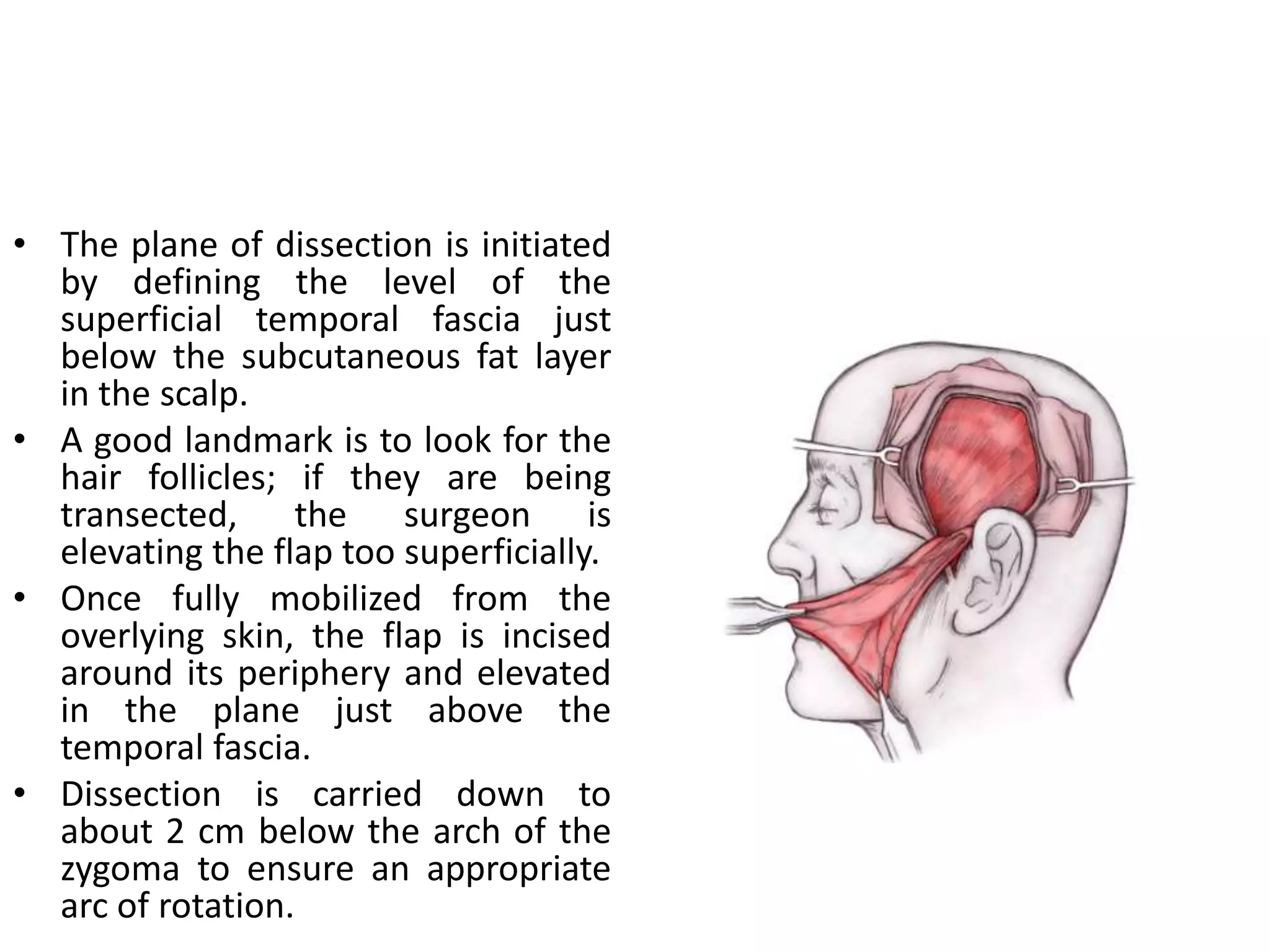
This document provides an overview of flaps used in head and neck surgery. It discusses the history of flap reconstruction from 600 BC to present day. It then covers general concepts in reconstruction including the reconstruction ladder. The rest of the document classifies and describes various types of flaps used in head and neck reconstruction including local, regional, distant, and free flaps. It discusses flap classification based on circulation, contiguity, composition, and contour. It provides details on specific flaps such as forehead, nasolabial, submental island, facial artery myomucosal, temporoparietal fascial, and deltopectoral flaps.