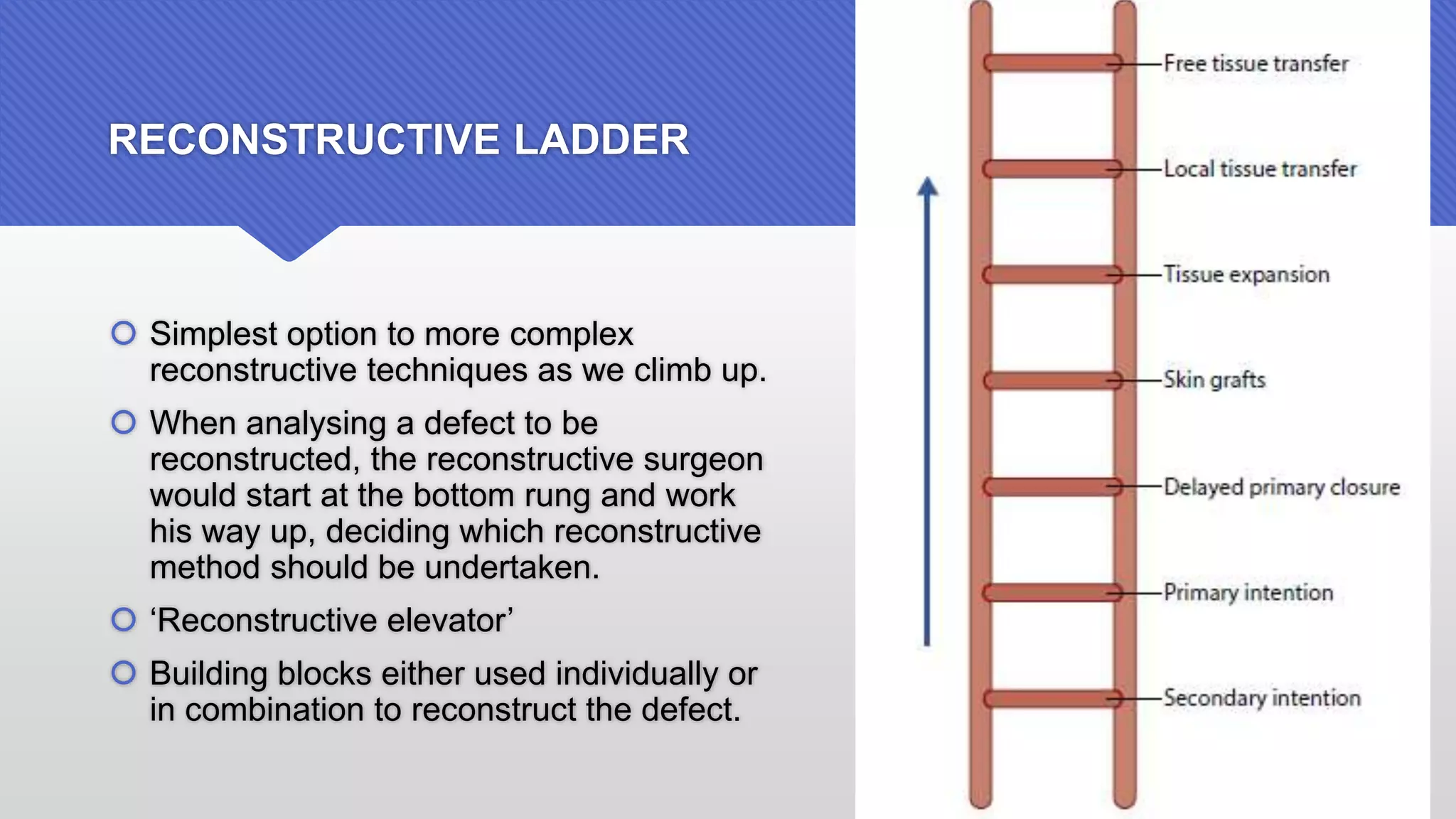
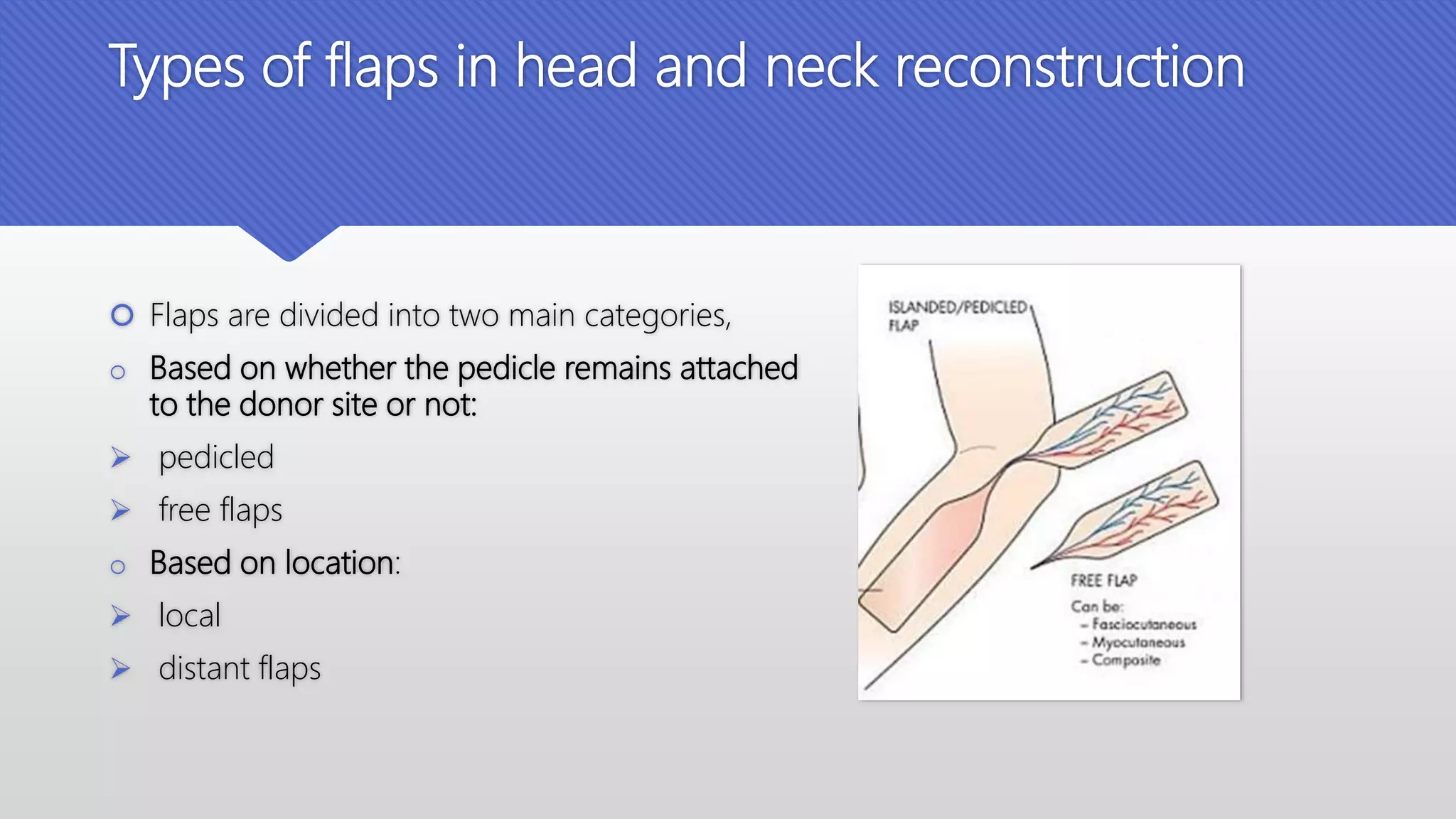
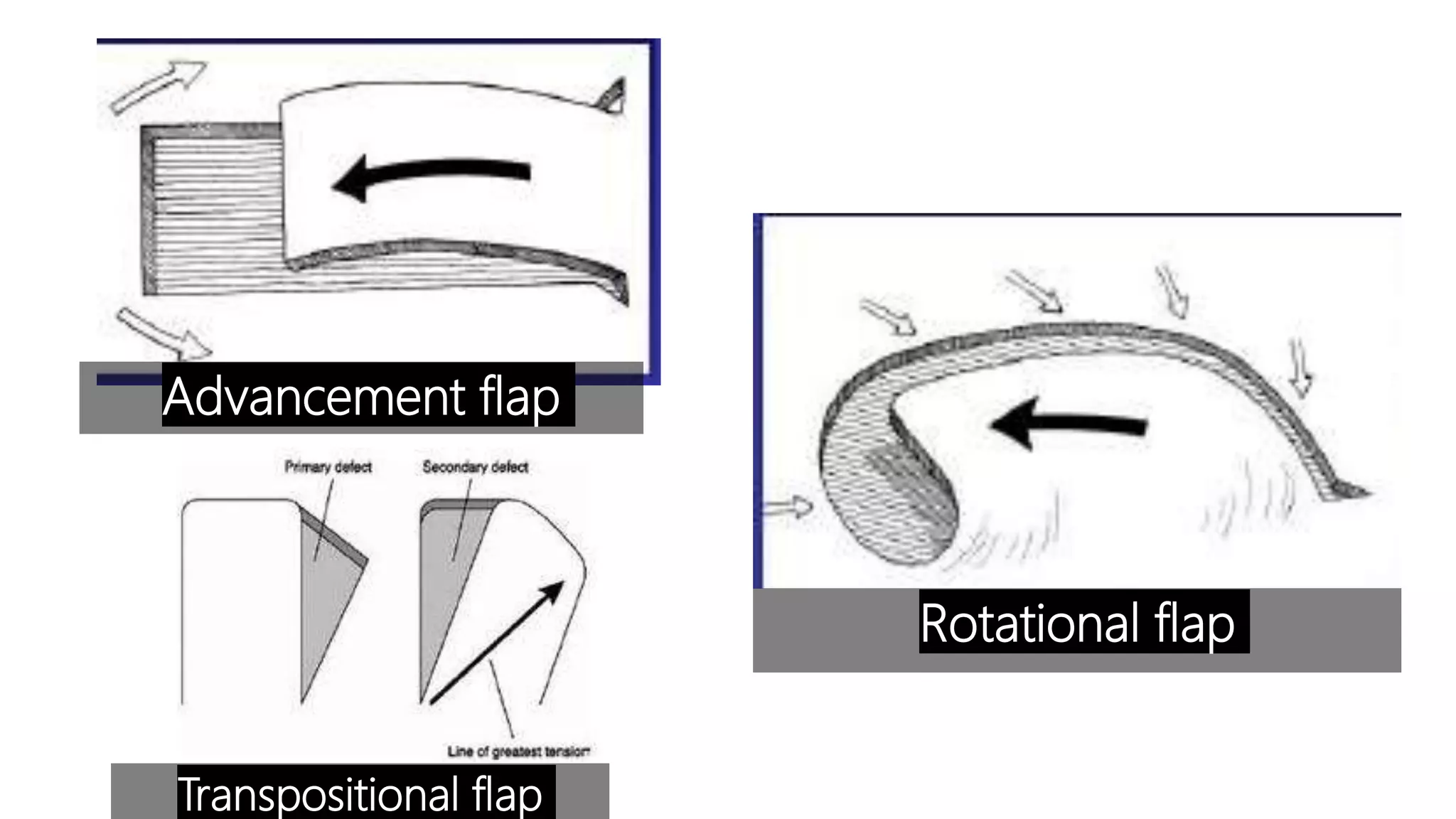
This document provides an overview of grafts and flaps used in head and neck reconstruction. It discusses the history of reconstructive surgery dating back 5000 years. Grafts are pieces of tissue without their own blood supply that rely on the recipient bed, while flaps have their own blood supply. Flaps are useful for larger defects and where radiation is planned. The document describes various local and distant pedicled and free flaps used to reconstruct different areas of the head and neck, including the forearm flap, rectus abdominis flap, and anterolateral thigh flap. Factors affecting graft and flap survival include adequate blood supply, wound conditions, and patient comorbidities. The key principles of reconstruction are to