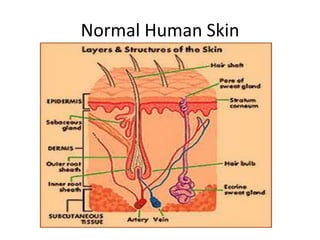
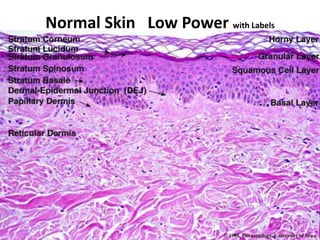
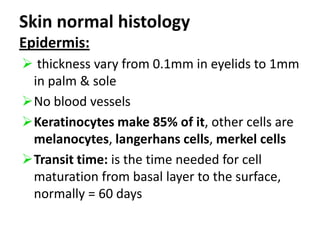
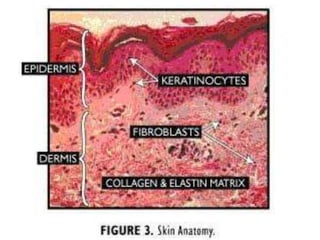
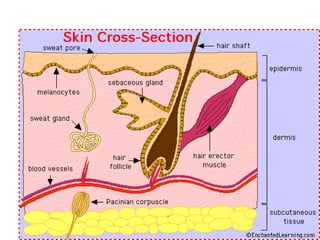
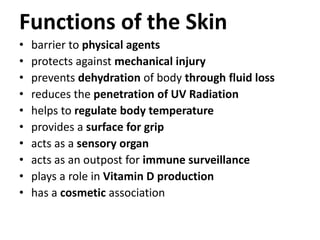
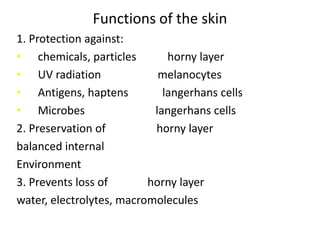
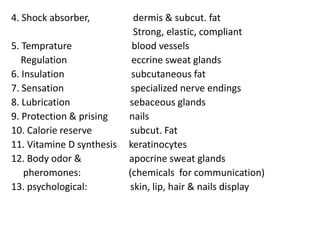
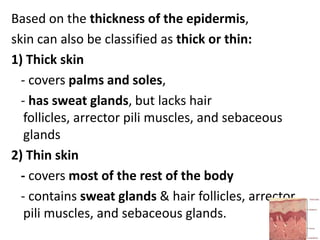
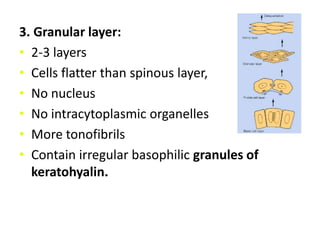
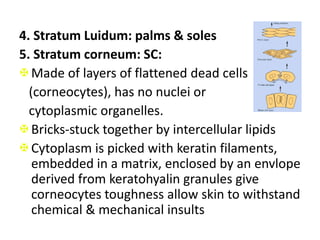
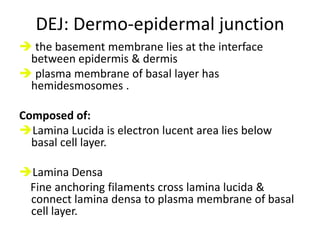
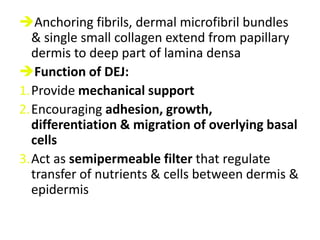
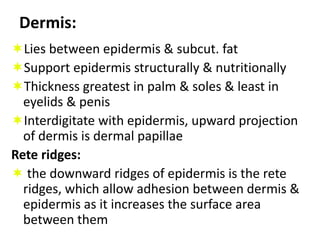
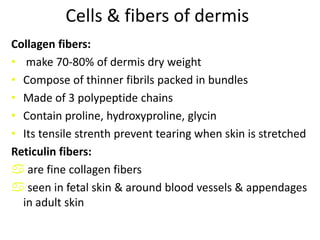
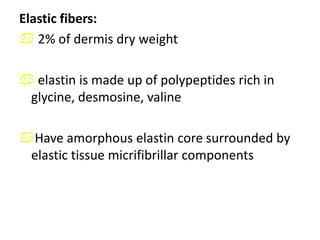
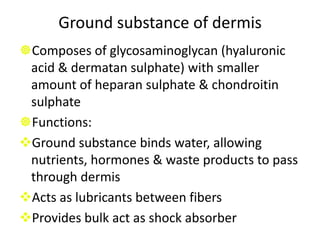
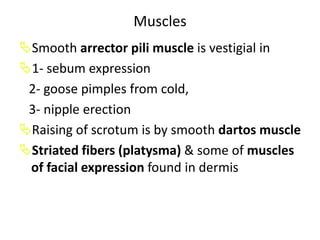
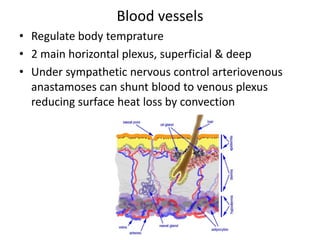
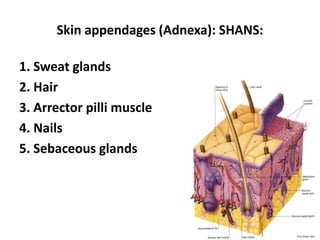
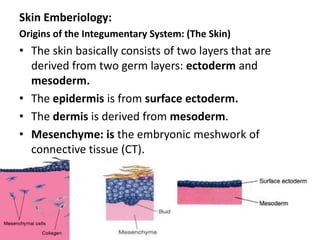
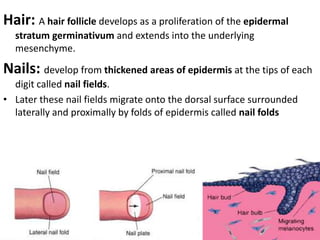
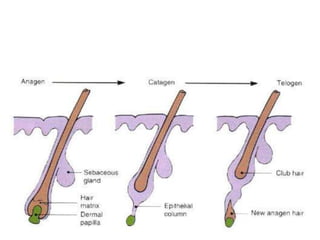
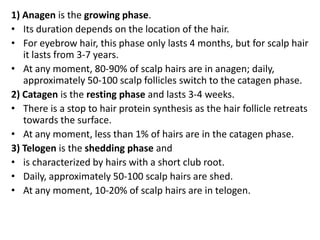
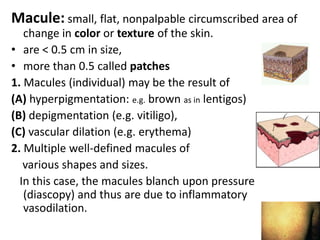
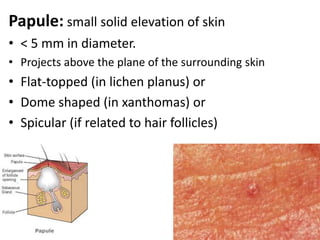
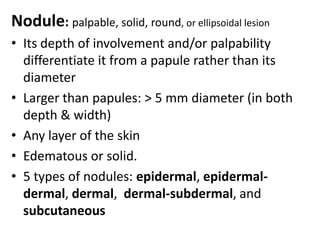
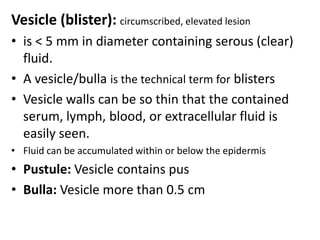
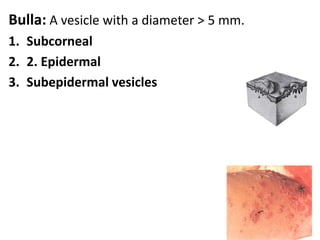
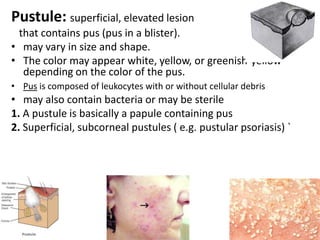
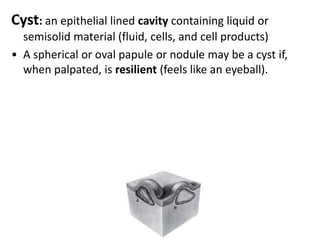
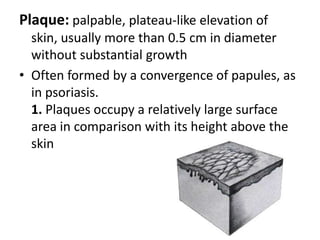
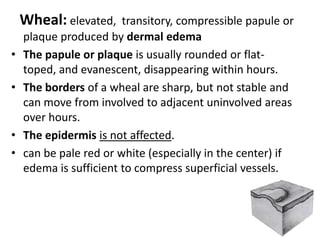
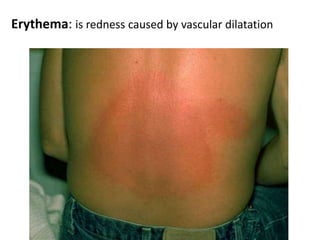
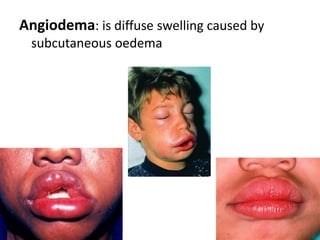
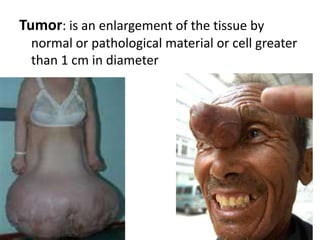
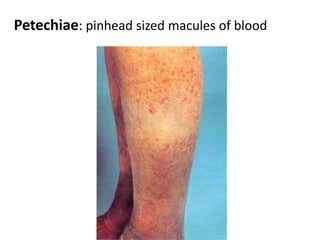
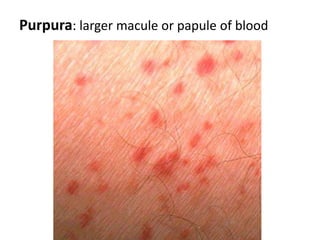
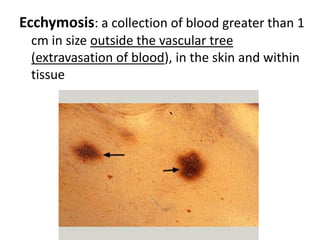
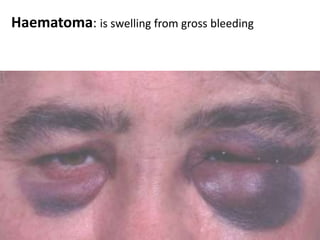
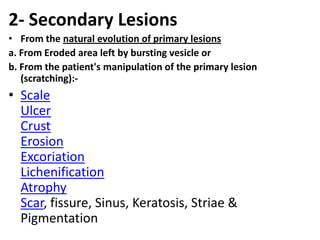
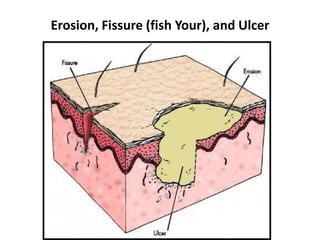
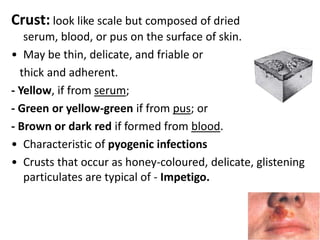
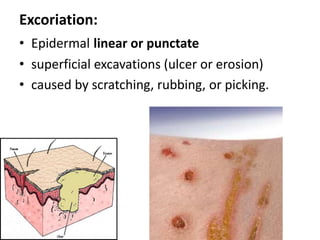
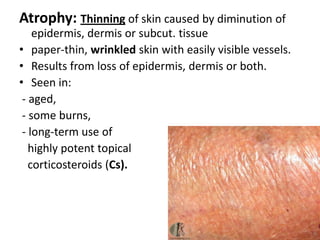
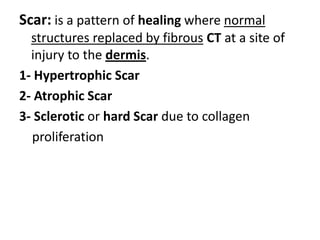
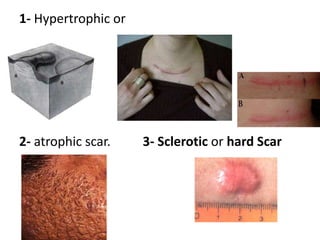
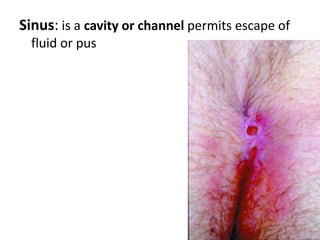
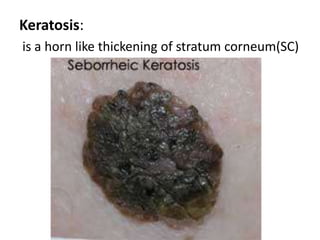
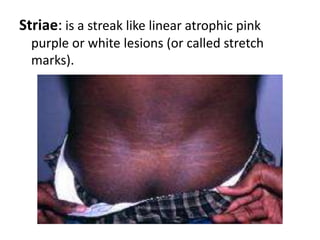
The document provides information about human skin anatomy, organization, histology, function and diagnosis. It discusses the key components and layers of the skin including the epidermis, dermis and skin appendages. The epidermis is composed of the basal, spinous, granular and stratum corneum layers. The dermis contains collagen, elastic and ground substance fibers. The skin has important protective, sensory and temperature regulating functions. Common skin lesions and their characteristics are also defined.