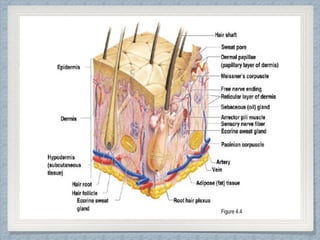
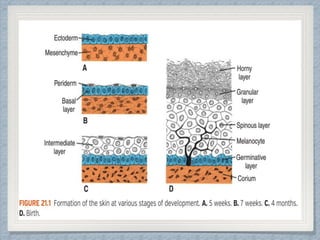
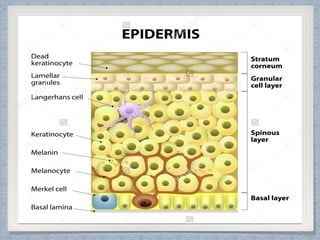
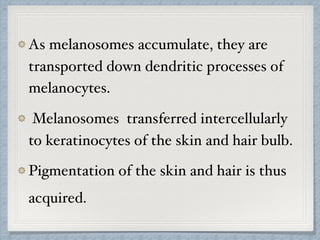
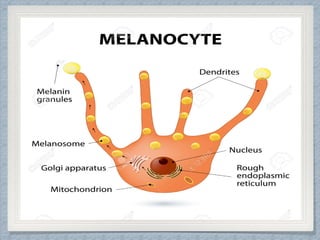
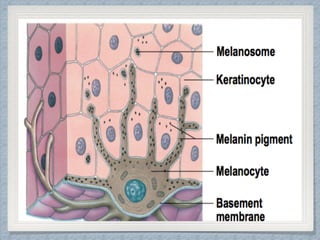
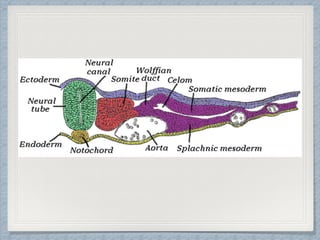
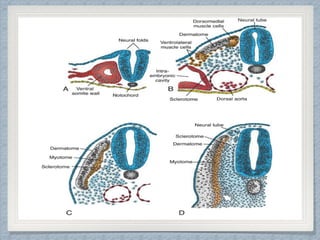
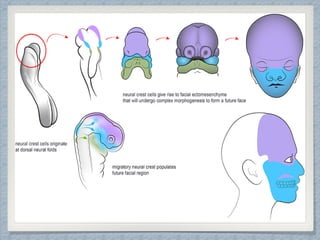
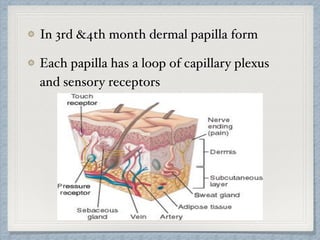
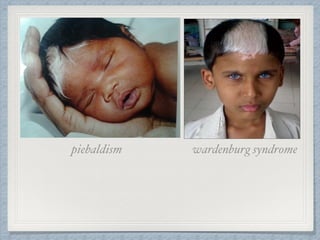
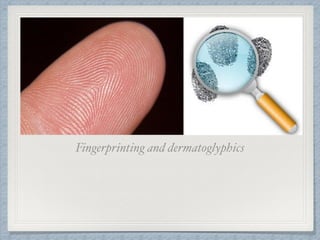
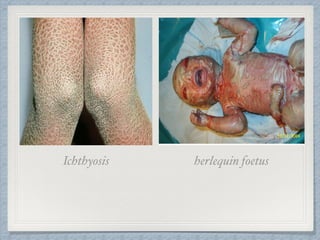
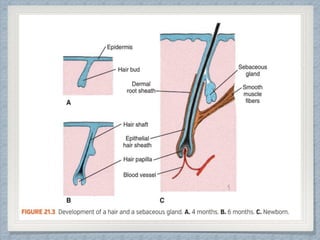
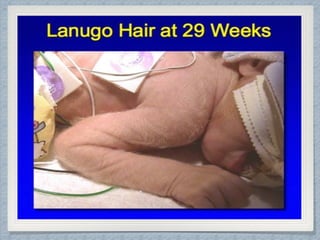
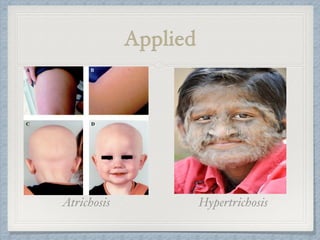
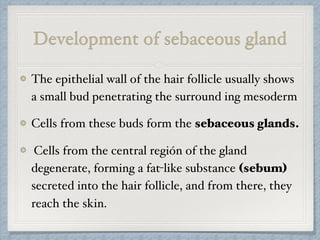
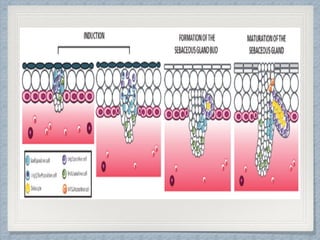
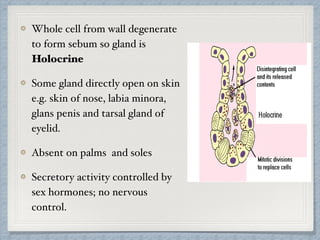
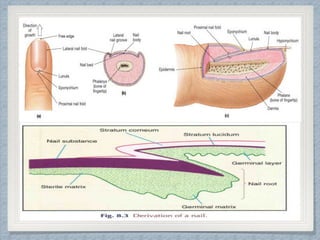
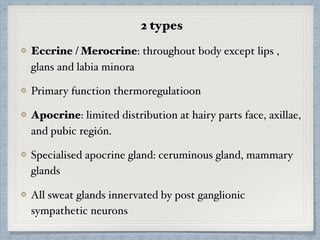
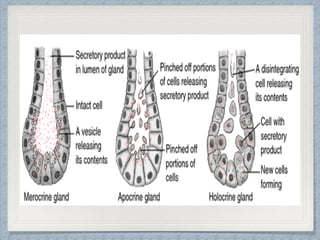
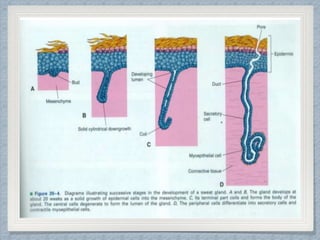
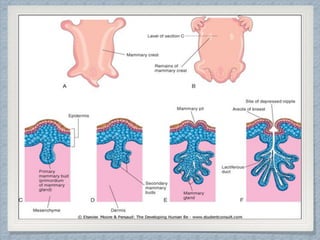
The document summarizes the development of the integumentary system. It states that the skin and its derivatives like hair, nails, sweat glands, and mammary glands develop from both the surface ectoderm and underlying mesoderm. It describes the development process of each structure in detail. For example, it notes that the epidermis forms from the surface ectoderm and develops four layers by the end of the fourth month, while the dermis develops from the mesoderm and forms dermal papillae containing blood vessels and sensory receptors in the third and fourth months. The document also lists several pigmentary, hair, and gland disorders as examples of conditions related to integumentary system development.