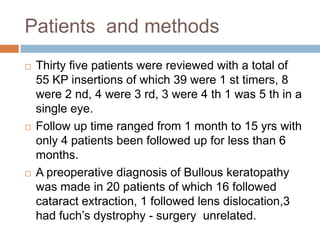
This document reviews a study of 55 keratoprosthesis insertions in 35 patients over periods ranging from 1 month to 15 years. Keratoprosthesis is a surgical procedure that replaces a severely damaged cornea with an artificial cornea to restore vision. There are two main types - Type 1 is a collar button shaped device that perforates the cornea, while Type 2 is a through-the-lid design with an anterior nub to penetrate a tarsorrhaphy. Indications for each type are described. Complications can include rejection, infections, and extrusion. The aim of the study was to review visual outcomes, retention time, and complications of keratoprosthesis surgery.
















![Proble
ms
Need for atleast two lengthy surgeries
Need for oral surgery
[minimum tooth size & good dental health]
Cosmetic result unacceptable
[tooth loss, protuding eye, prosthetic shell help]](https://image.slidesharecdn.com/keratoprosthesis-140104063259-phpapp01/85/Keratoprosthesis-20-320.jpg)