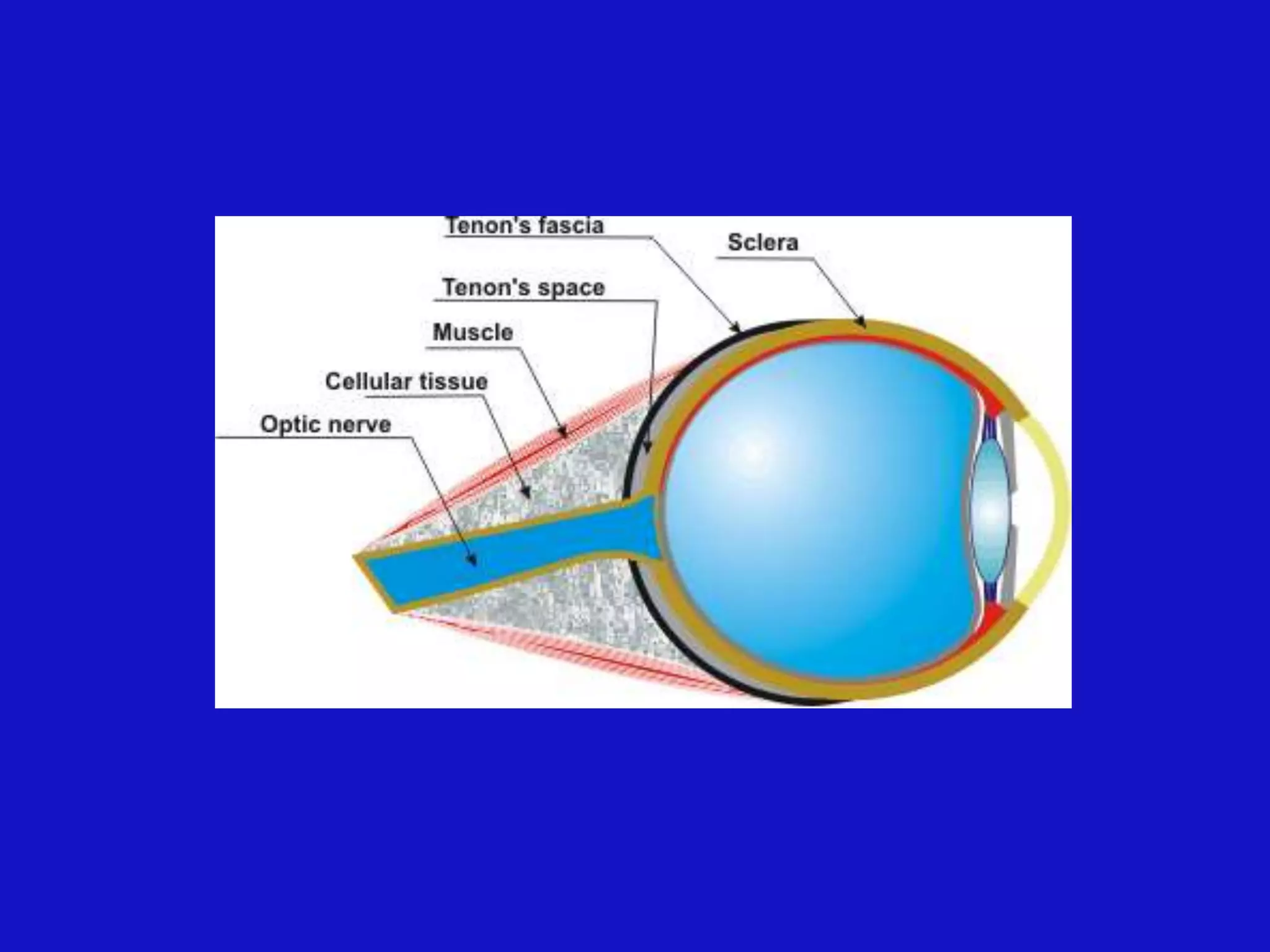
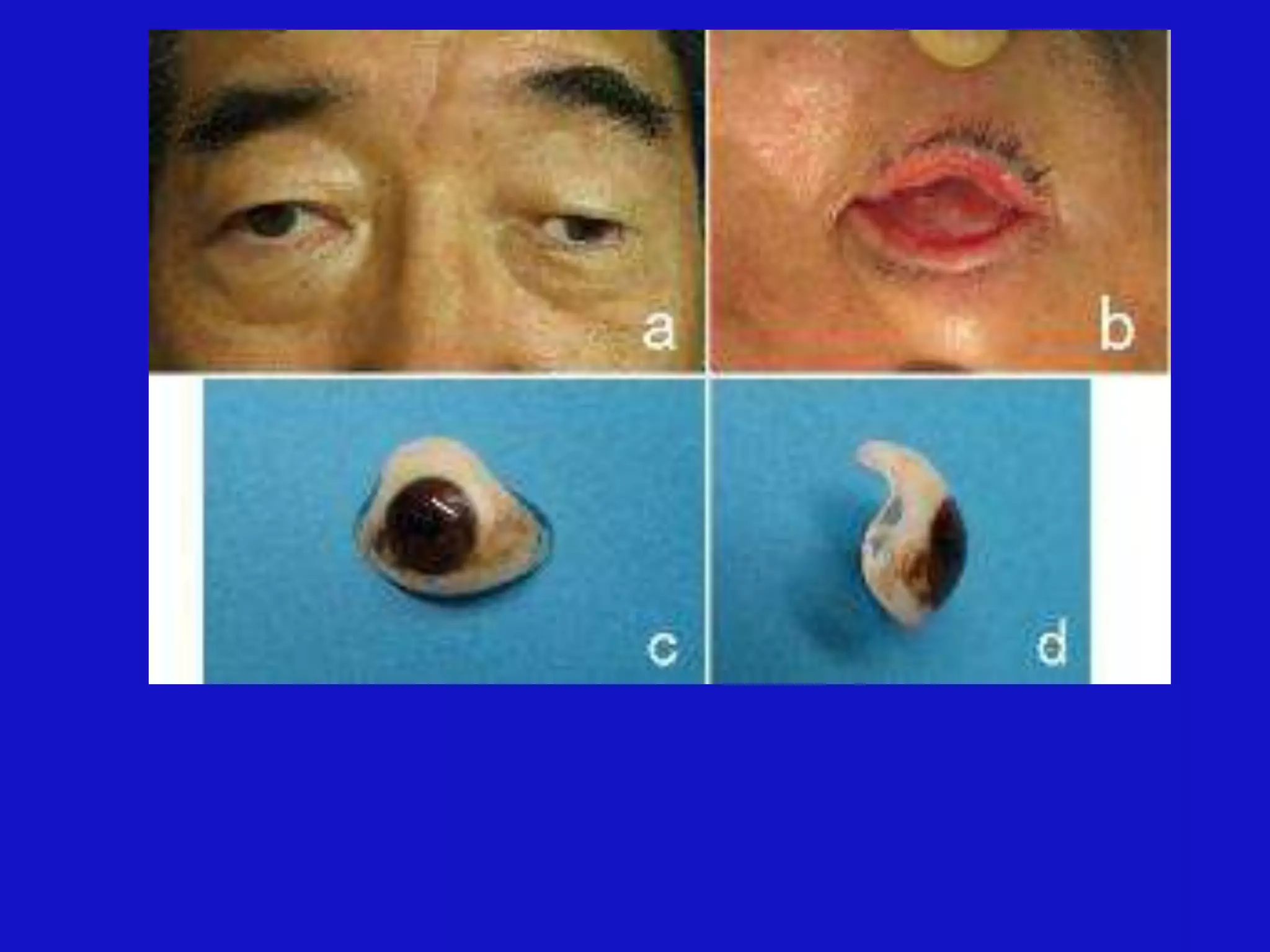
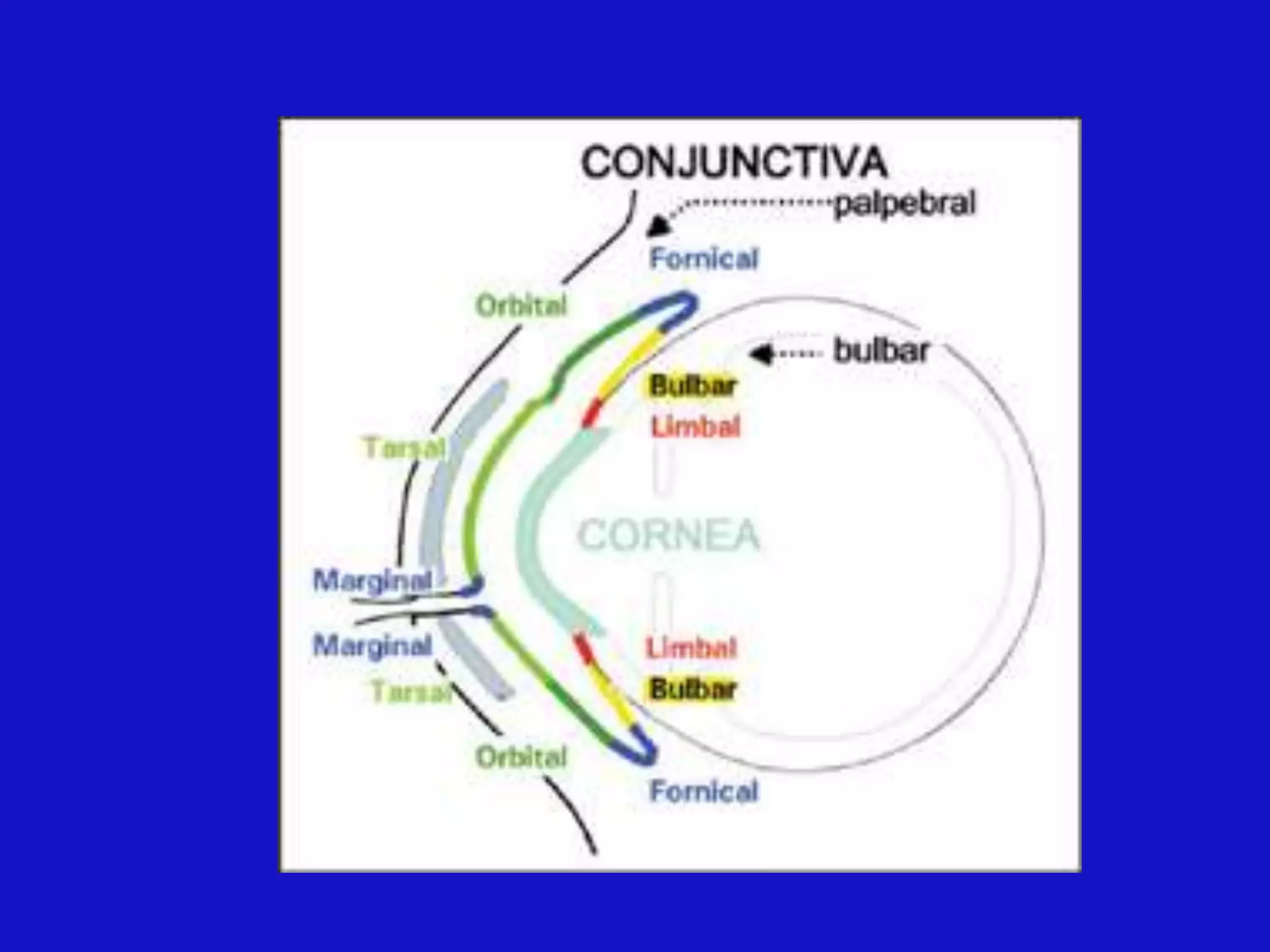
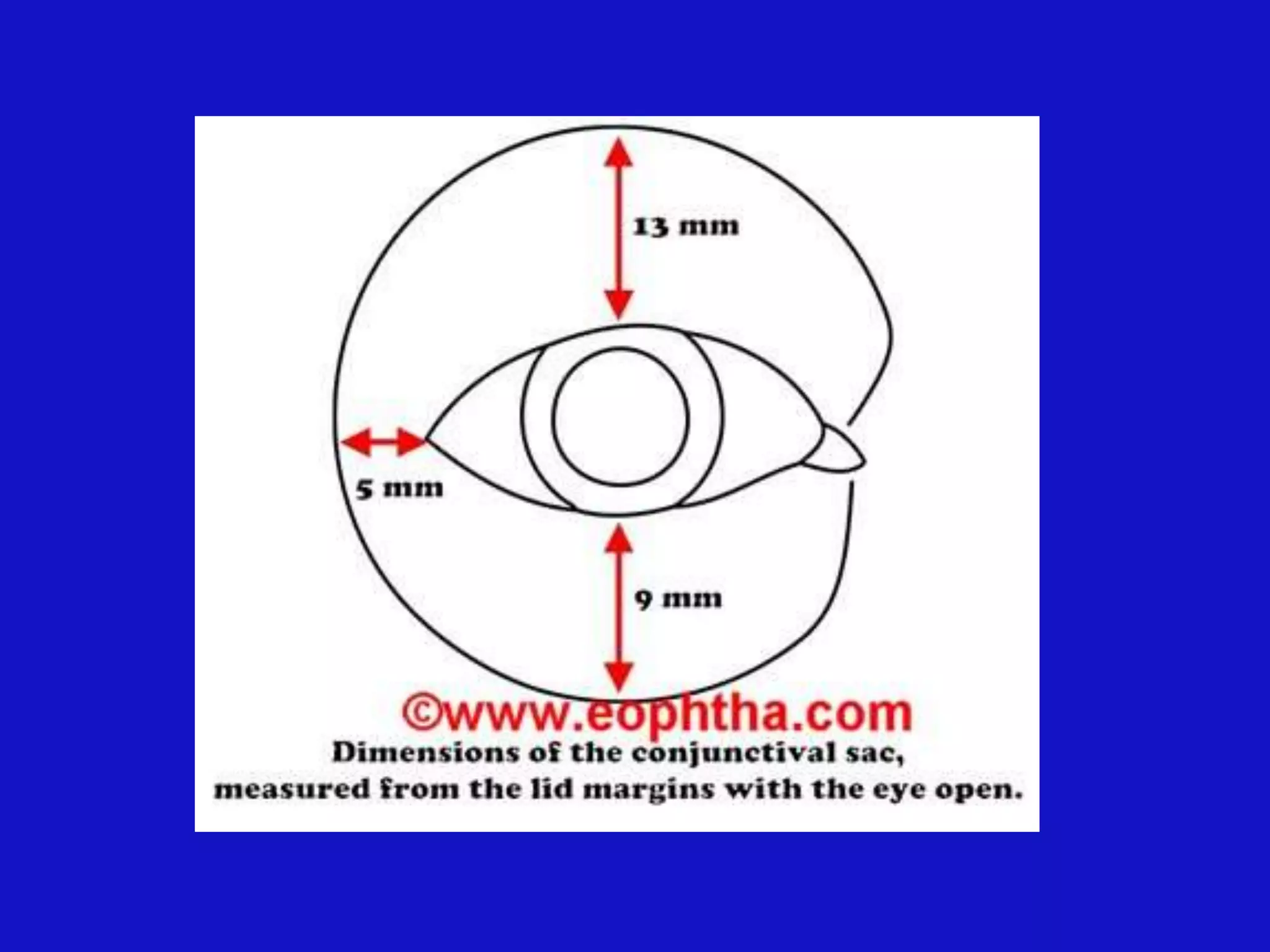
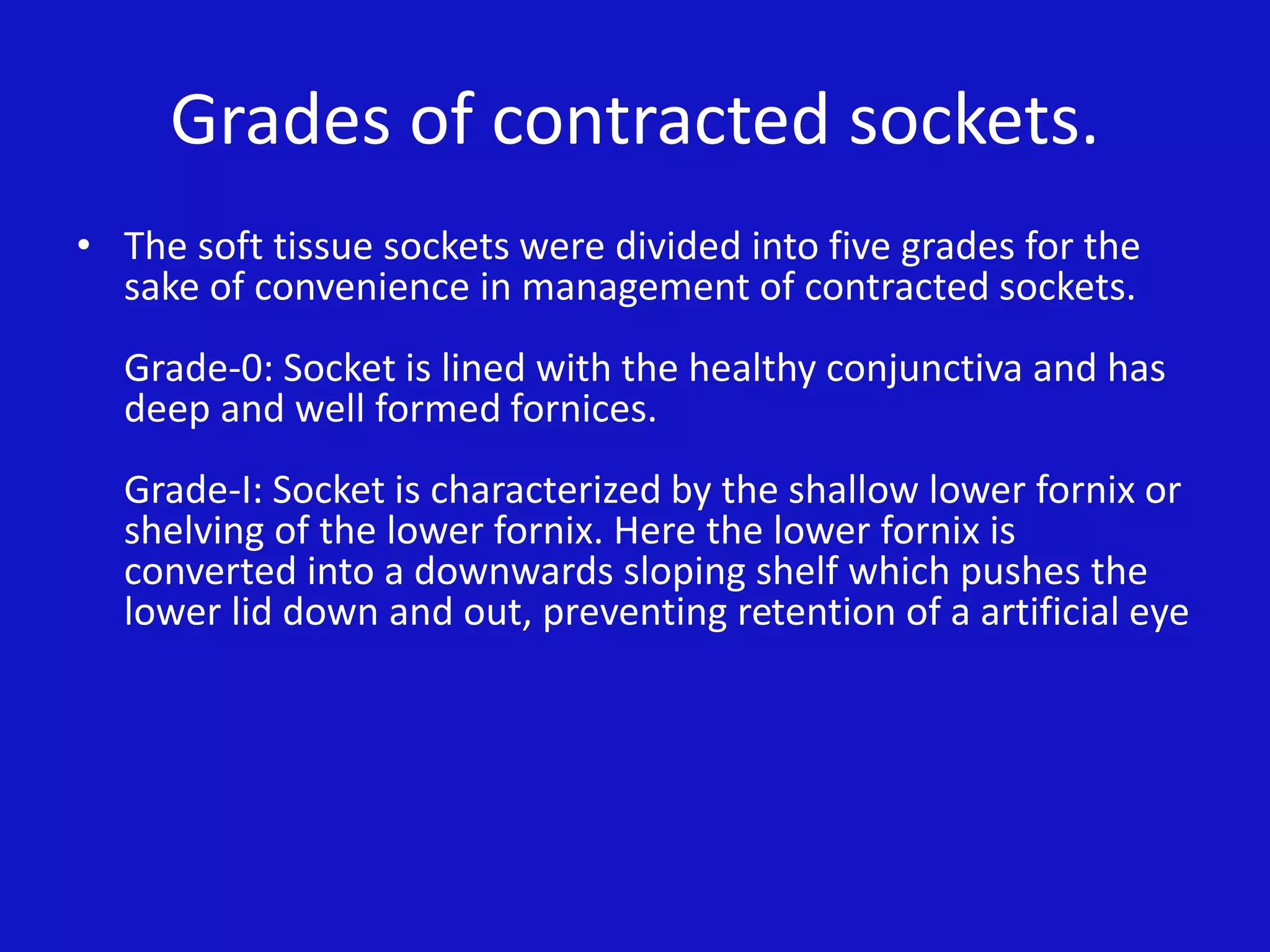
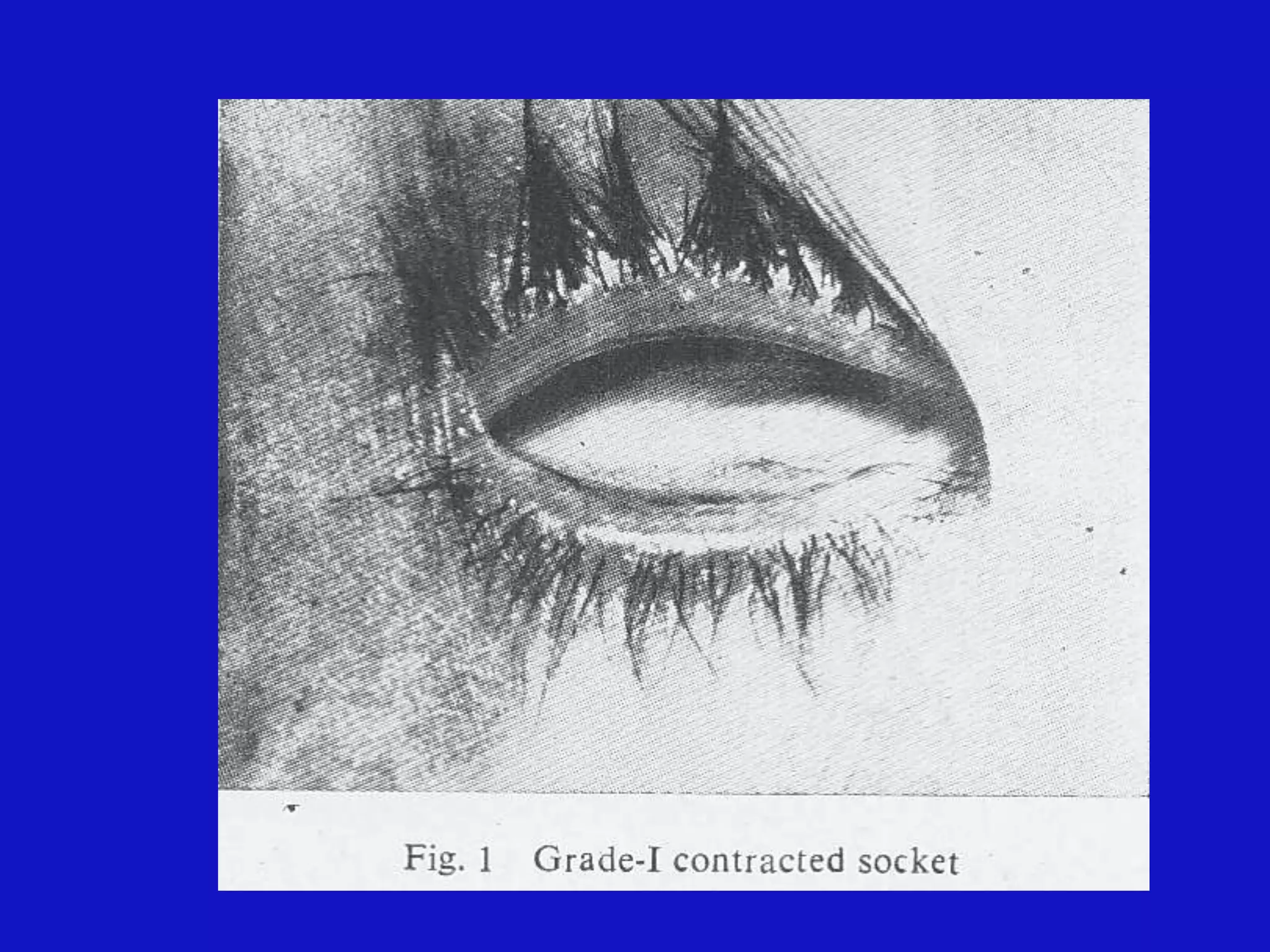
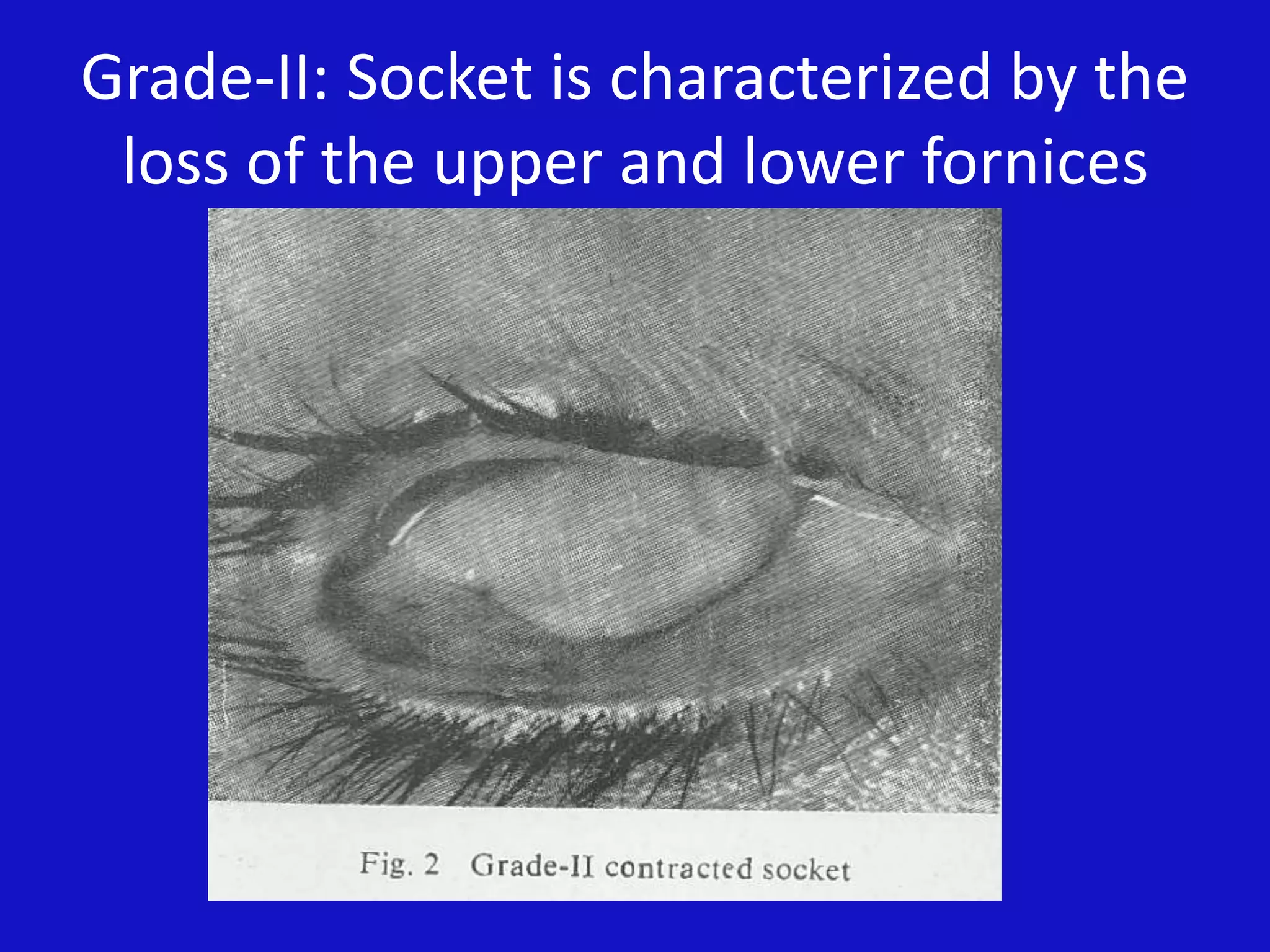
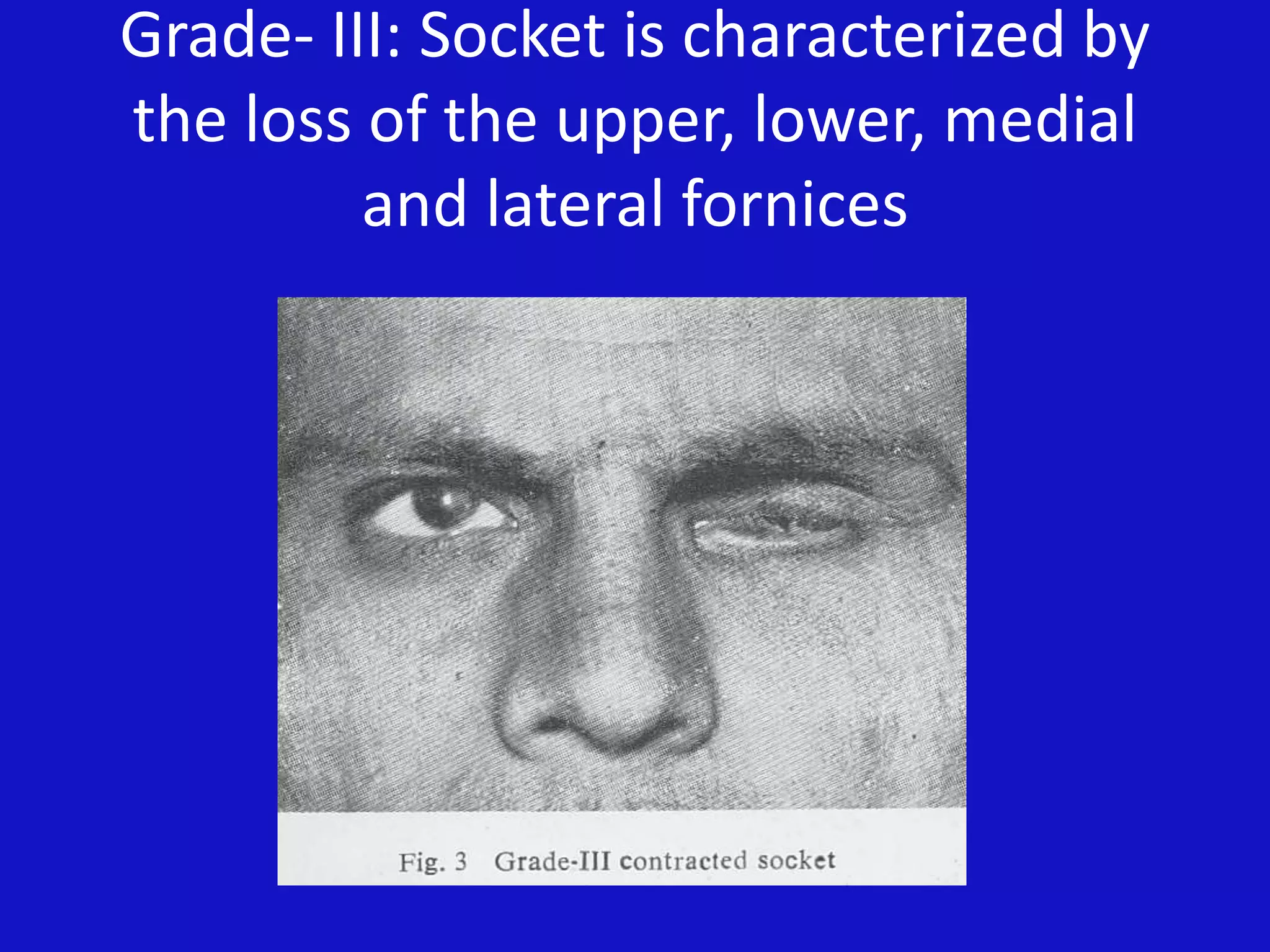
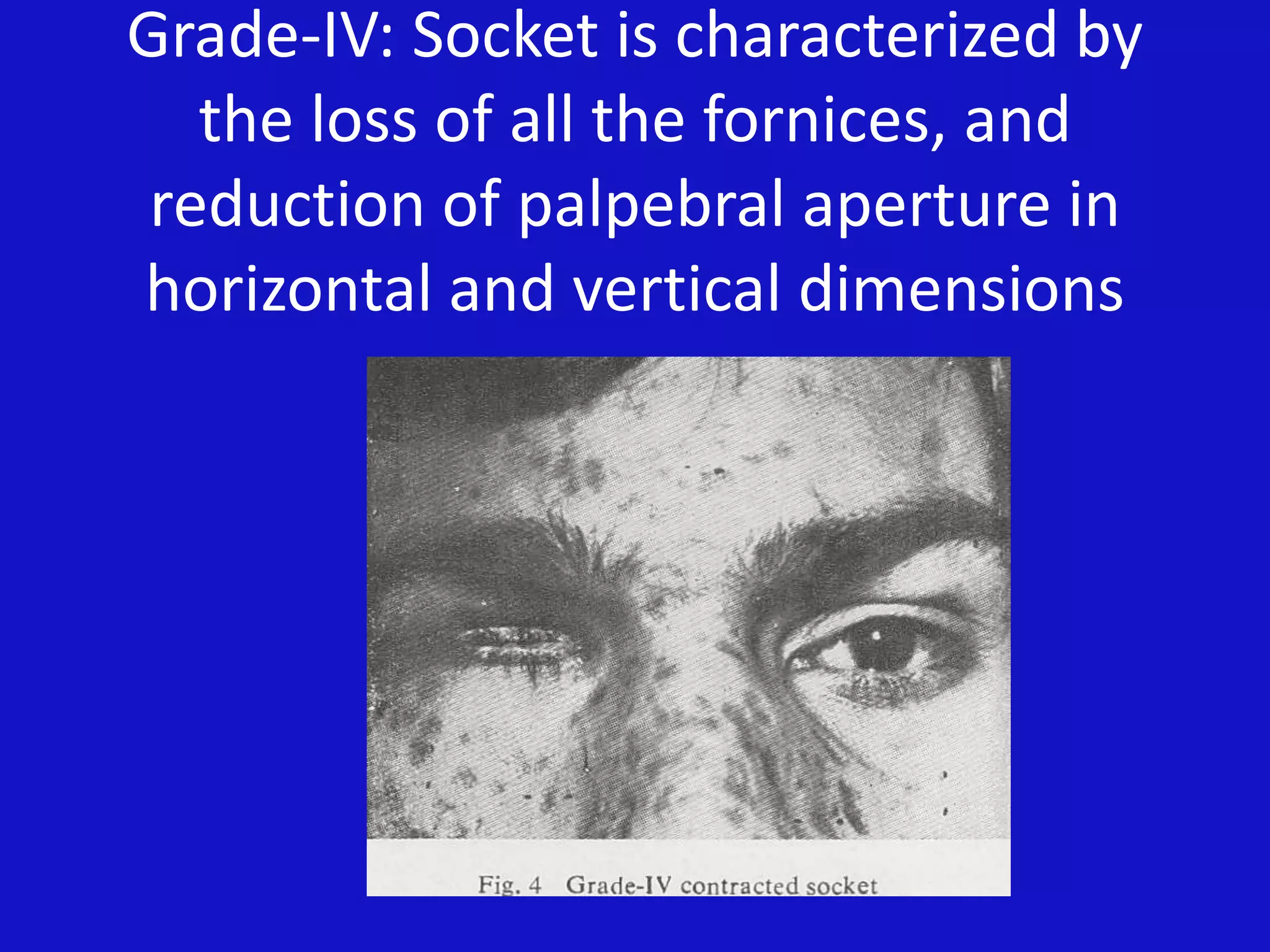
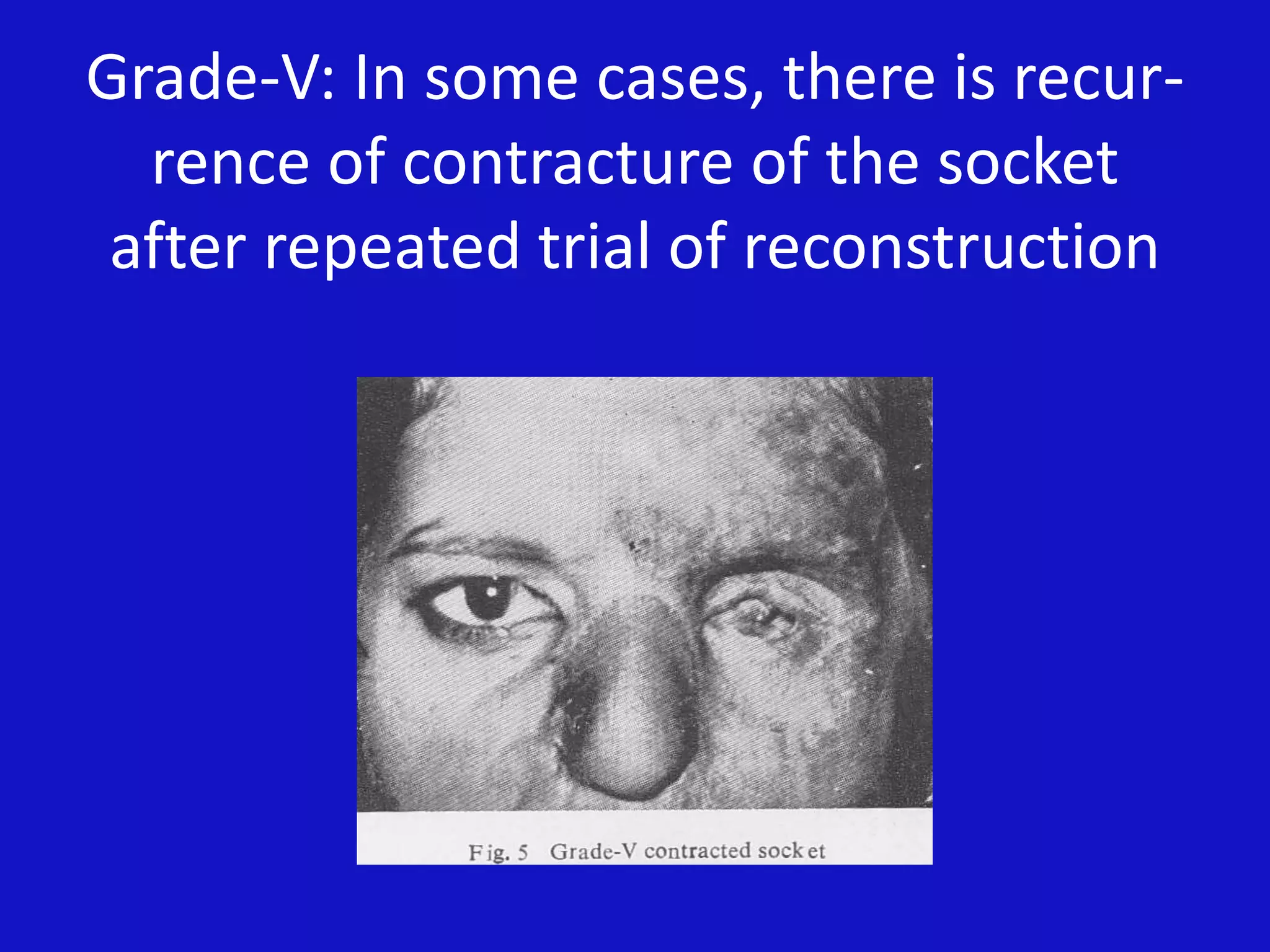
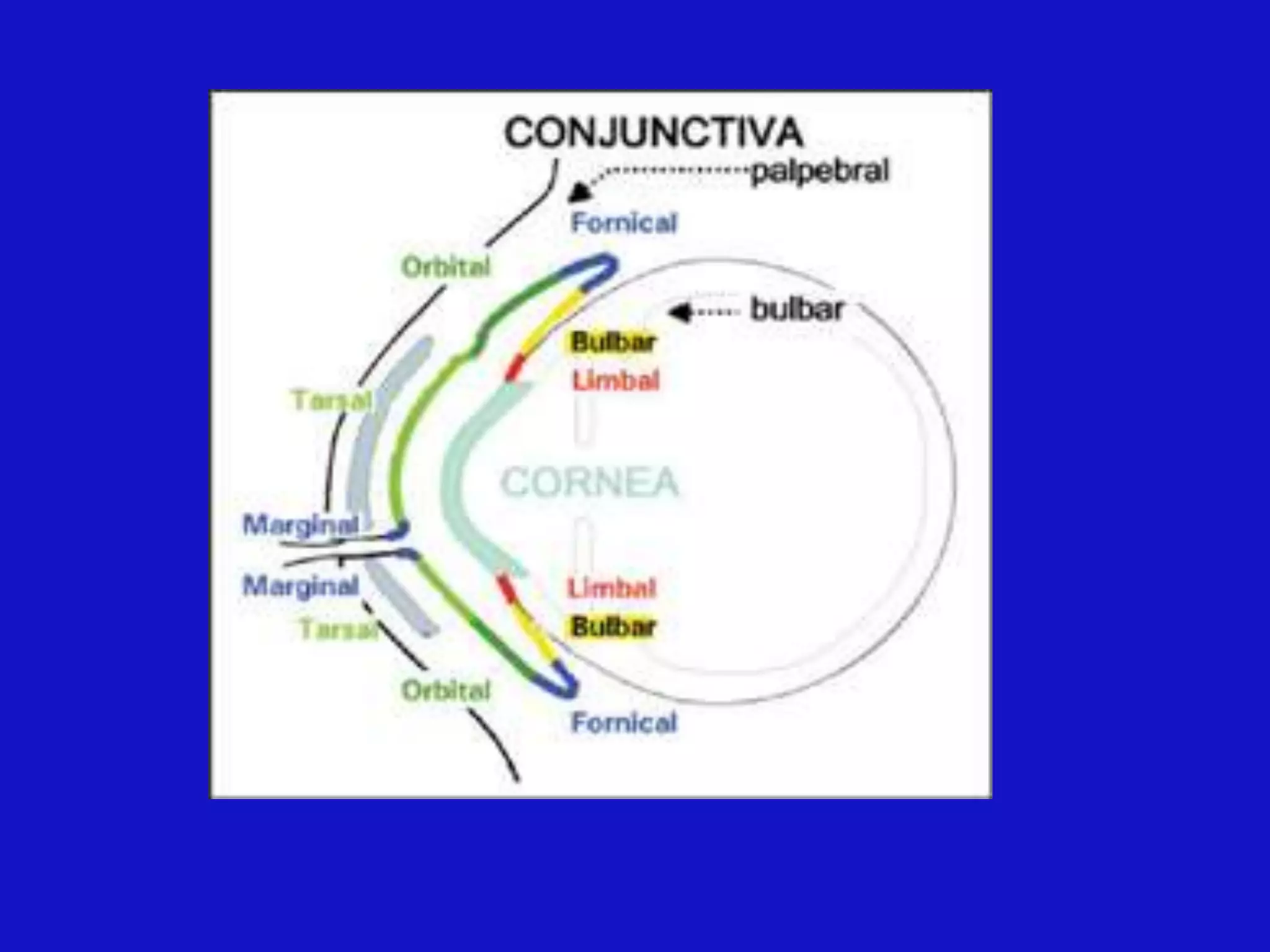
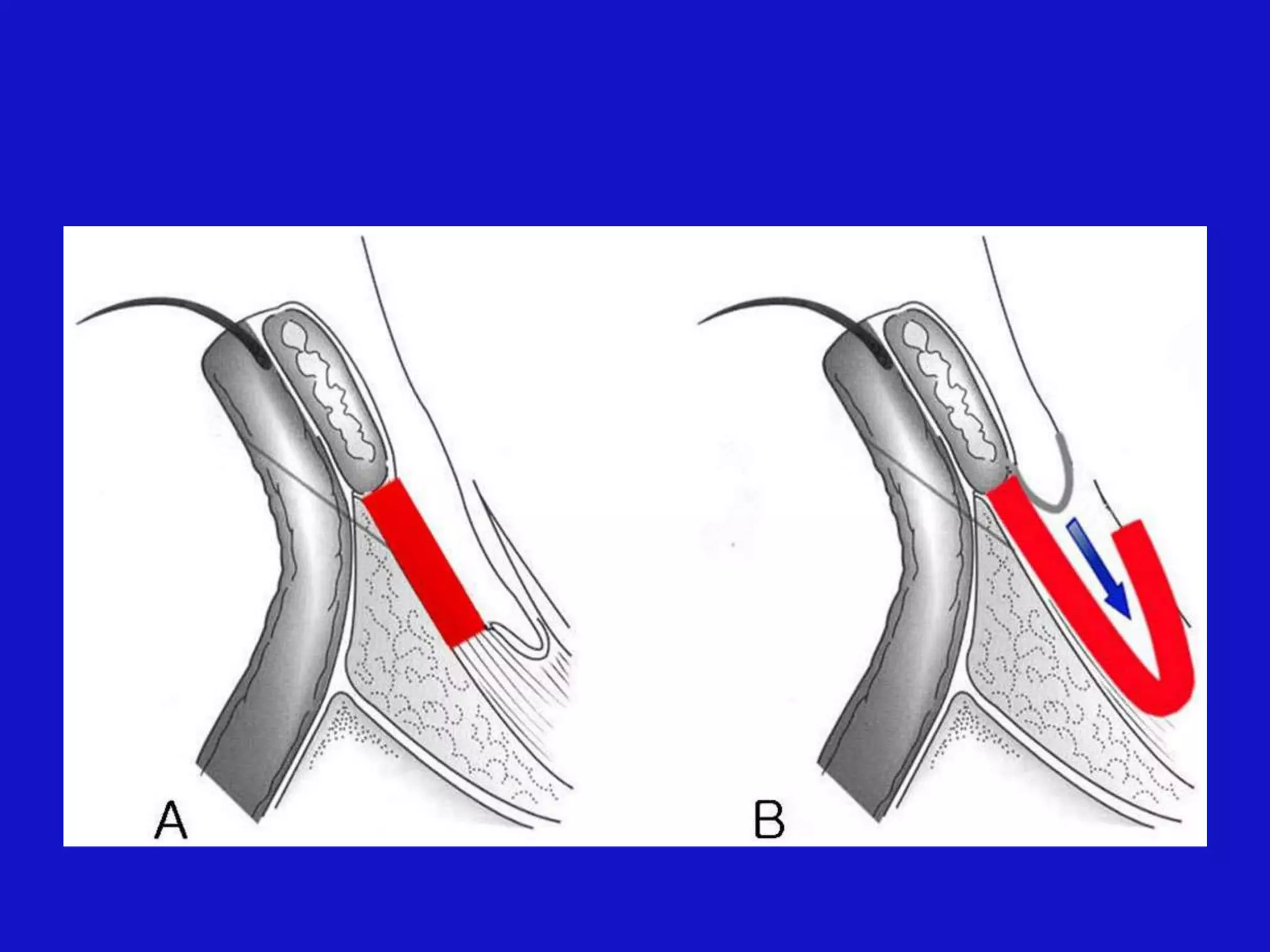
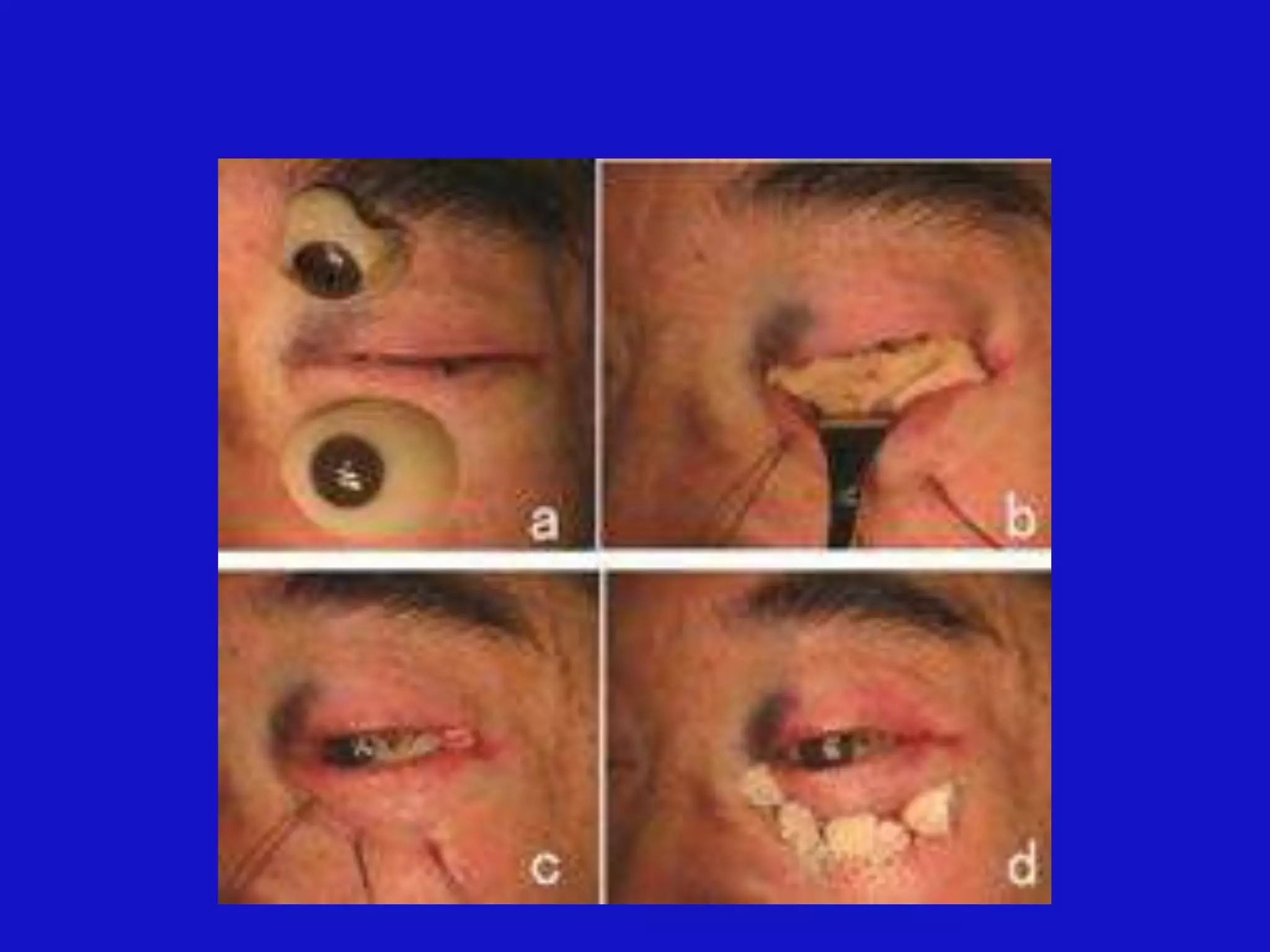
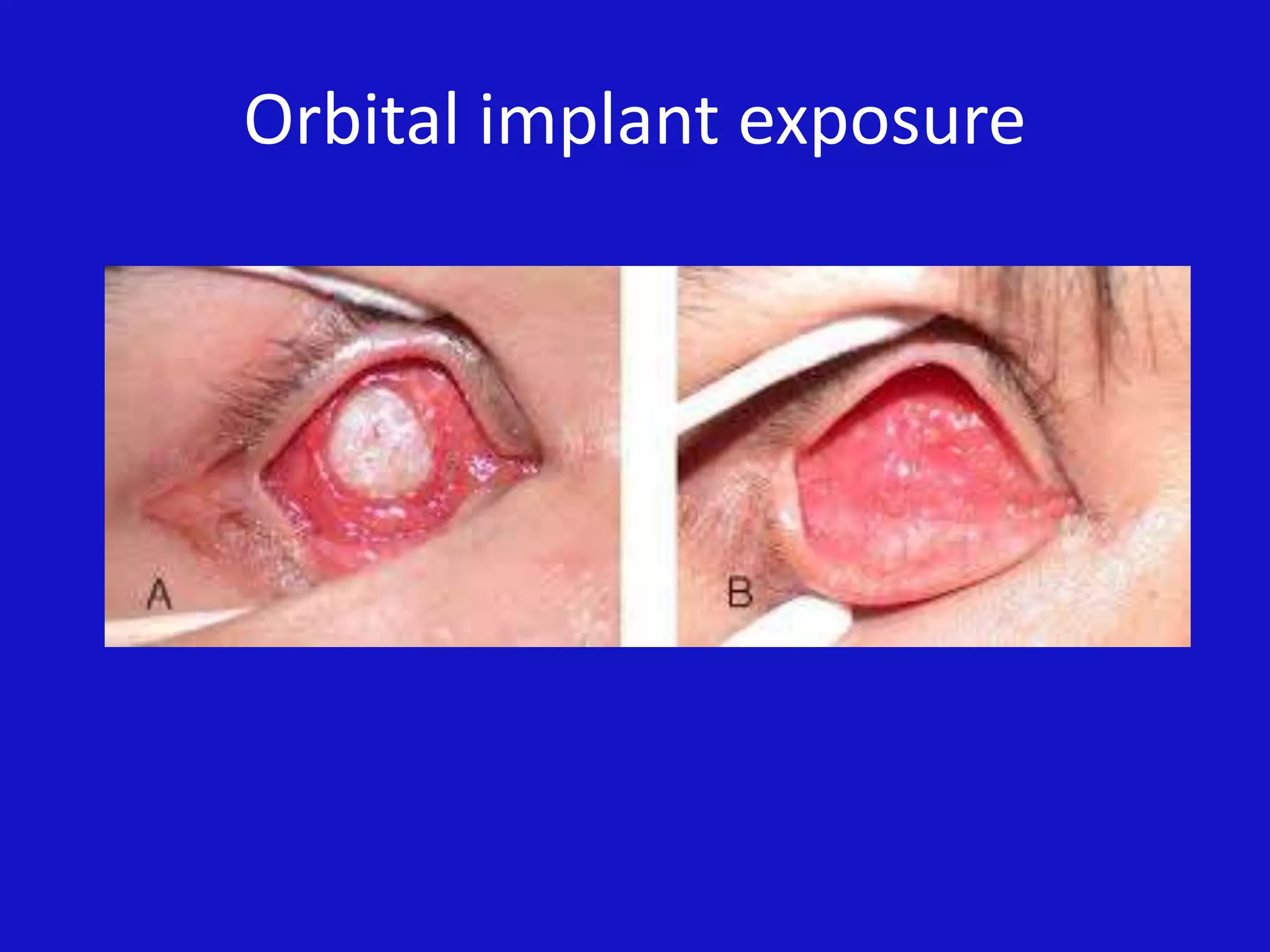
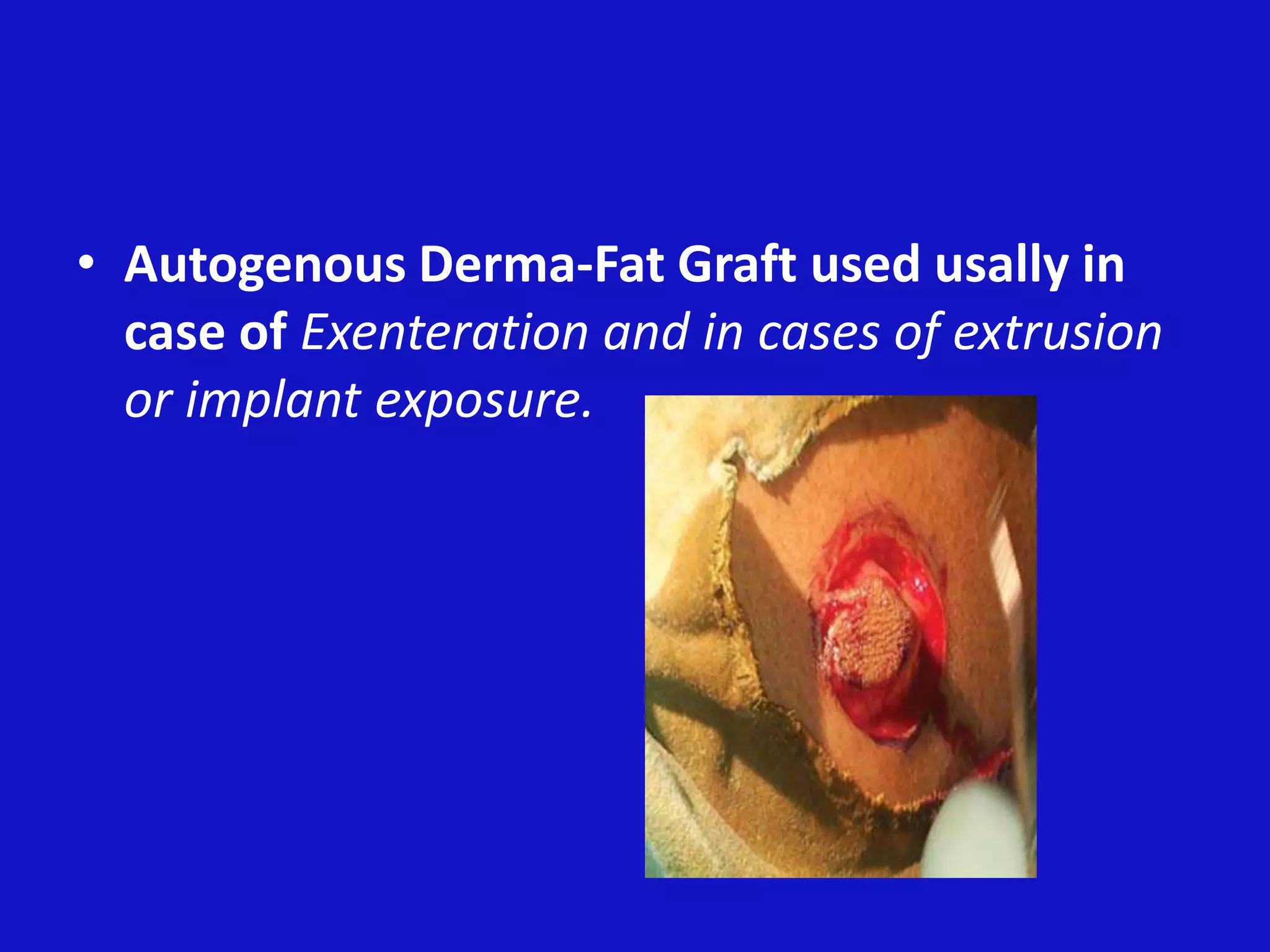
The document discusses contracted eye socket reconstruction. It defines an eye socket and the causes of eye removal (enucleation and exenteration). Socket contracture can result from scarring or infections and causes difficulty retaining prosthetics. Grades of contracture are described from mild to severe. Reconstruction aims to establish stable fornices using grafts to increase surface area and implants if needed. Prevention involves using conformers after removal and temporary tarsorrhaphy may be used. Autogenous derma-fat grafts can repair implant exposures.