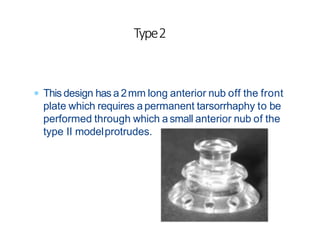
This document provides information about artificial cornea or keratoprosthesis surgery. It discusses the history and indications for the procedure, describes common designs for artificial corneas including biointegrated and non-biointegrated options, and outlines some of the major keratoprosthesis designs including the Boston KPro, AlphaCor KPro, and modified osteo-odonto keratoprosthesis. It also covers the preoperative evaluation, surgical procedure, postoperative management, prognosis, and complications for keratoprosthesis surgery.