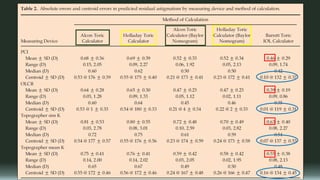
Toric IOLs were developed to reduce astigmatism and improve spectacle independence for patients with cataracts and astigmatism. The document summarizes the history, design, and clinical outcomes of toric IOLs. A meta-analysis found that patients receiving toric IOLs were more likely to achieve good visual acuity without glasses compared to patients receiving non-toric IOLs or relaxing incisions. While toric IOLs are generally effective, predicting the exact amount of post-operative astigmatism remains challenging due to factors like IOL rotation and variability in surgically induced astigmatism. New technologies aim to improve the accuracy of toric lens alignment and outcomes.