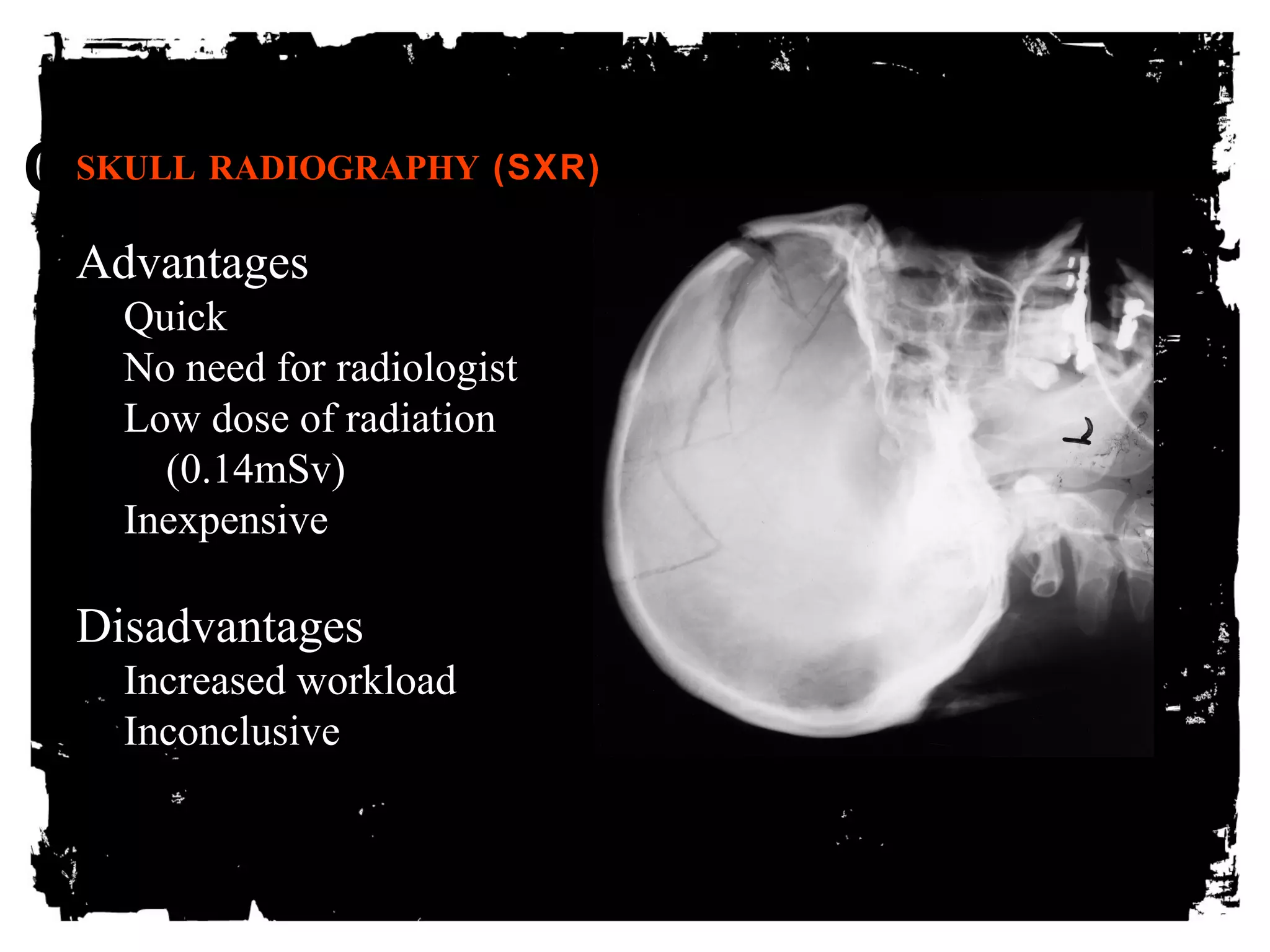
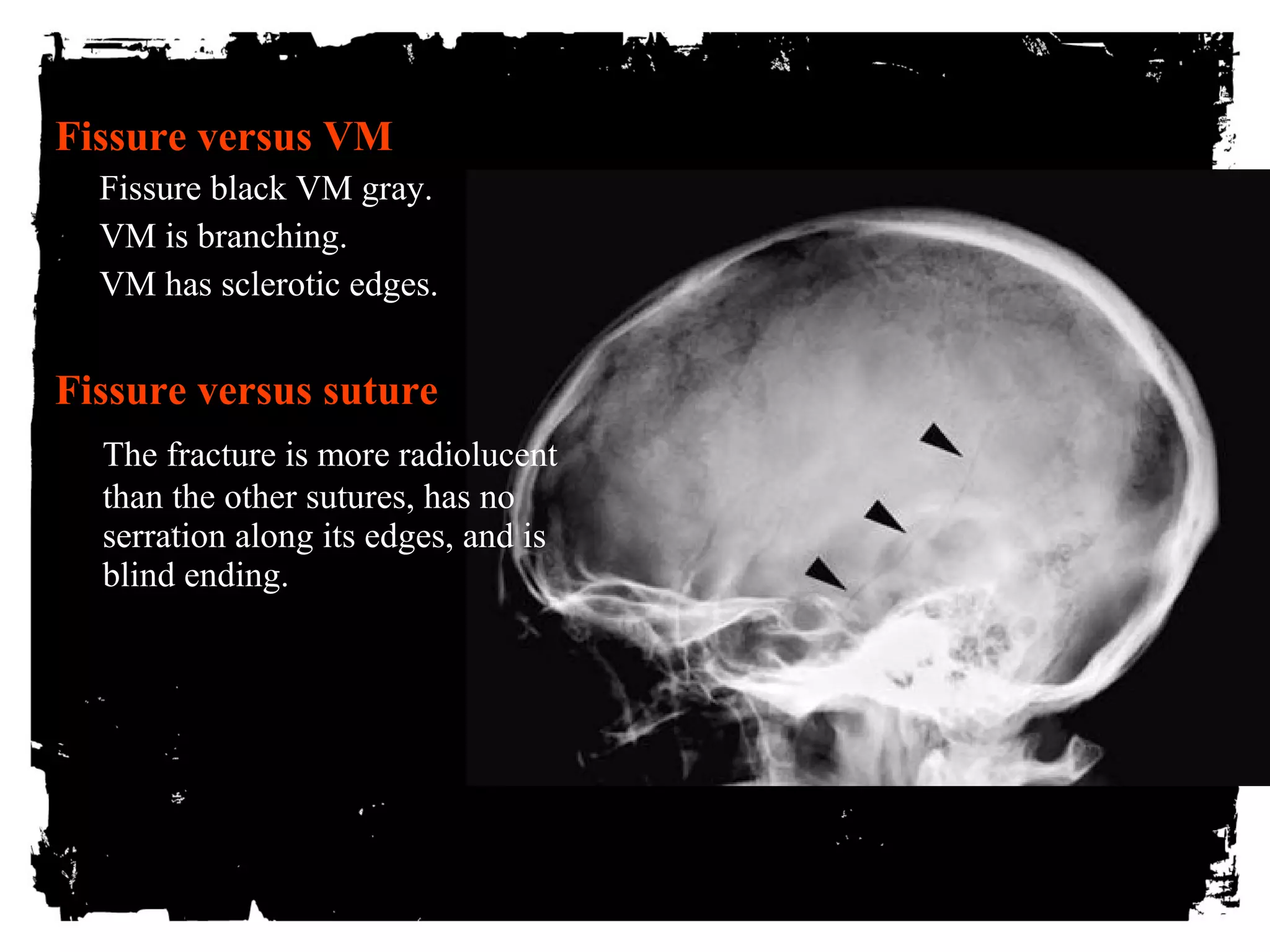
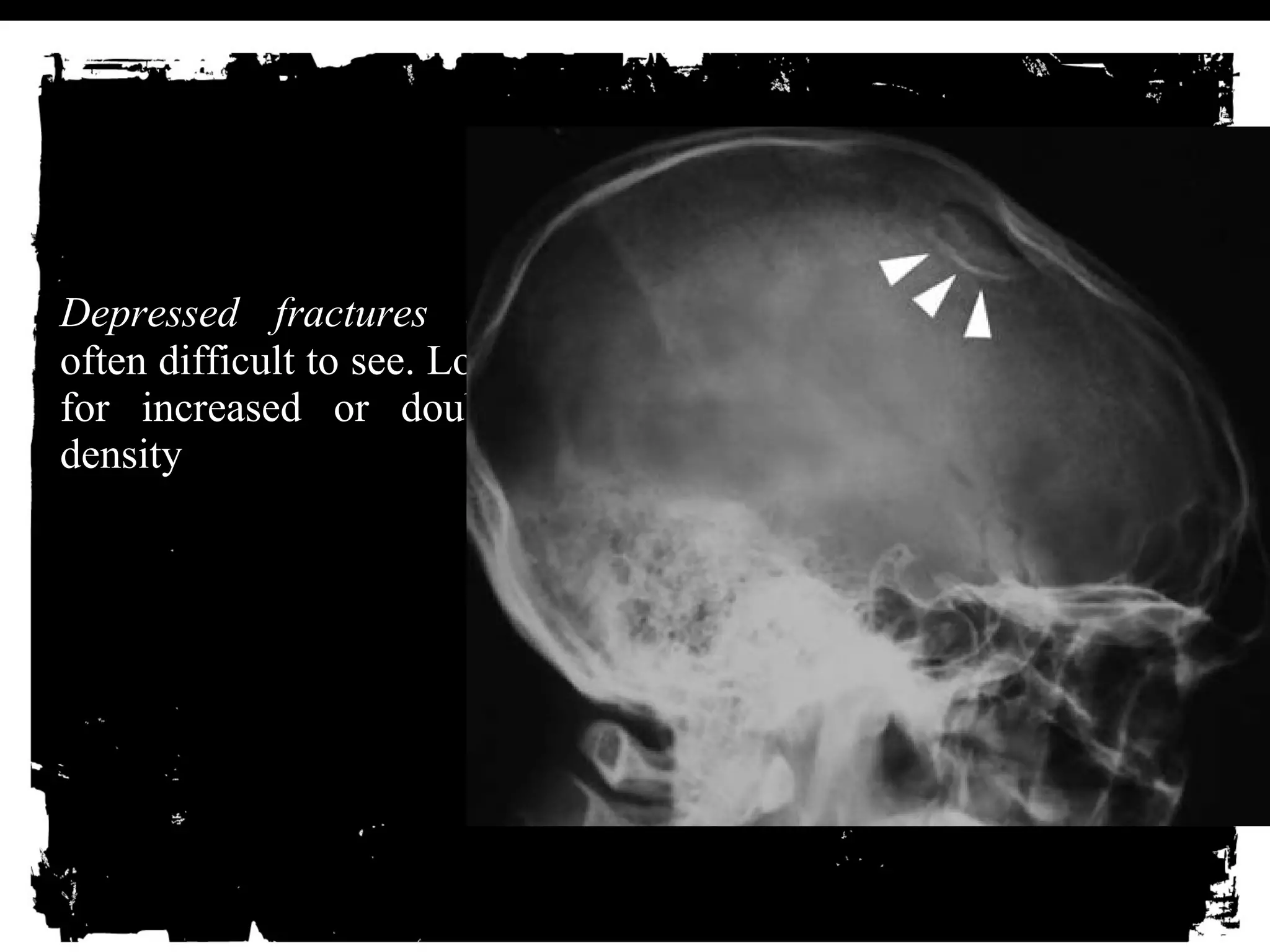
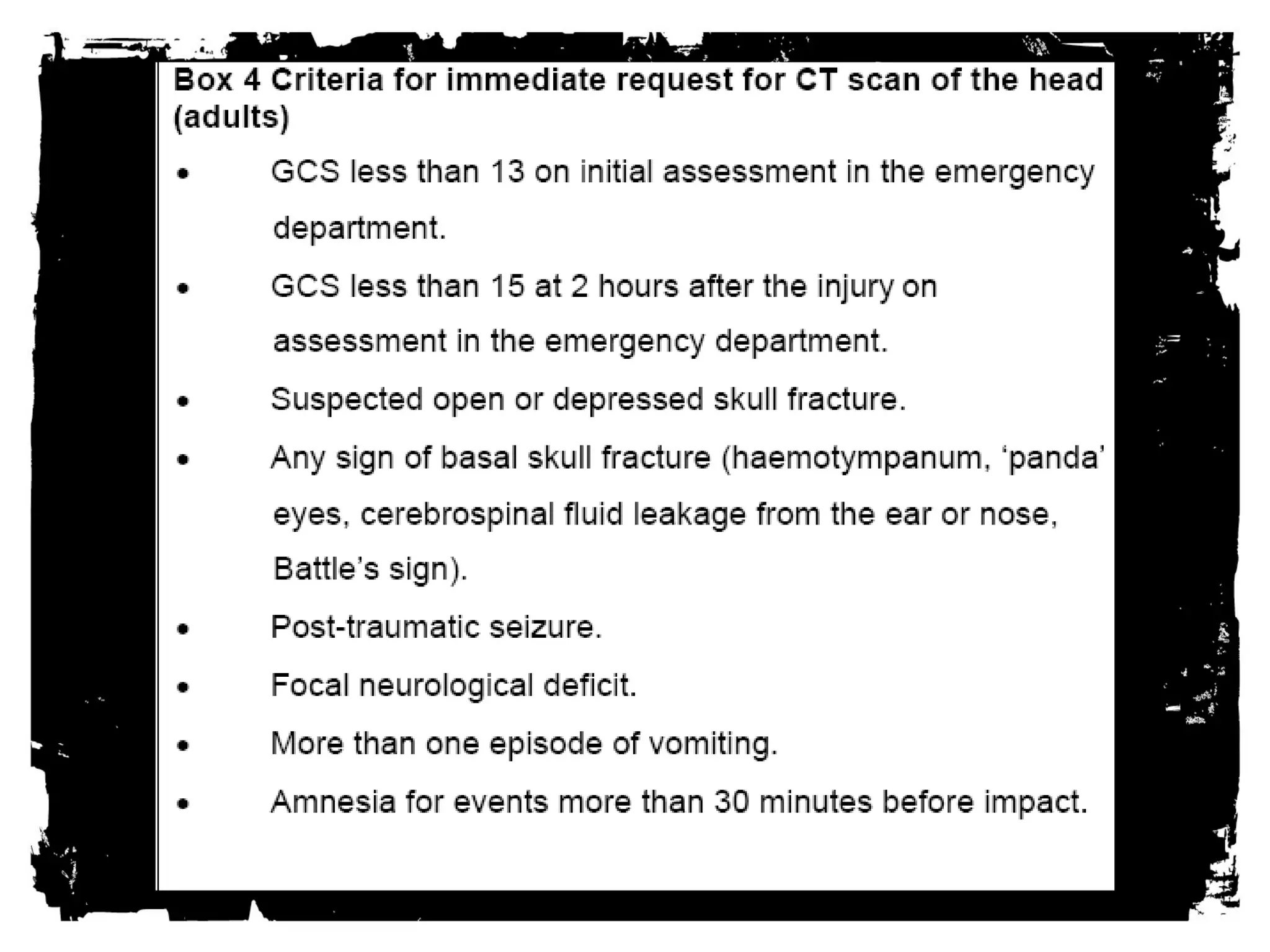
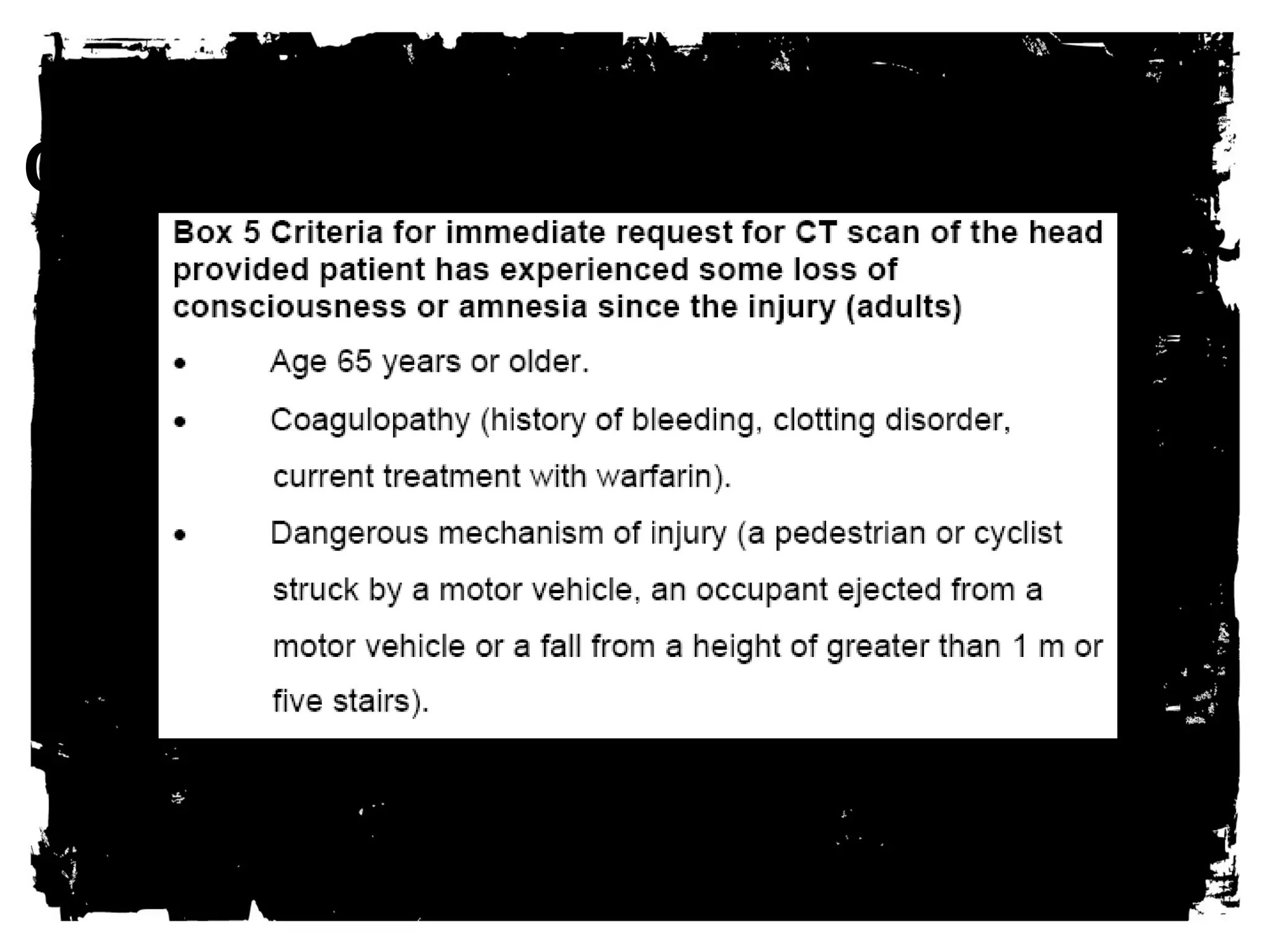
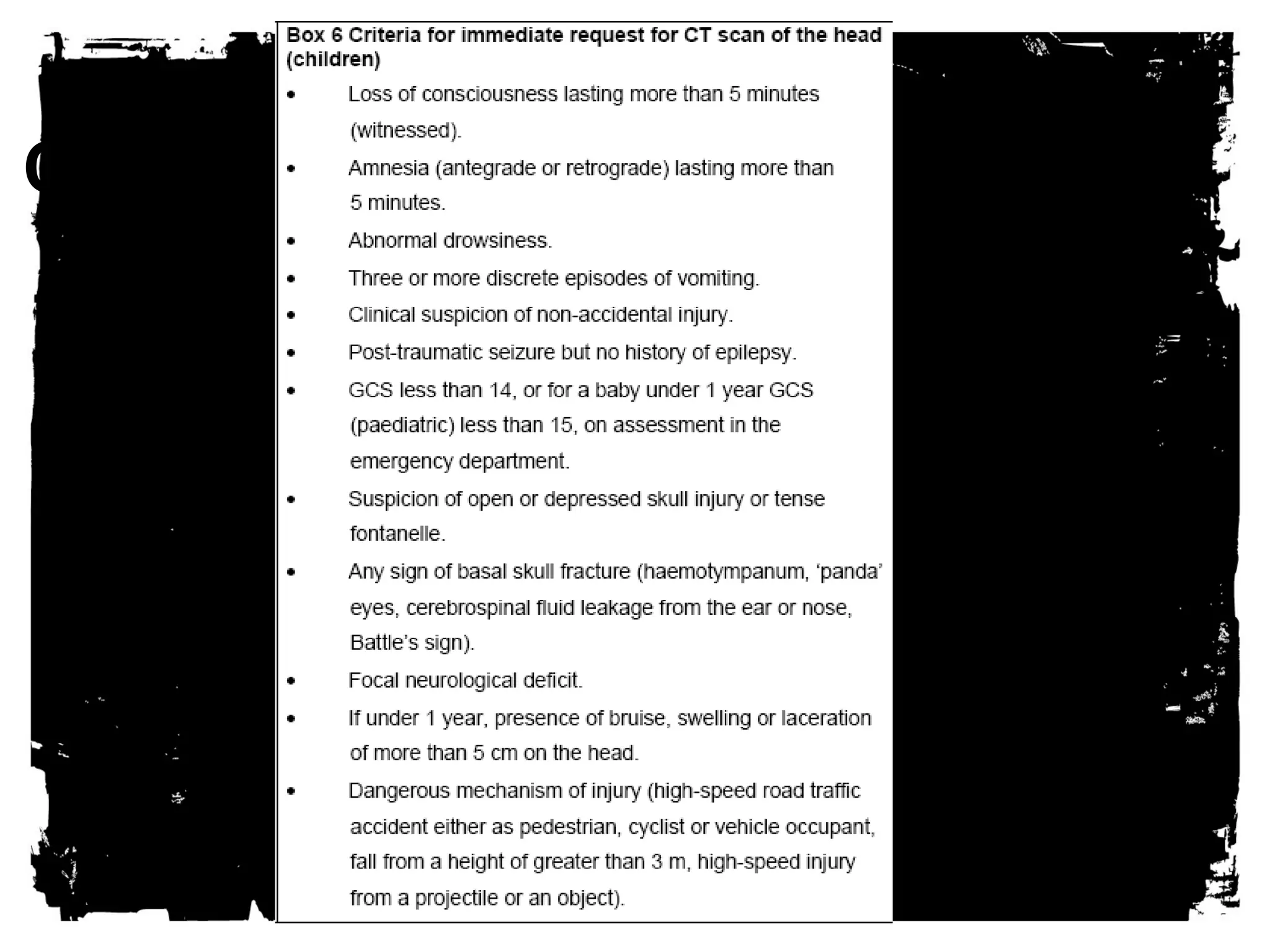
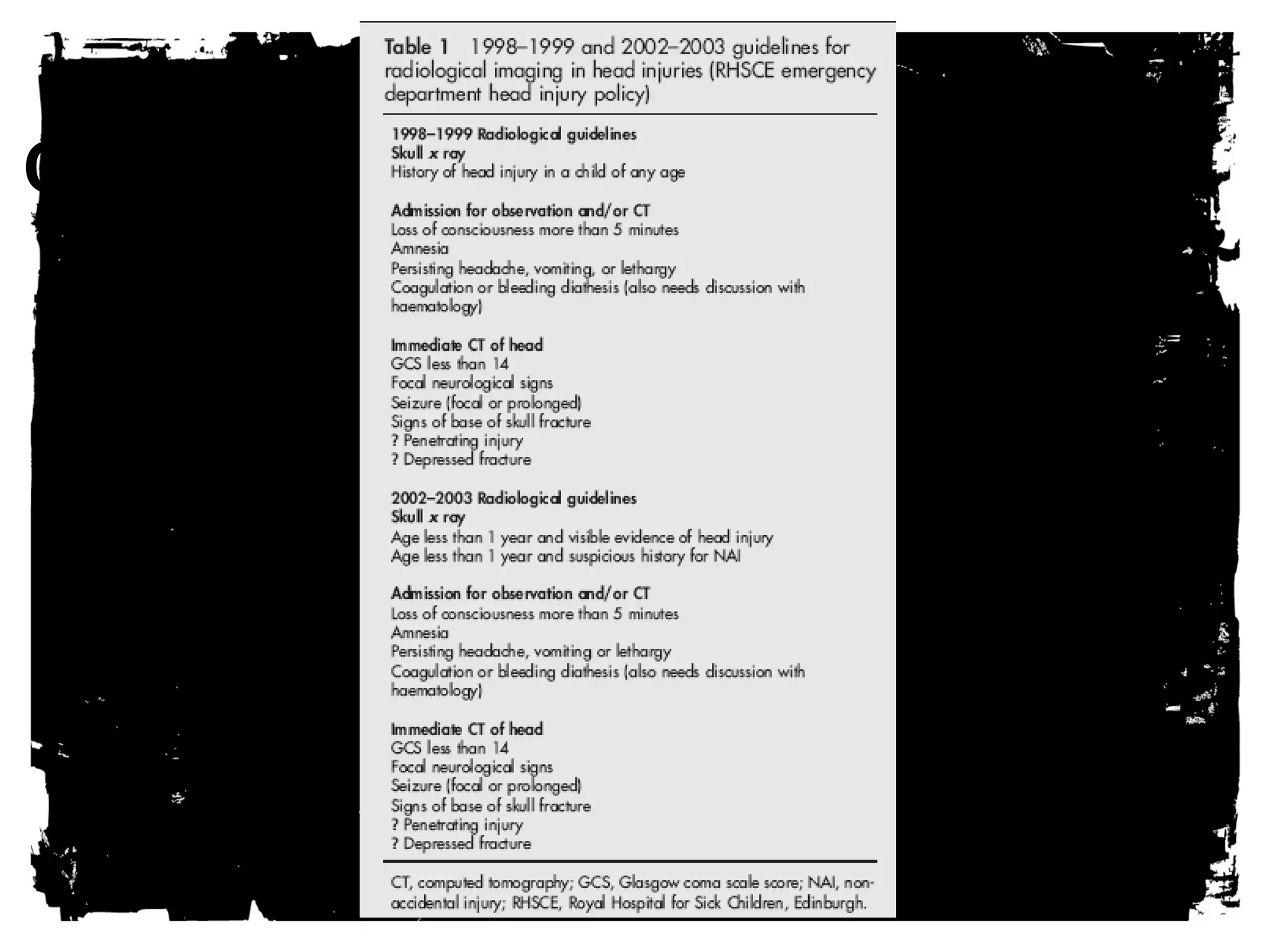
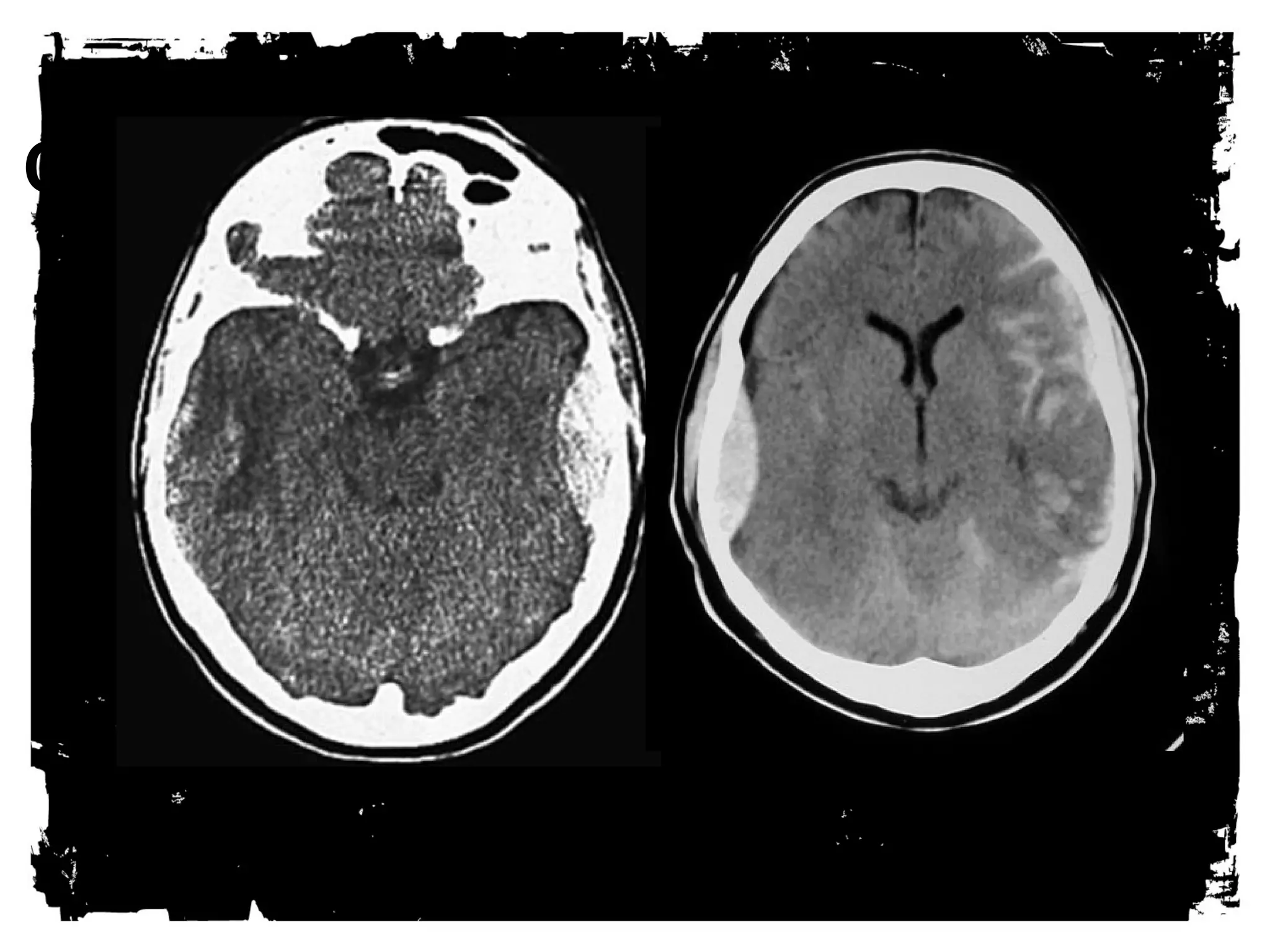
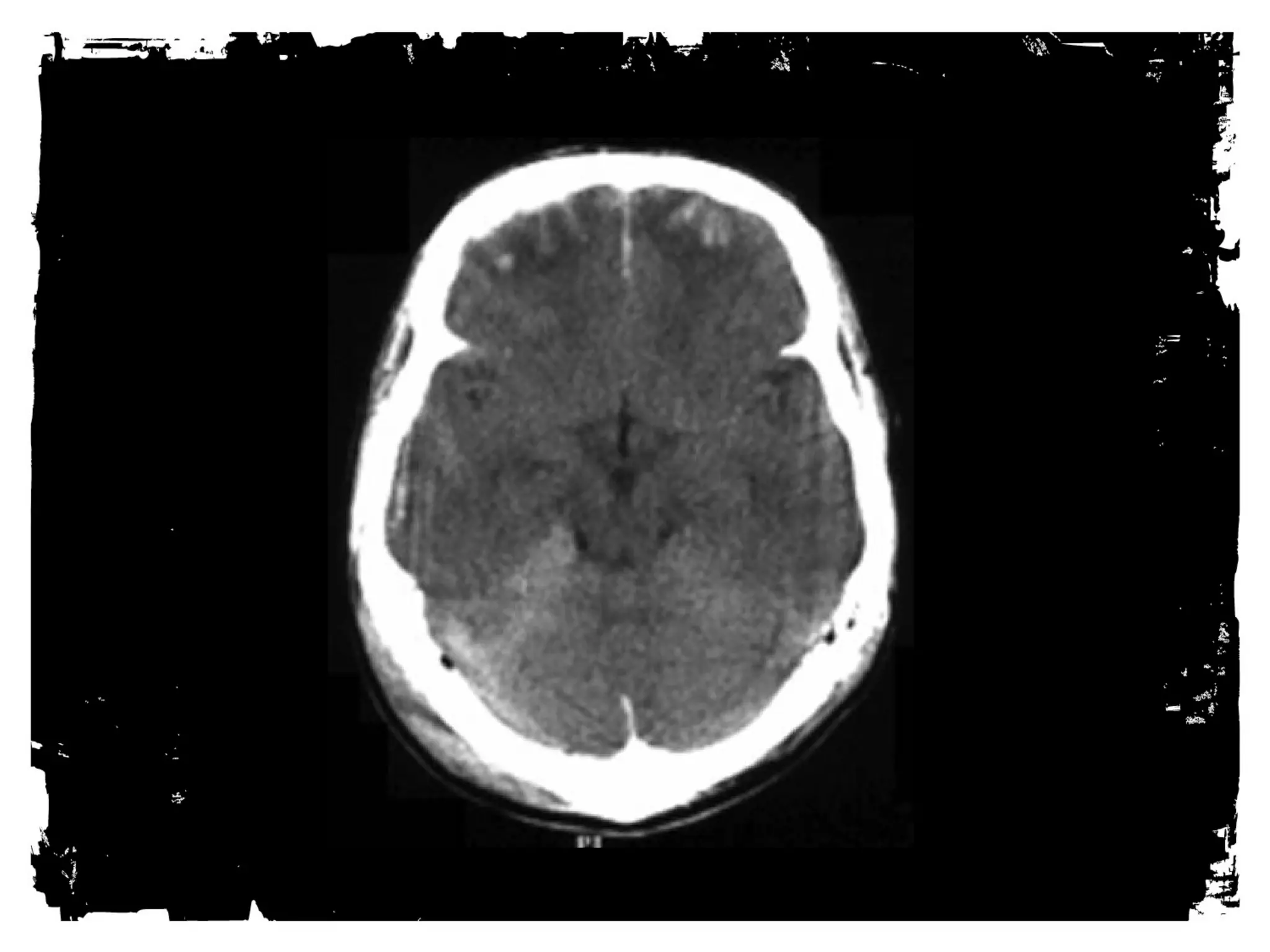
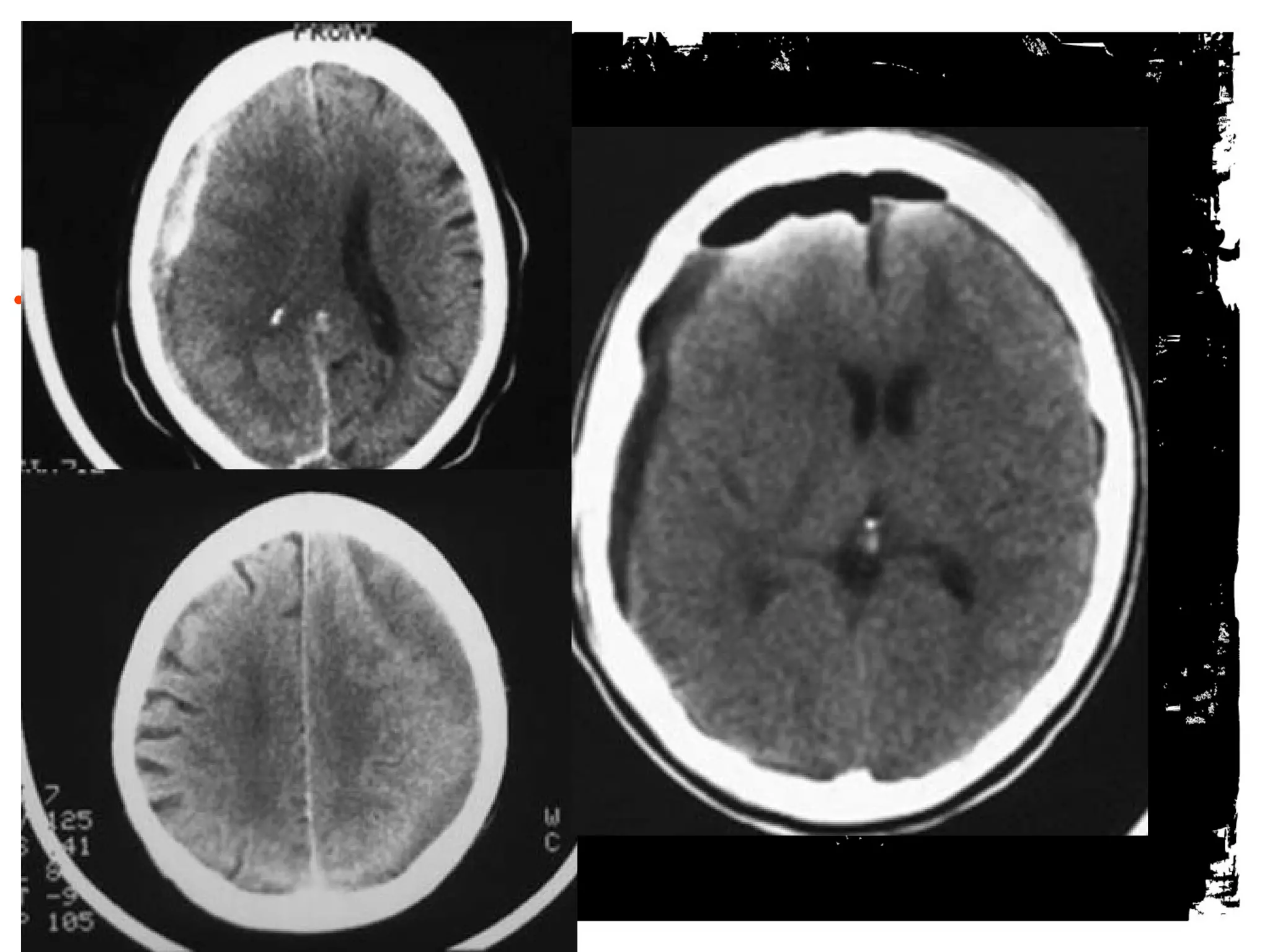
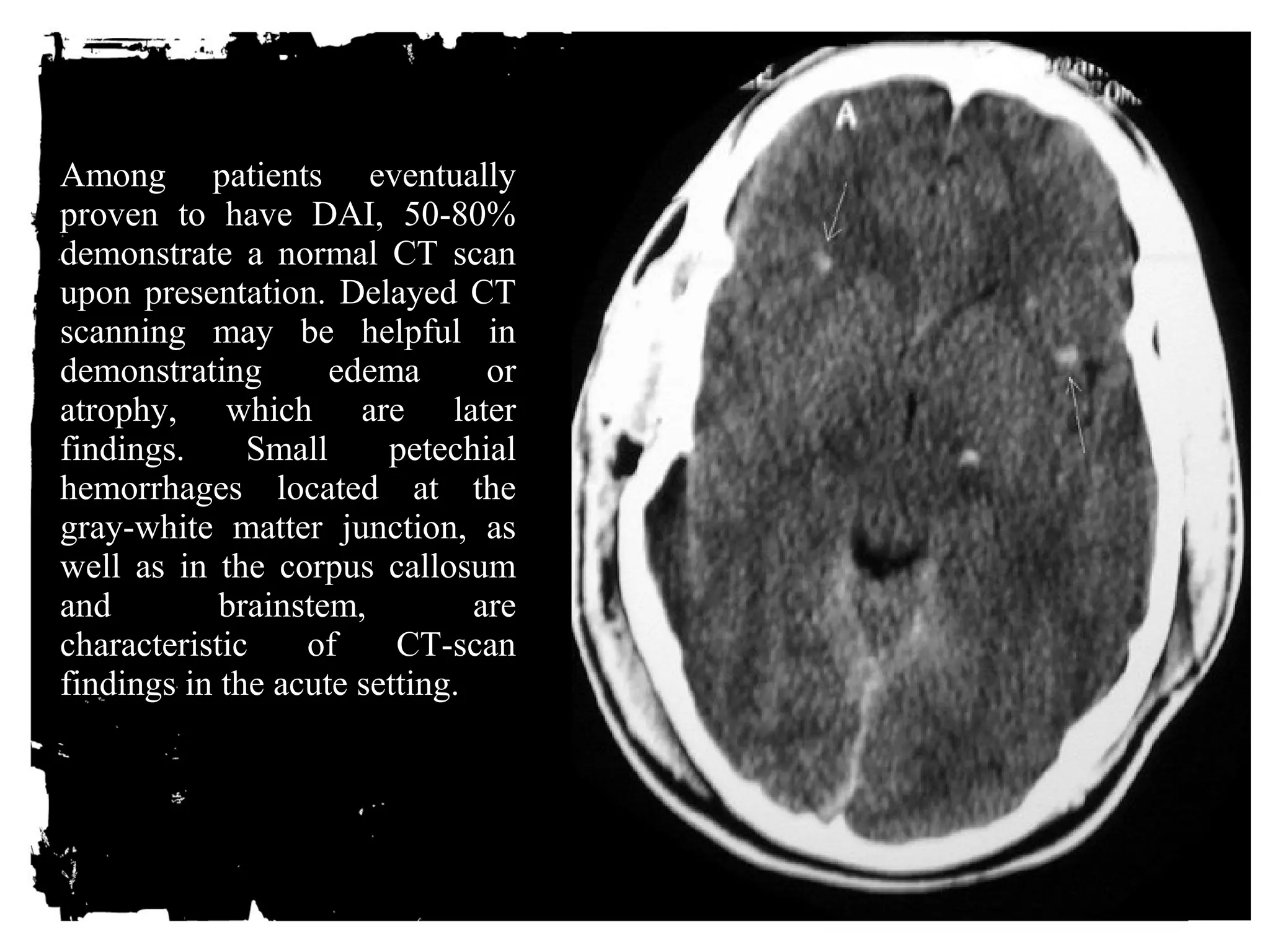
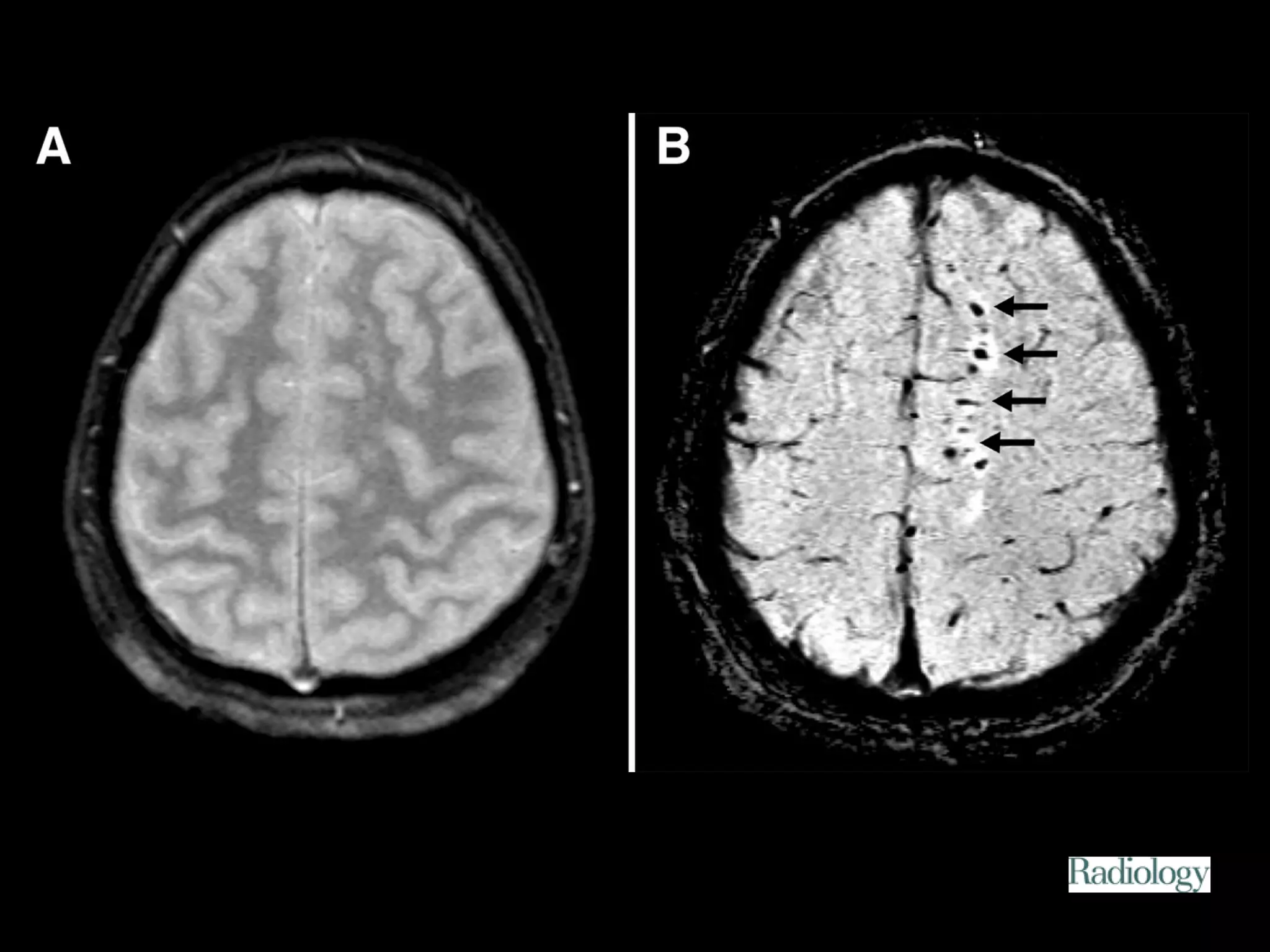
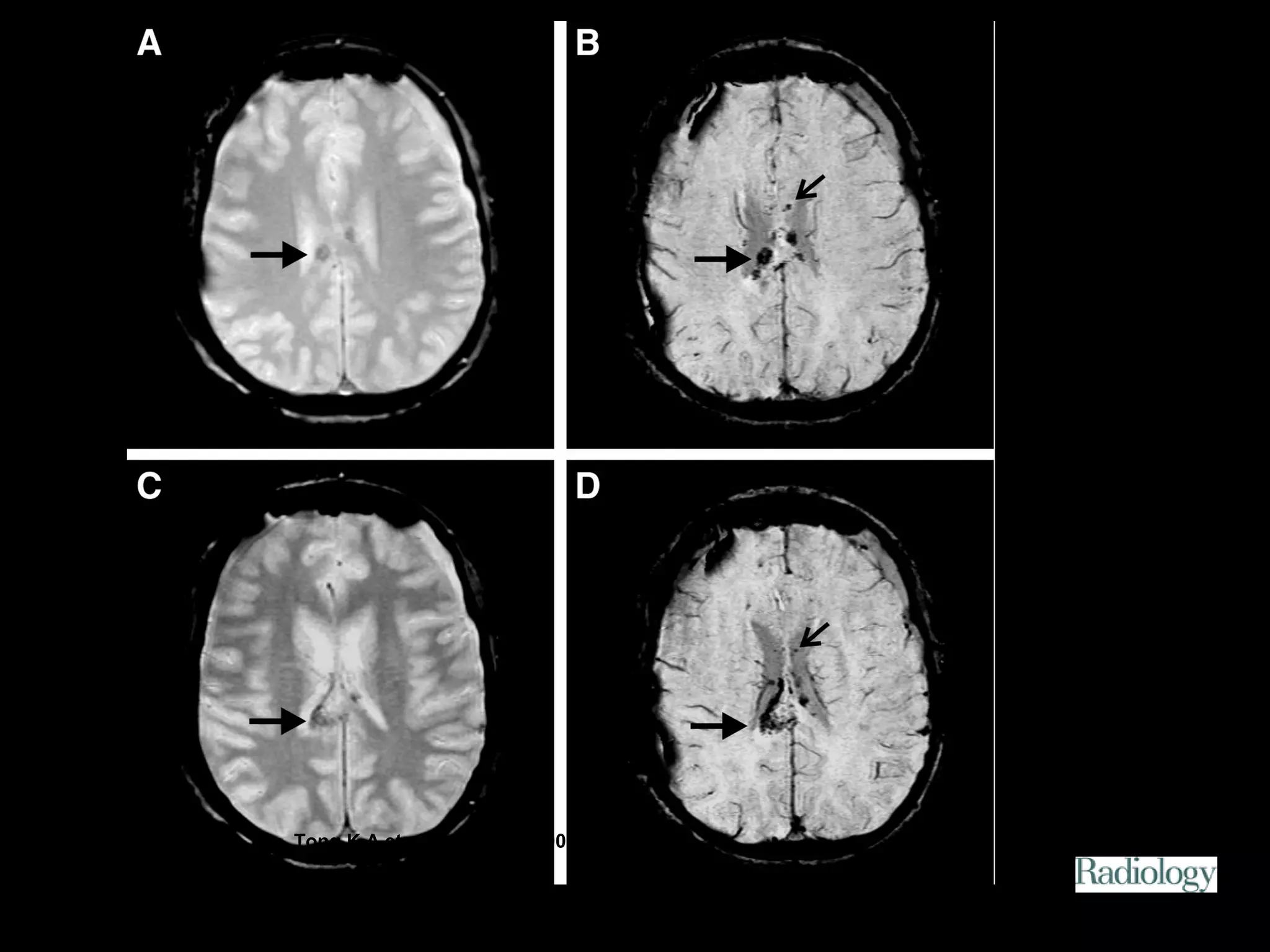
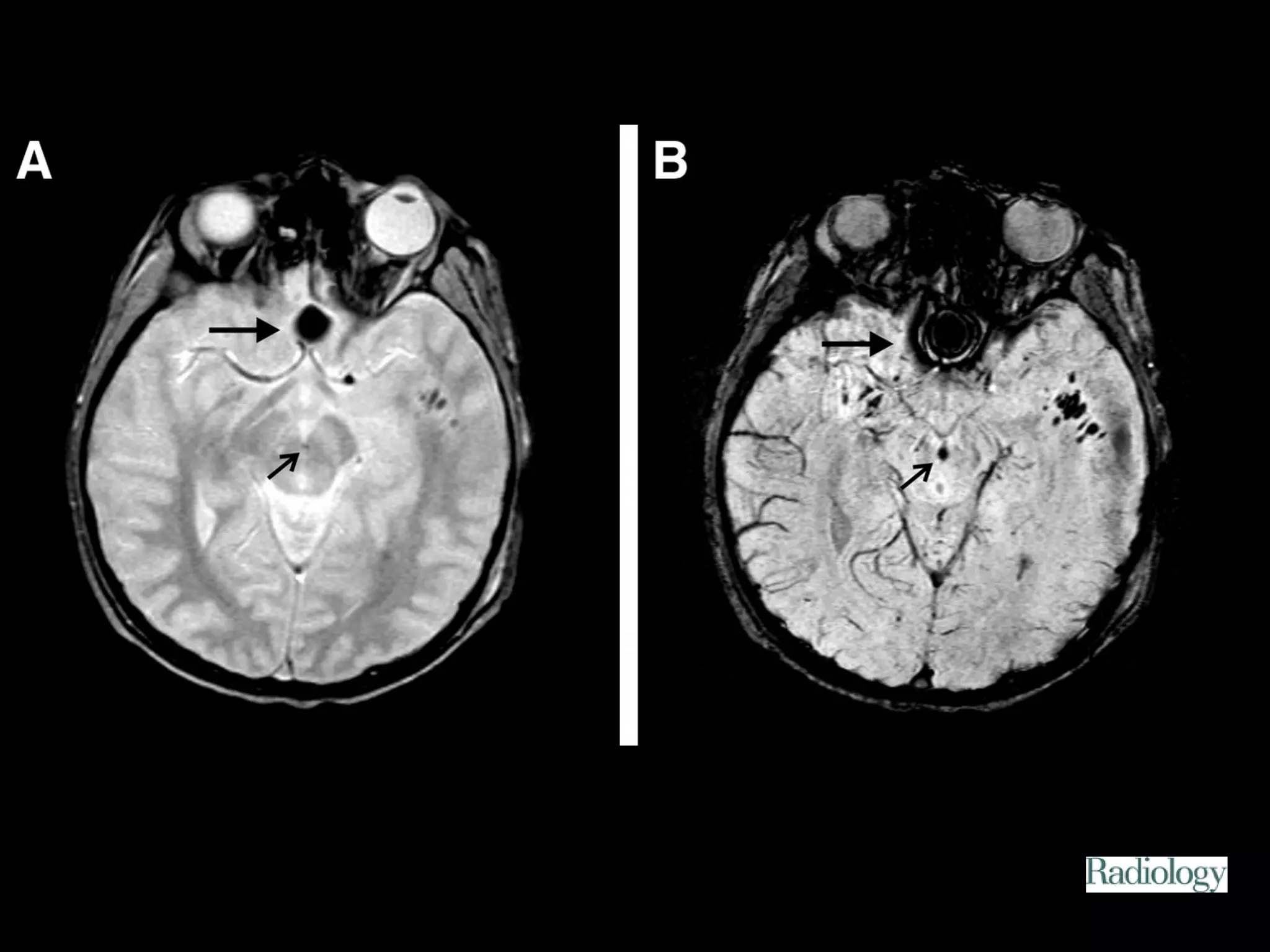
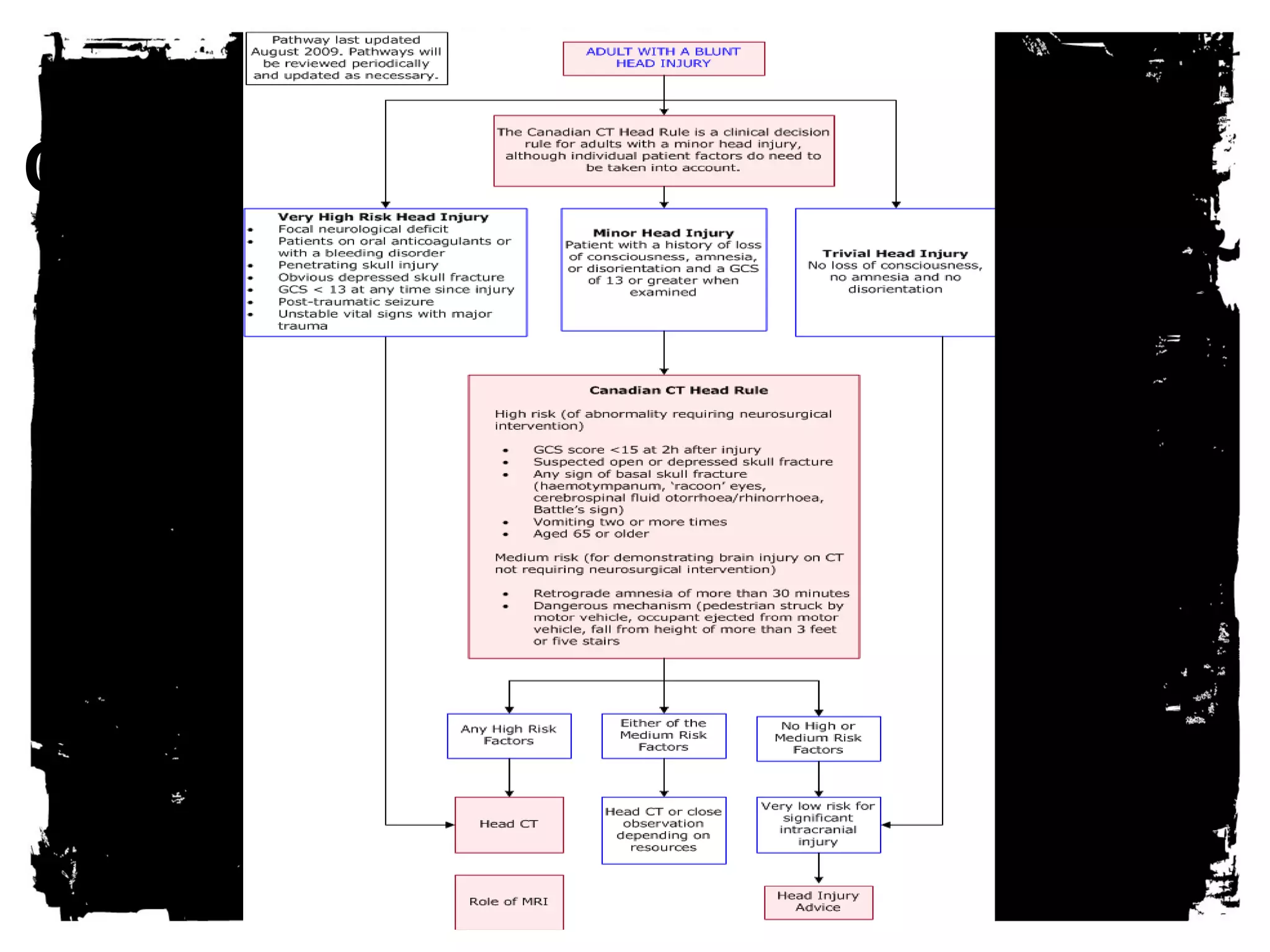
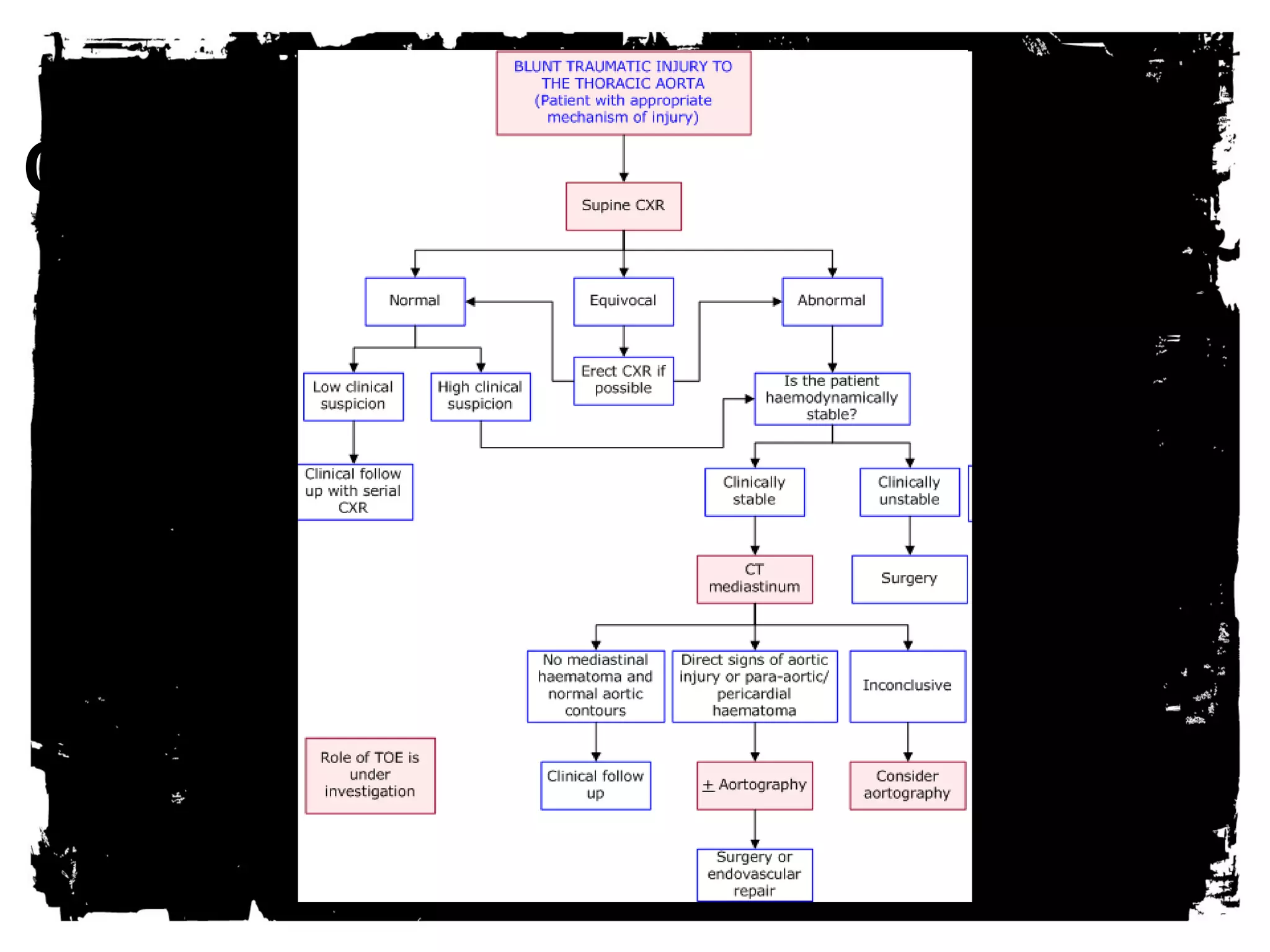
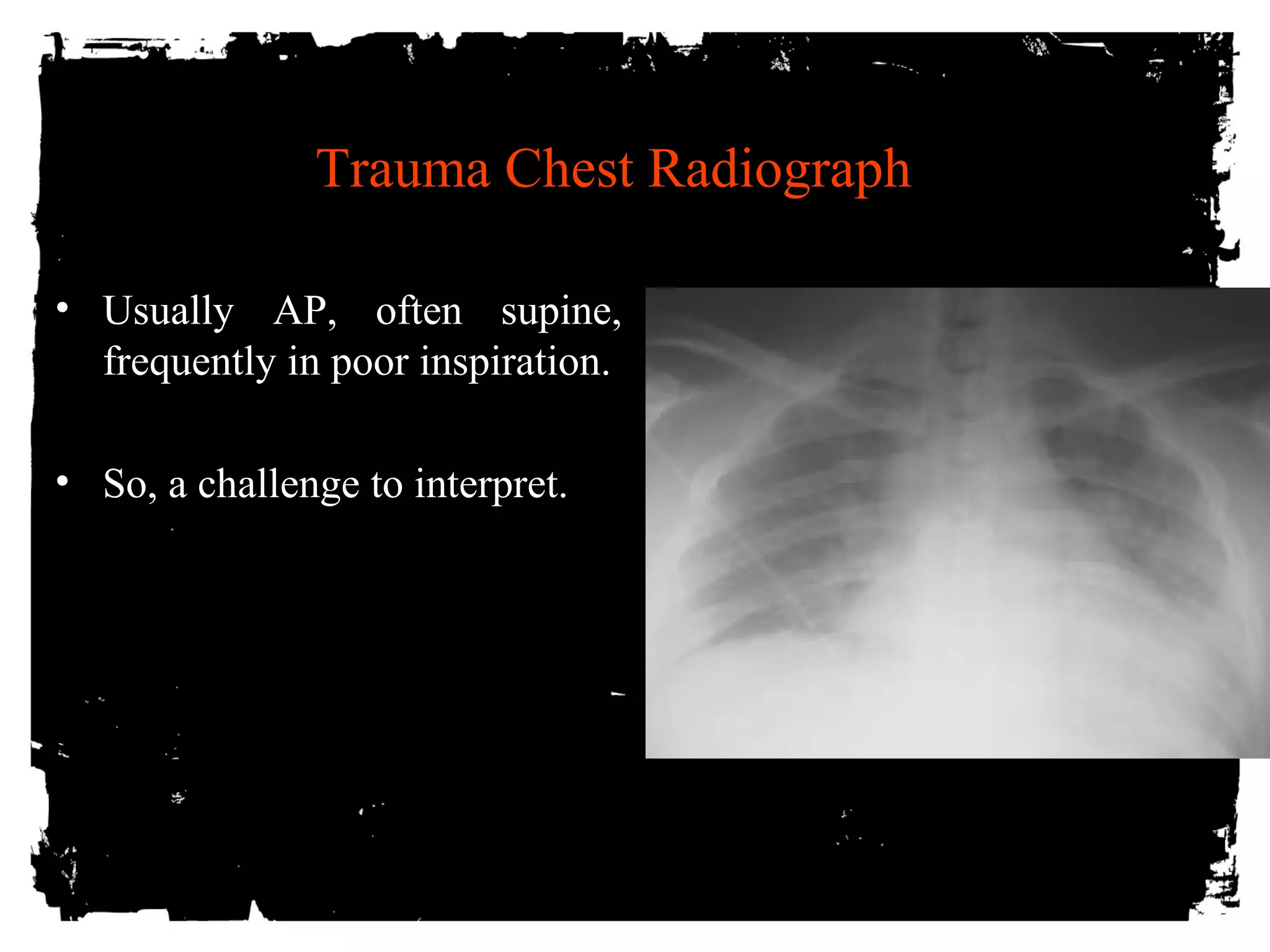
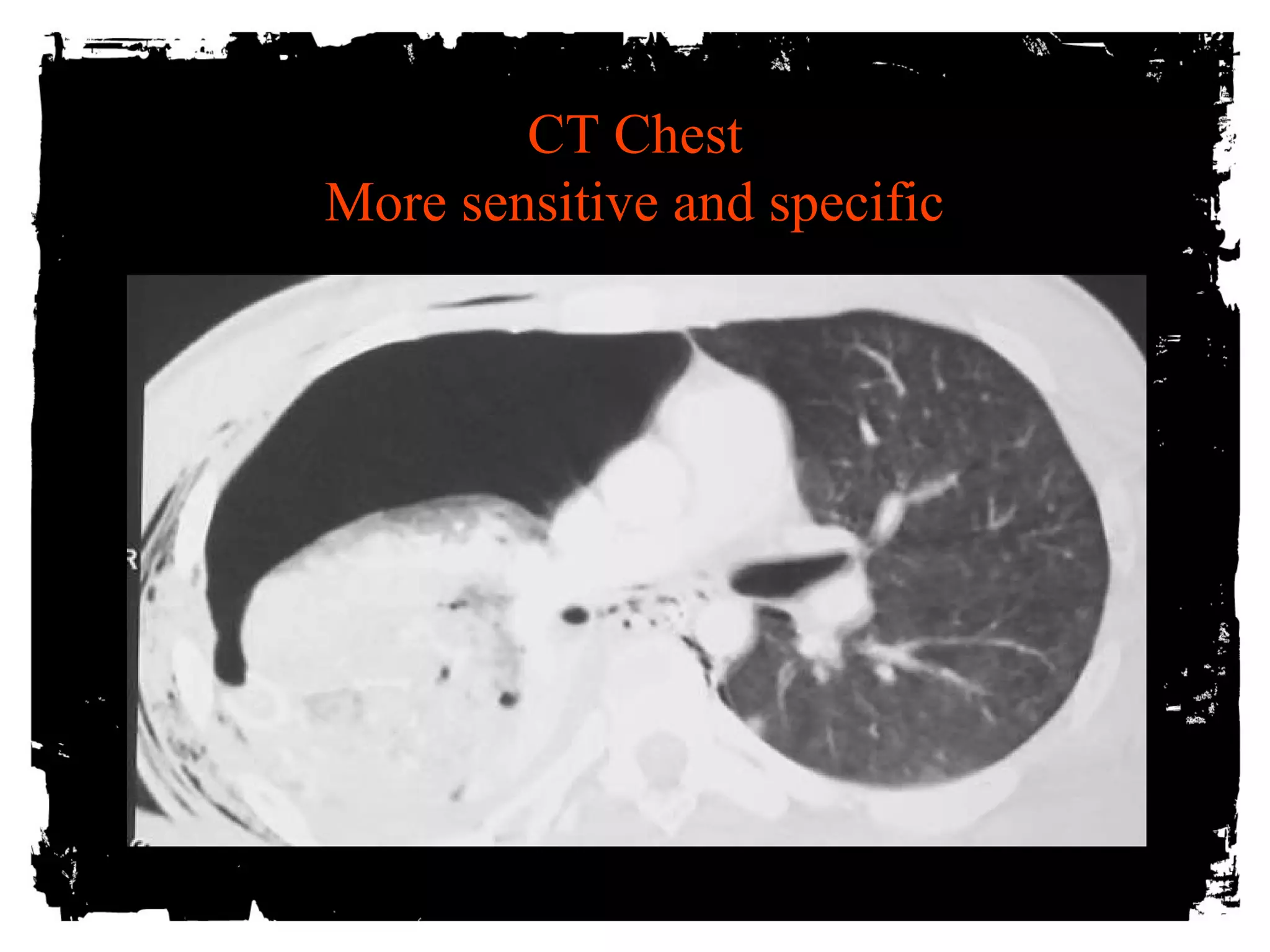
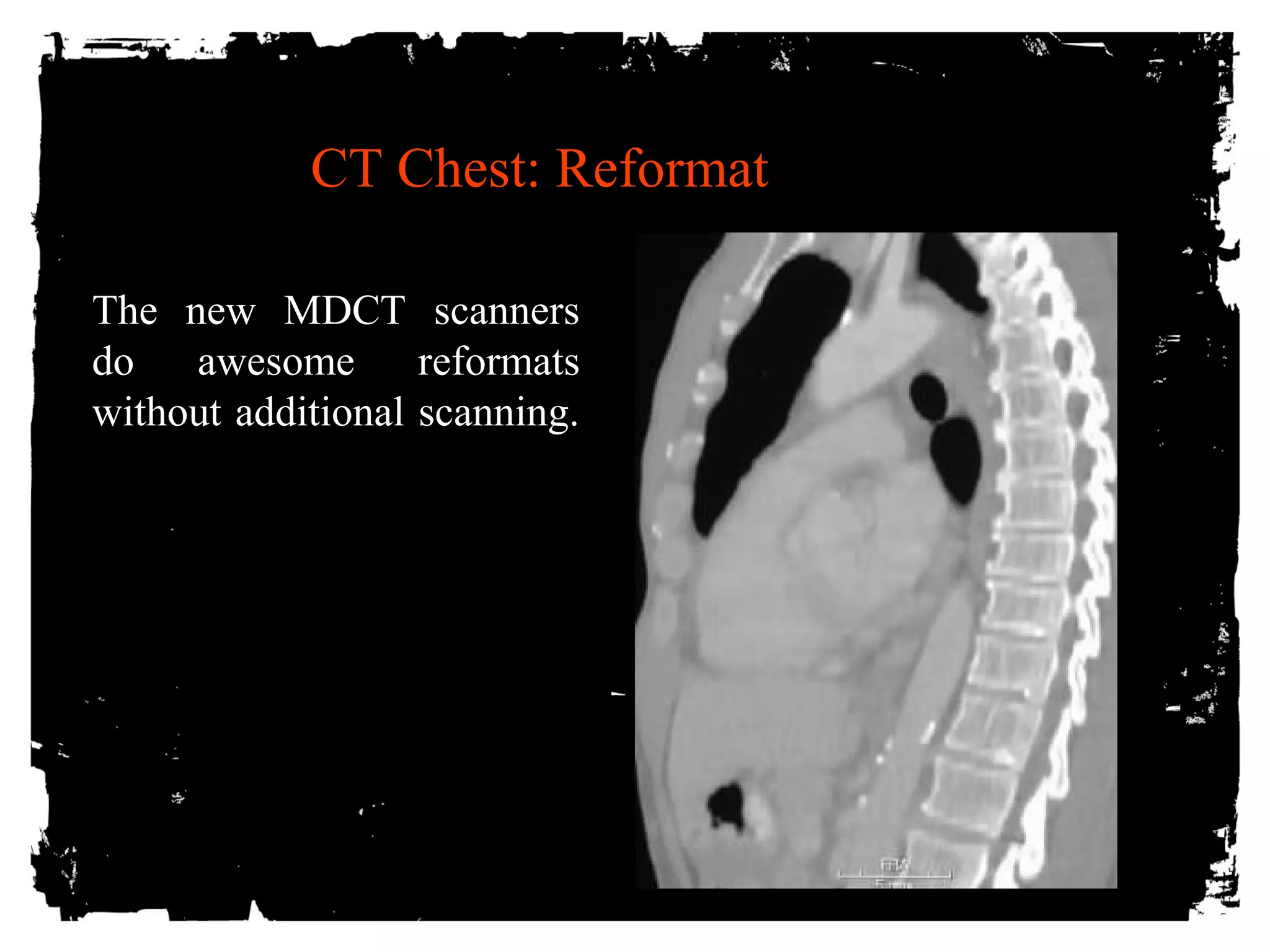
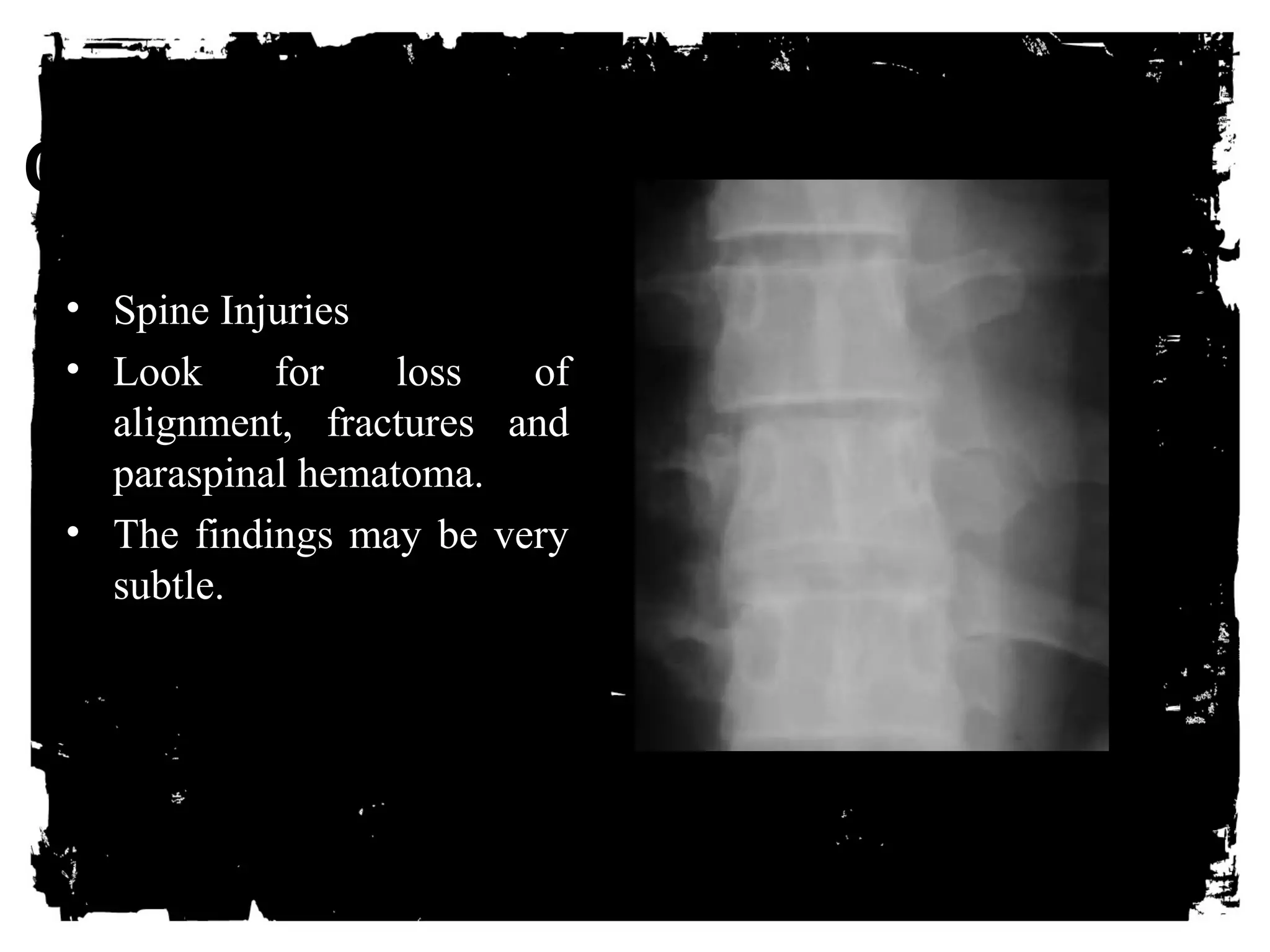
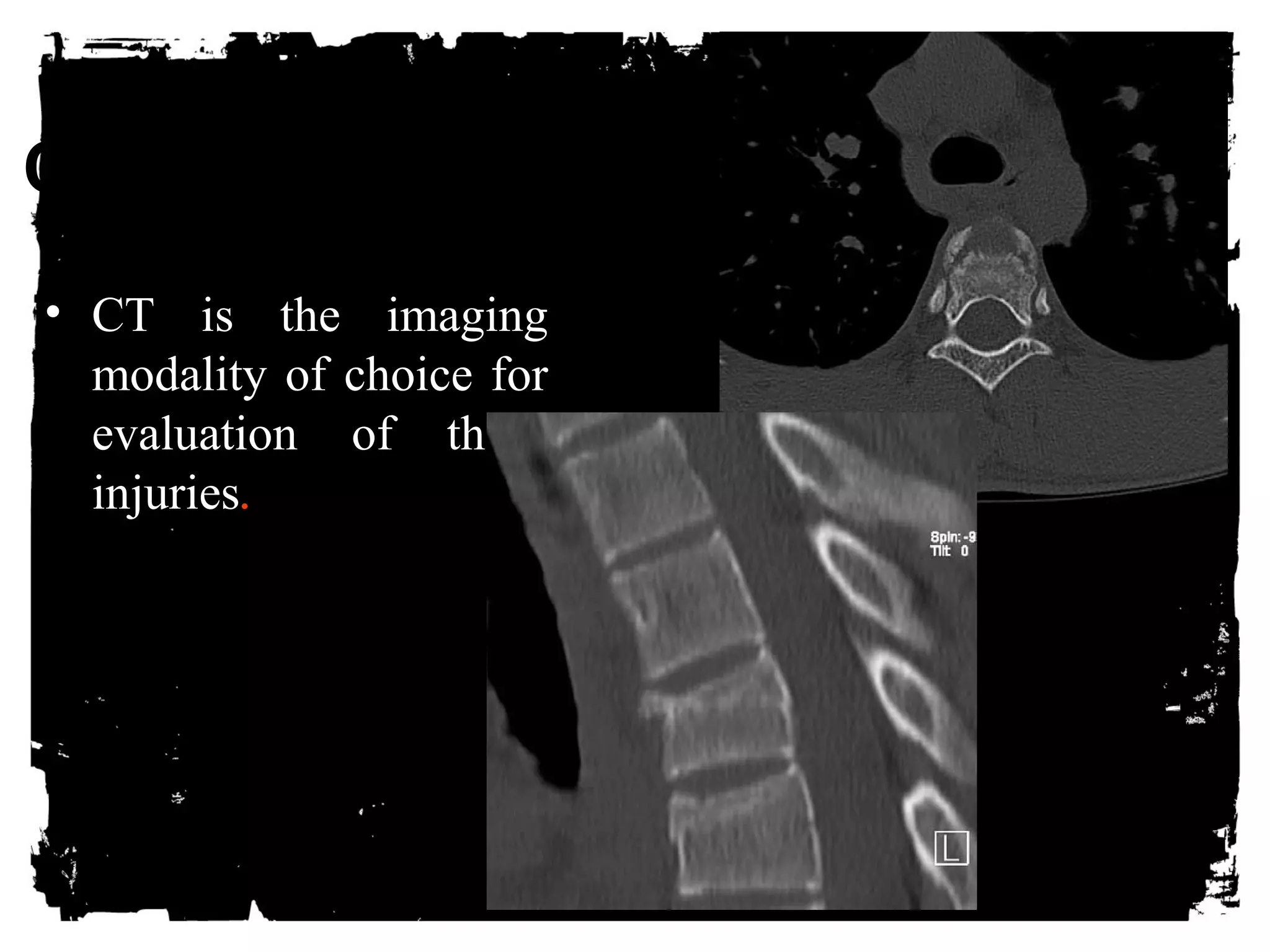
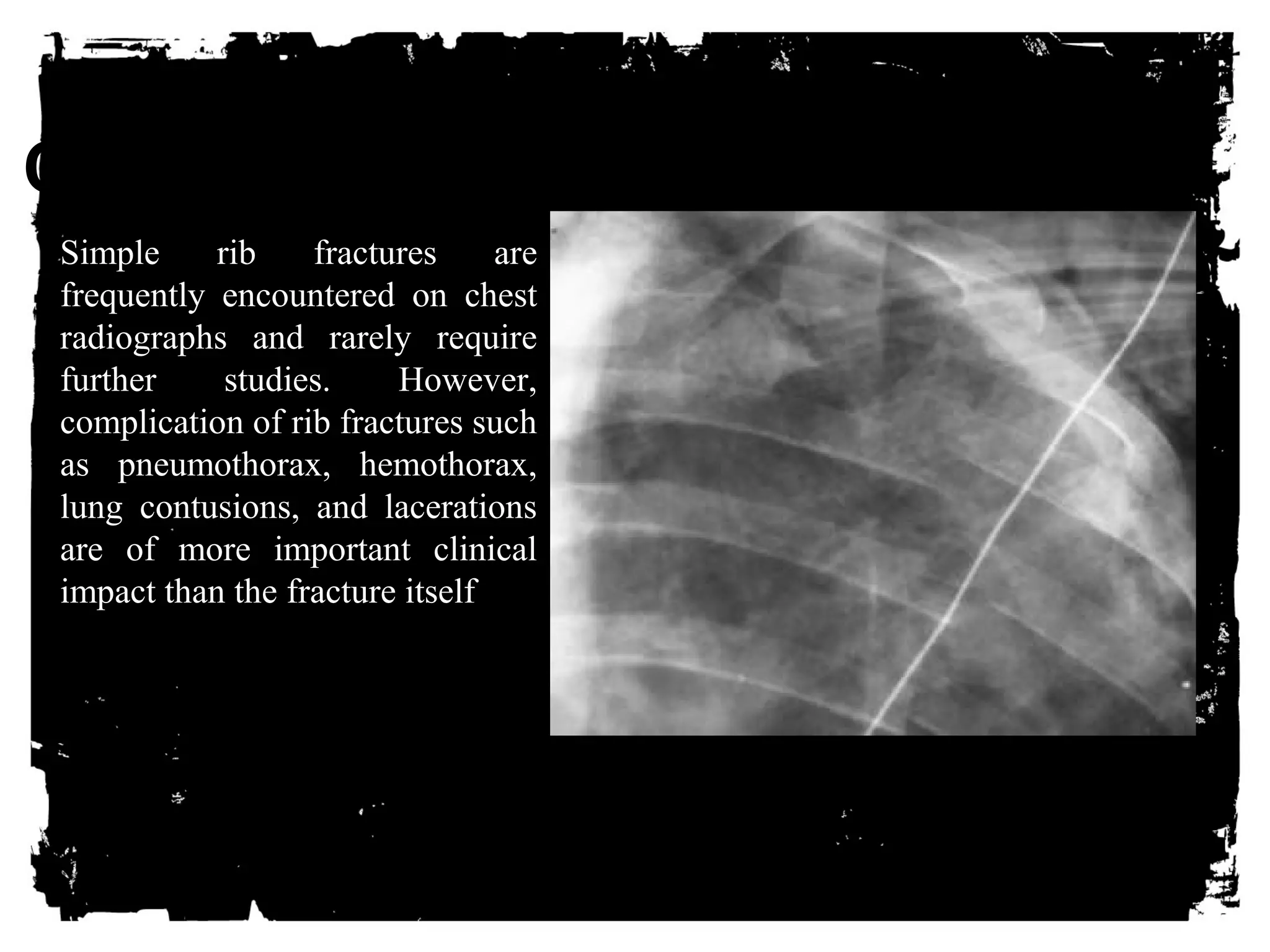
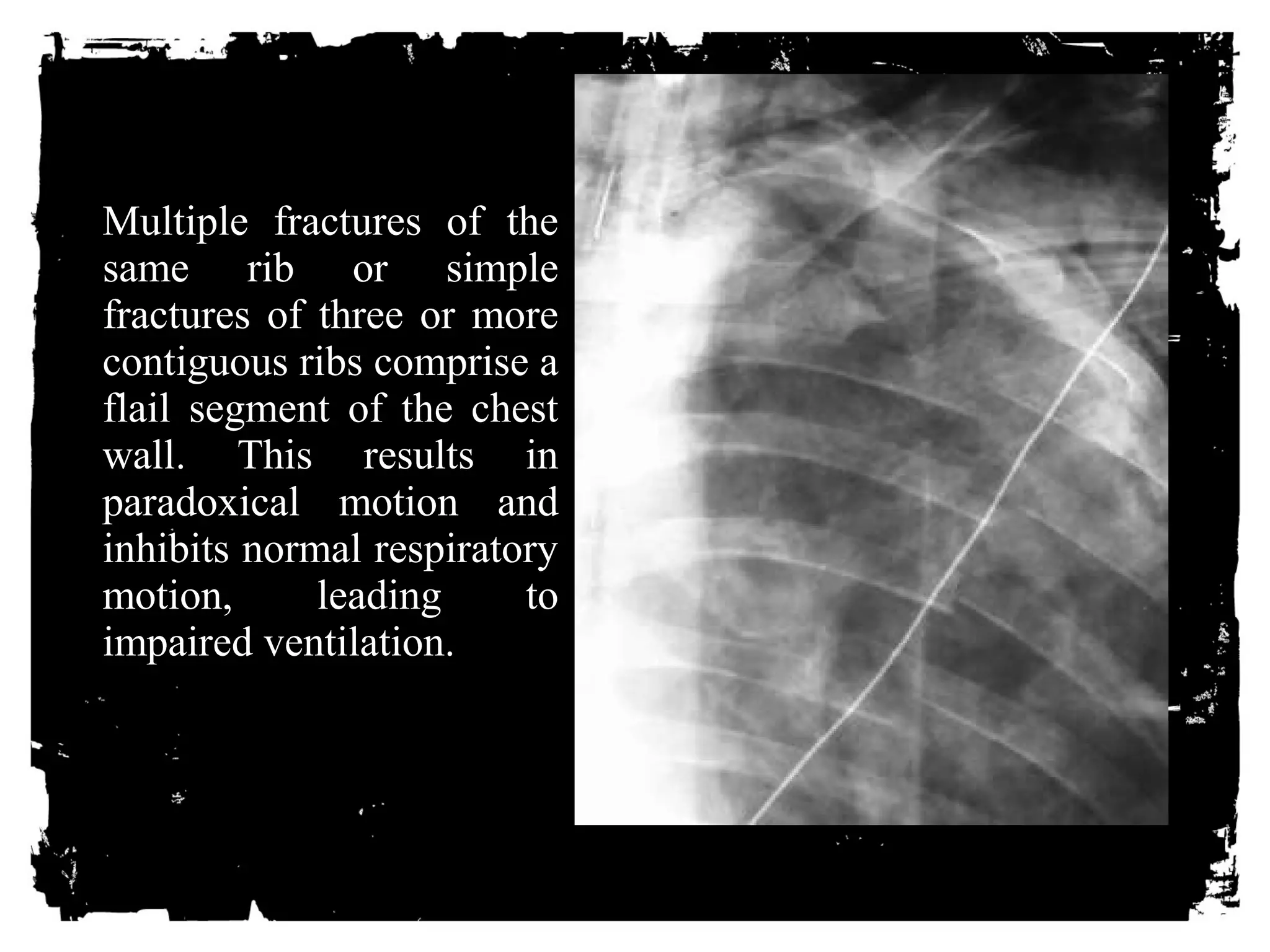
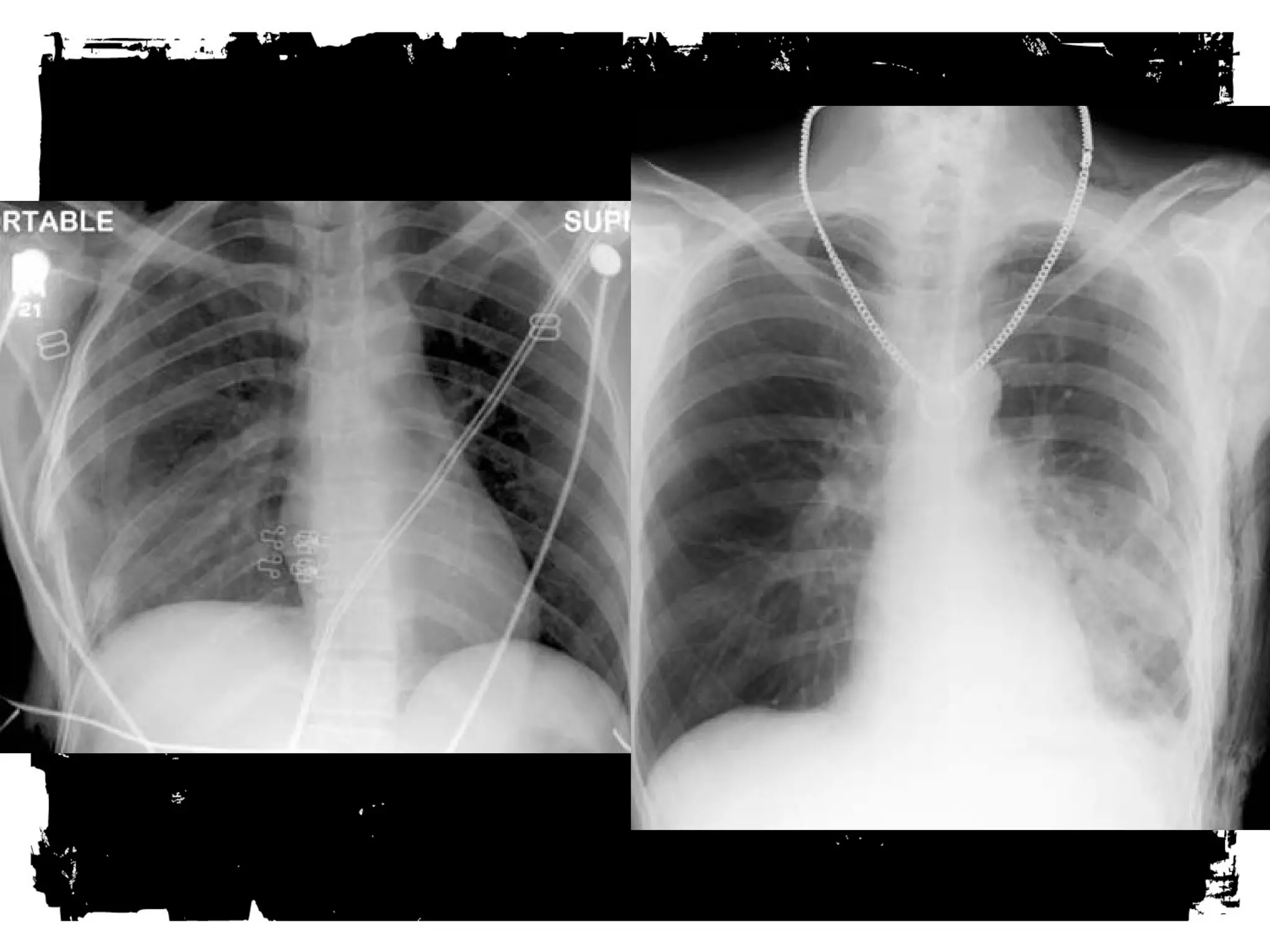
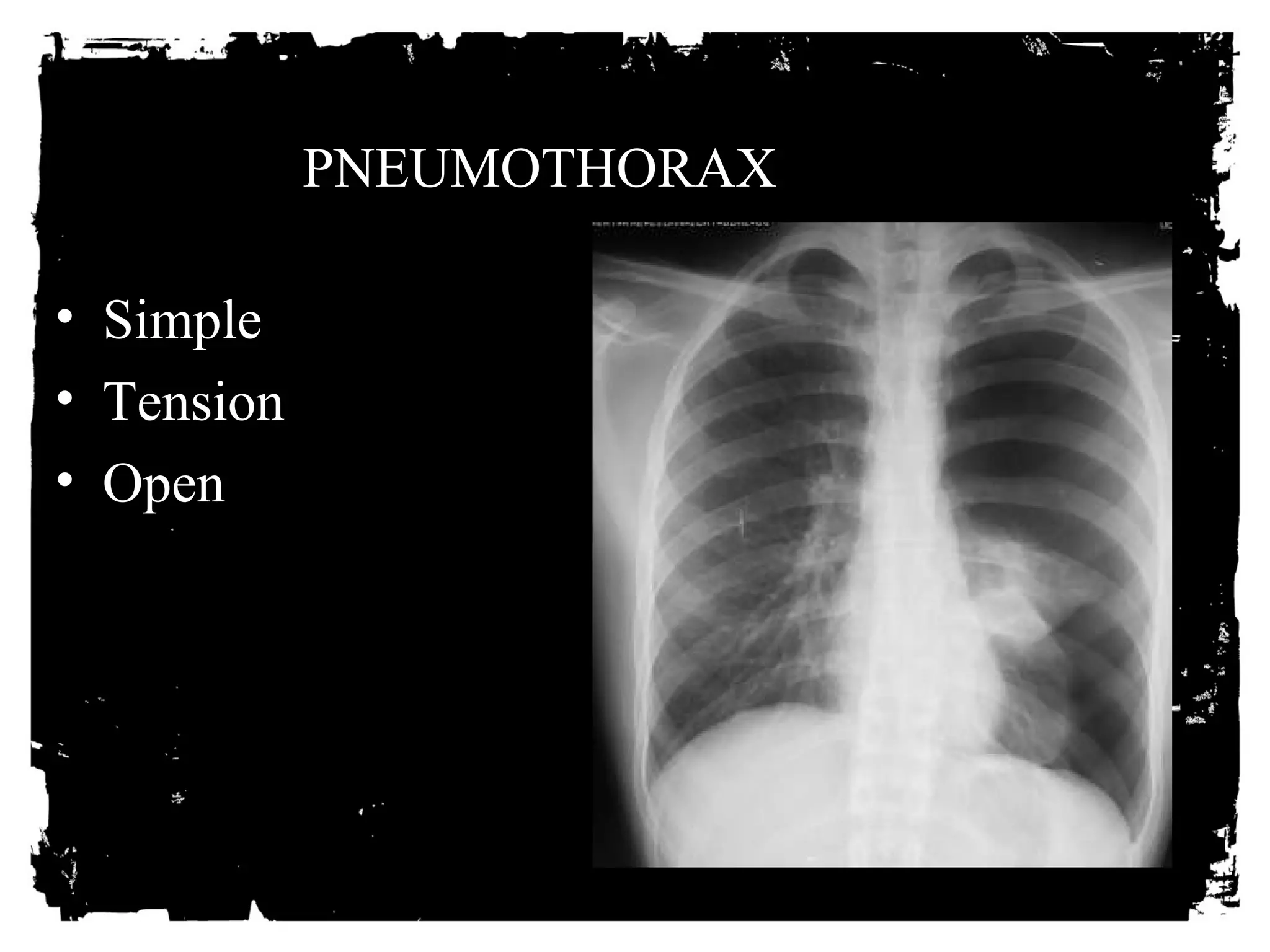
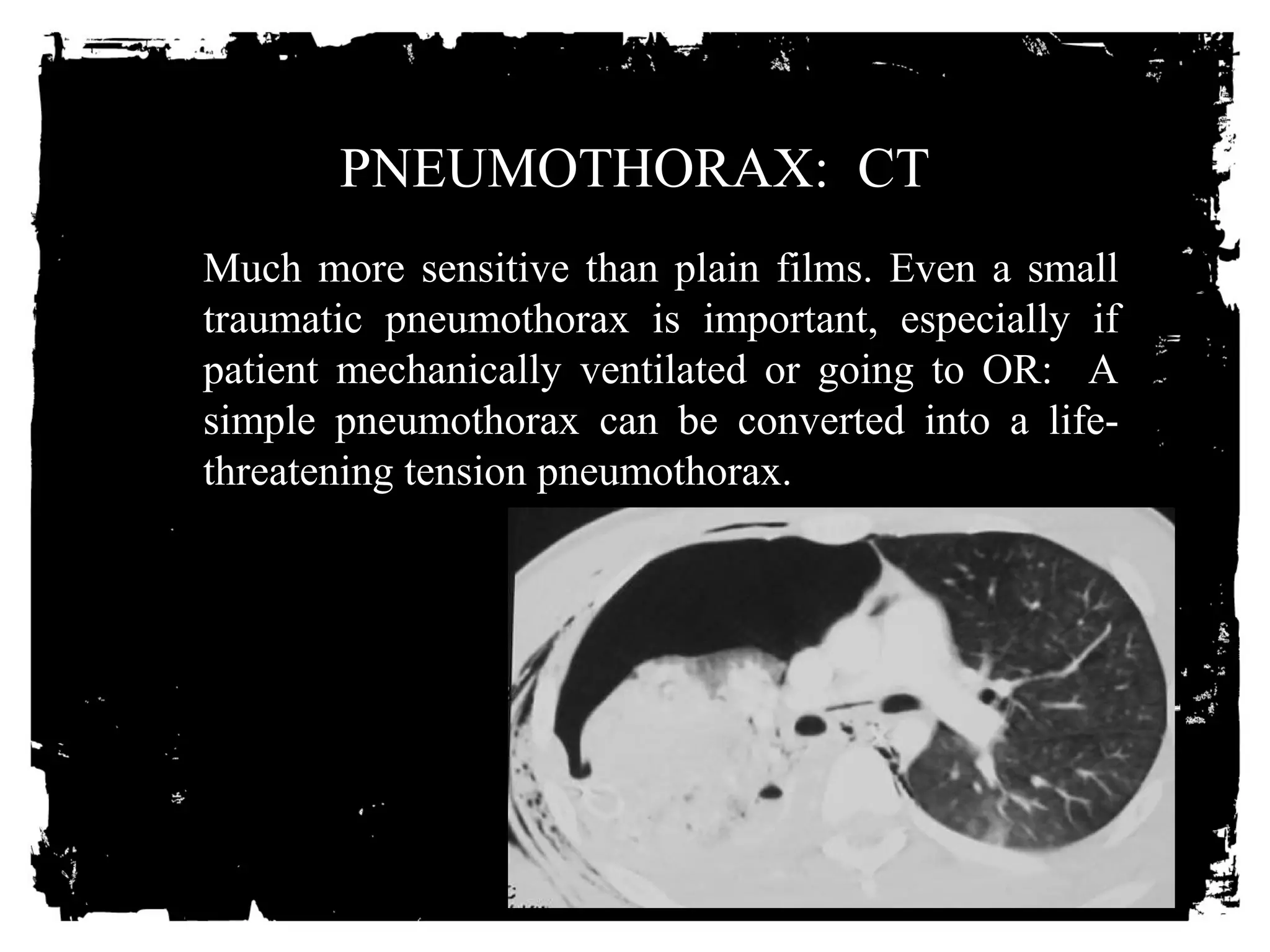
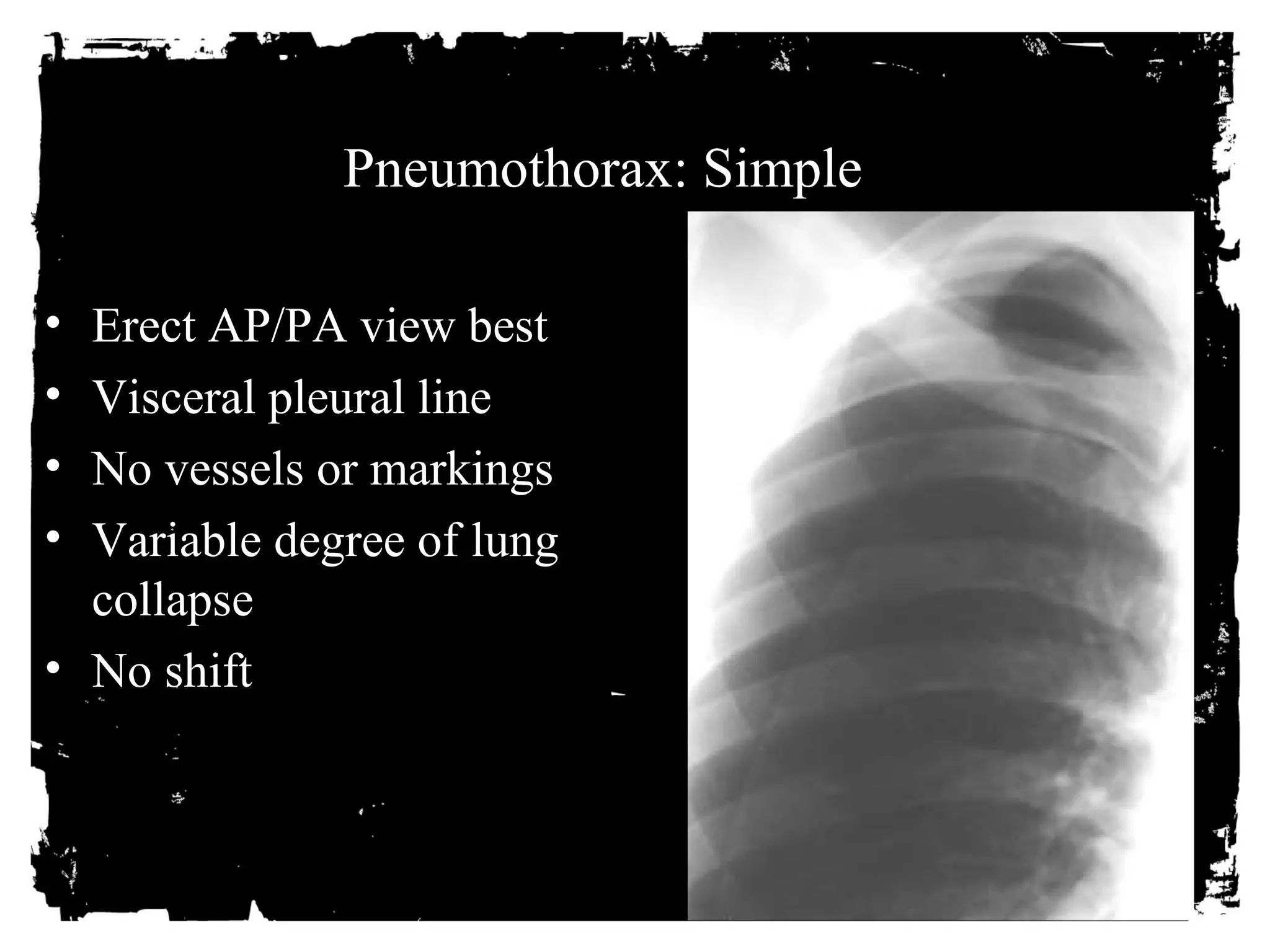
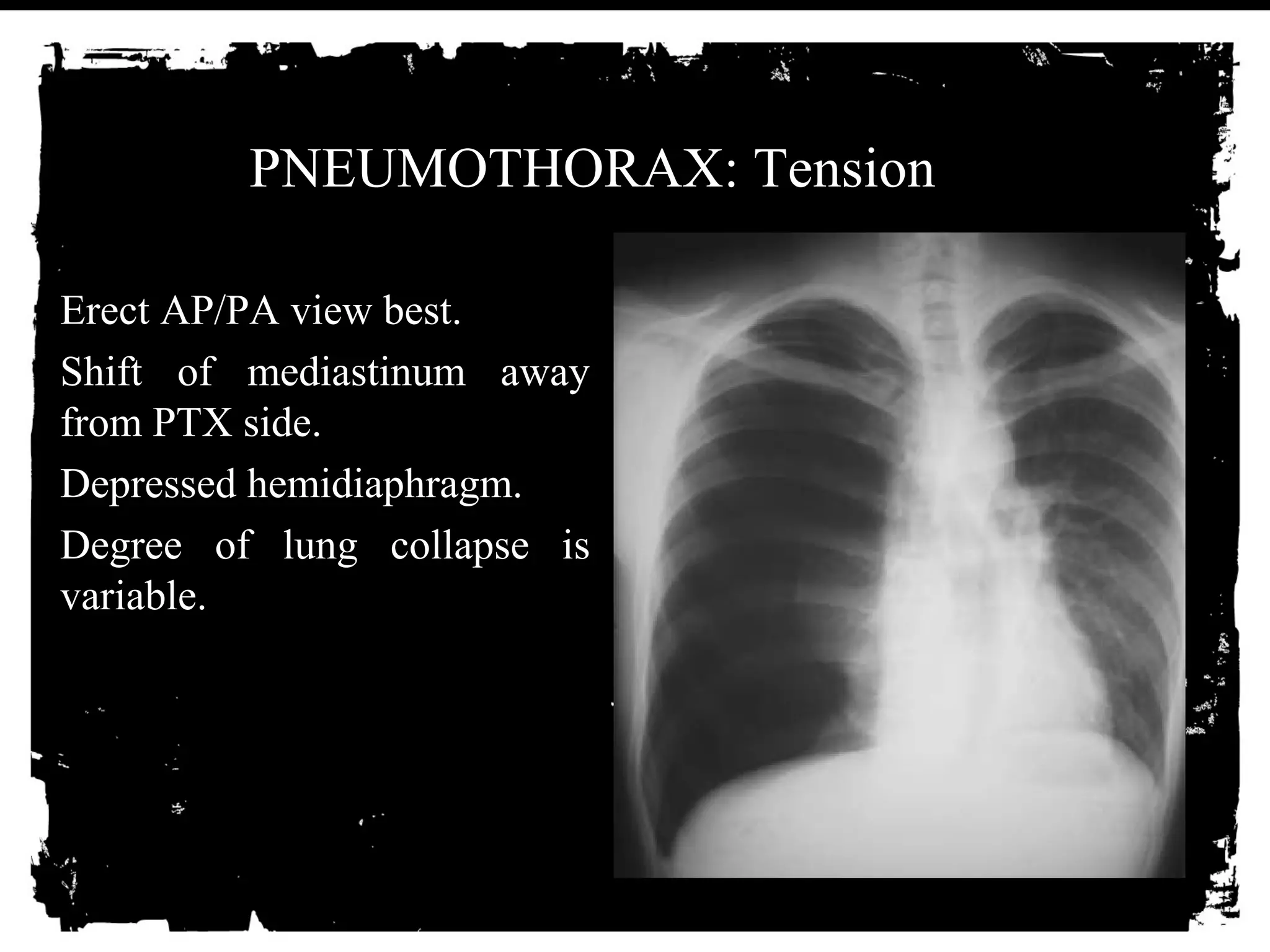
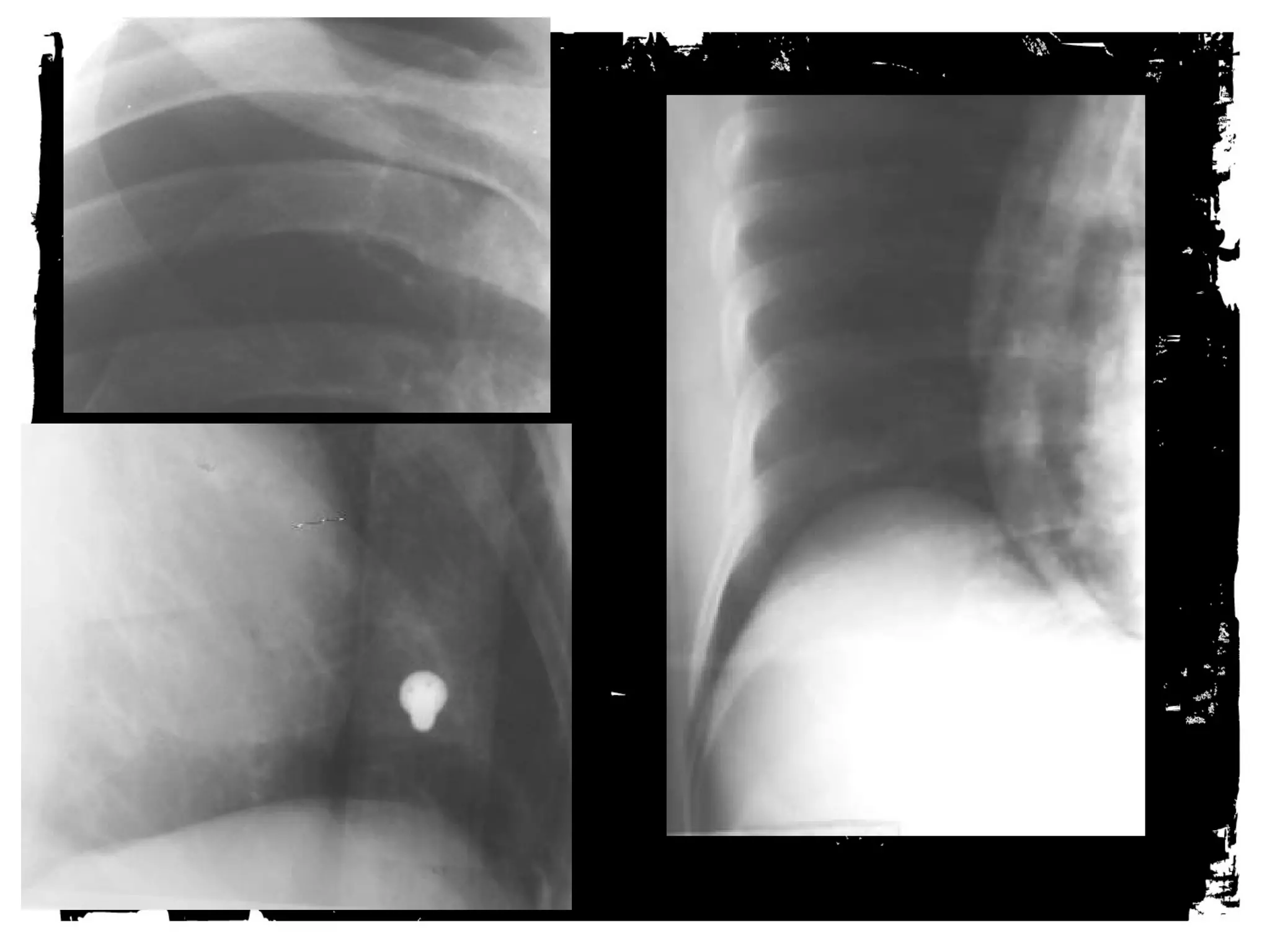
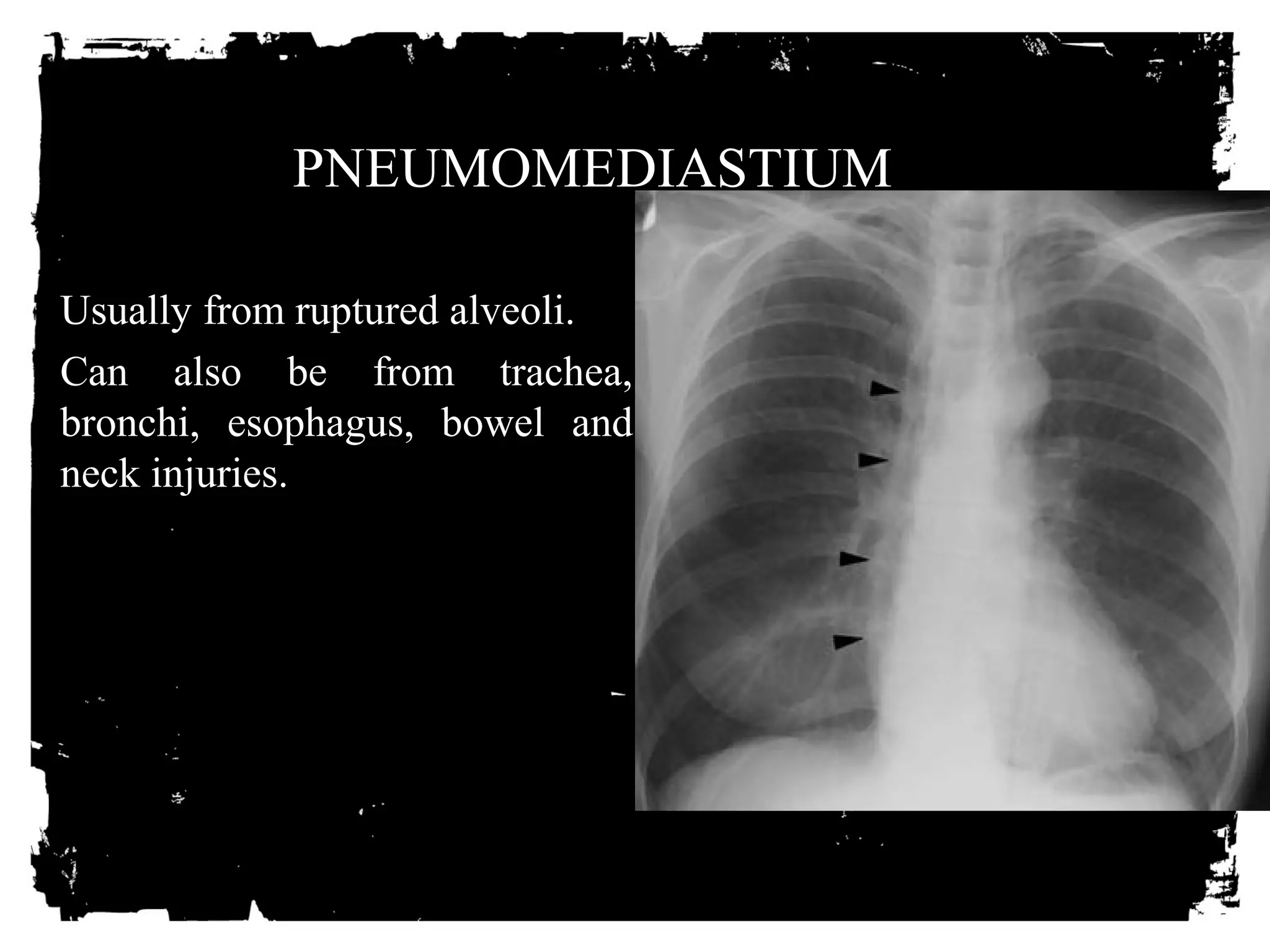
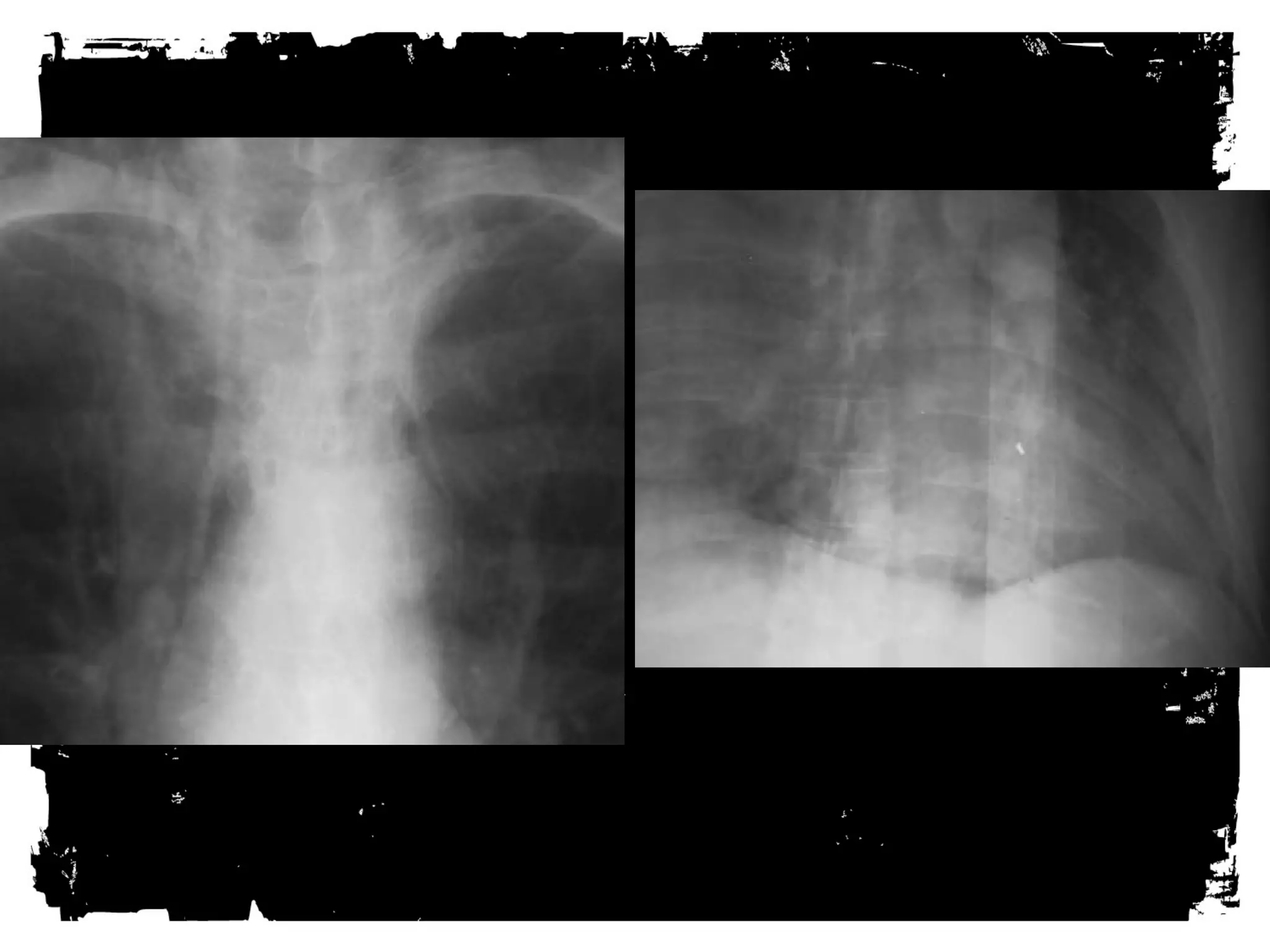
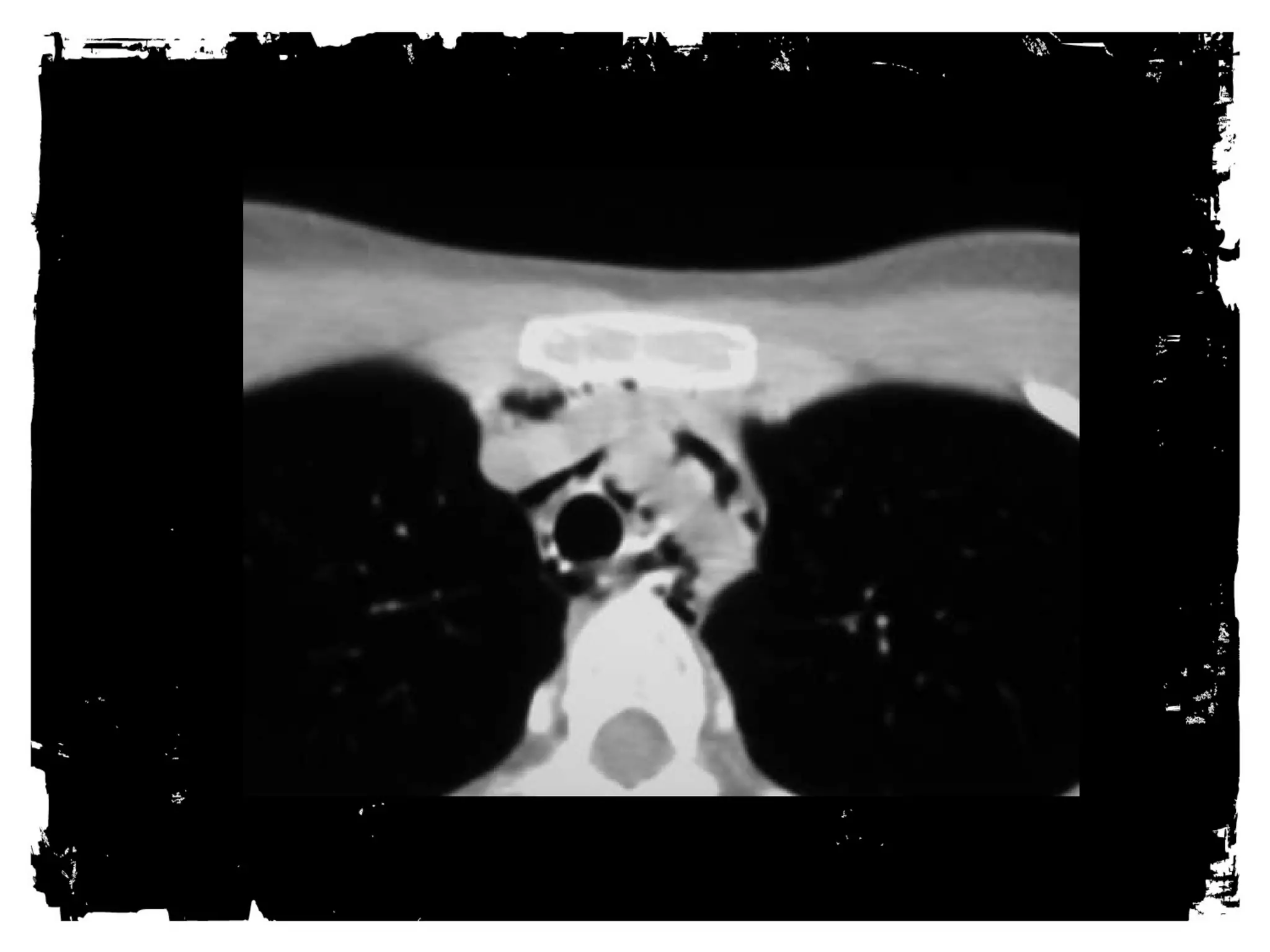
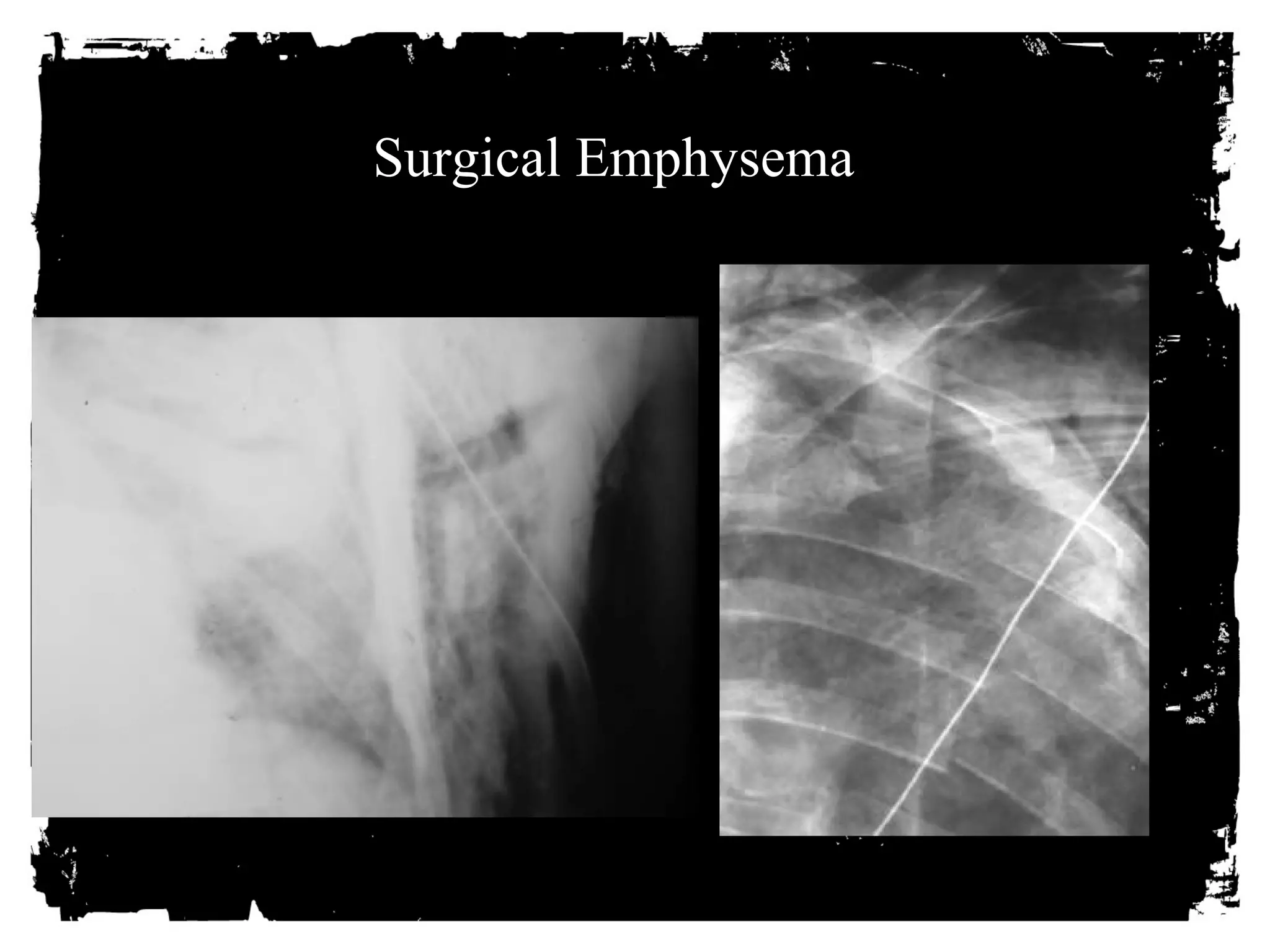
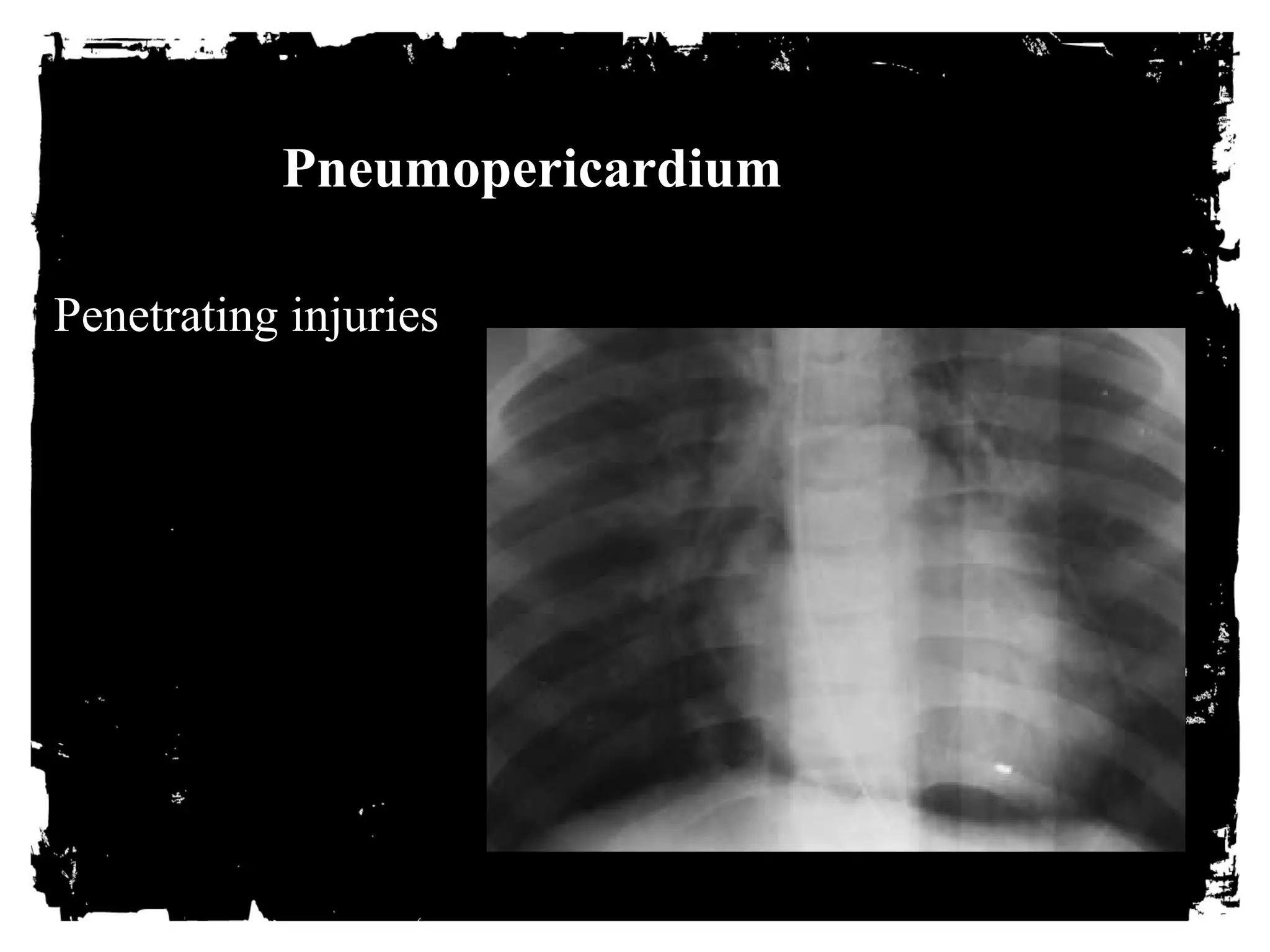
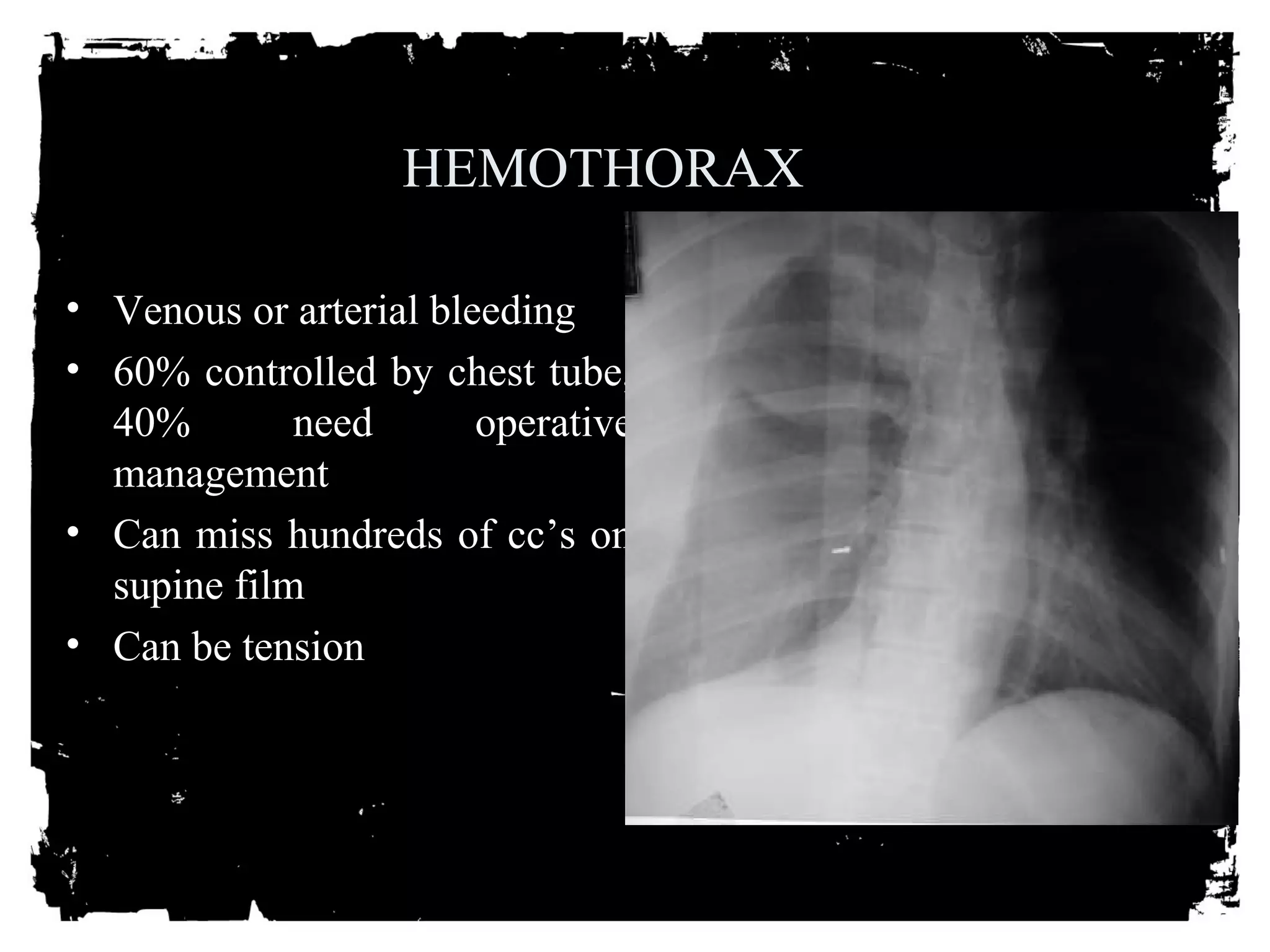
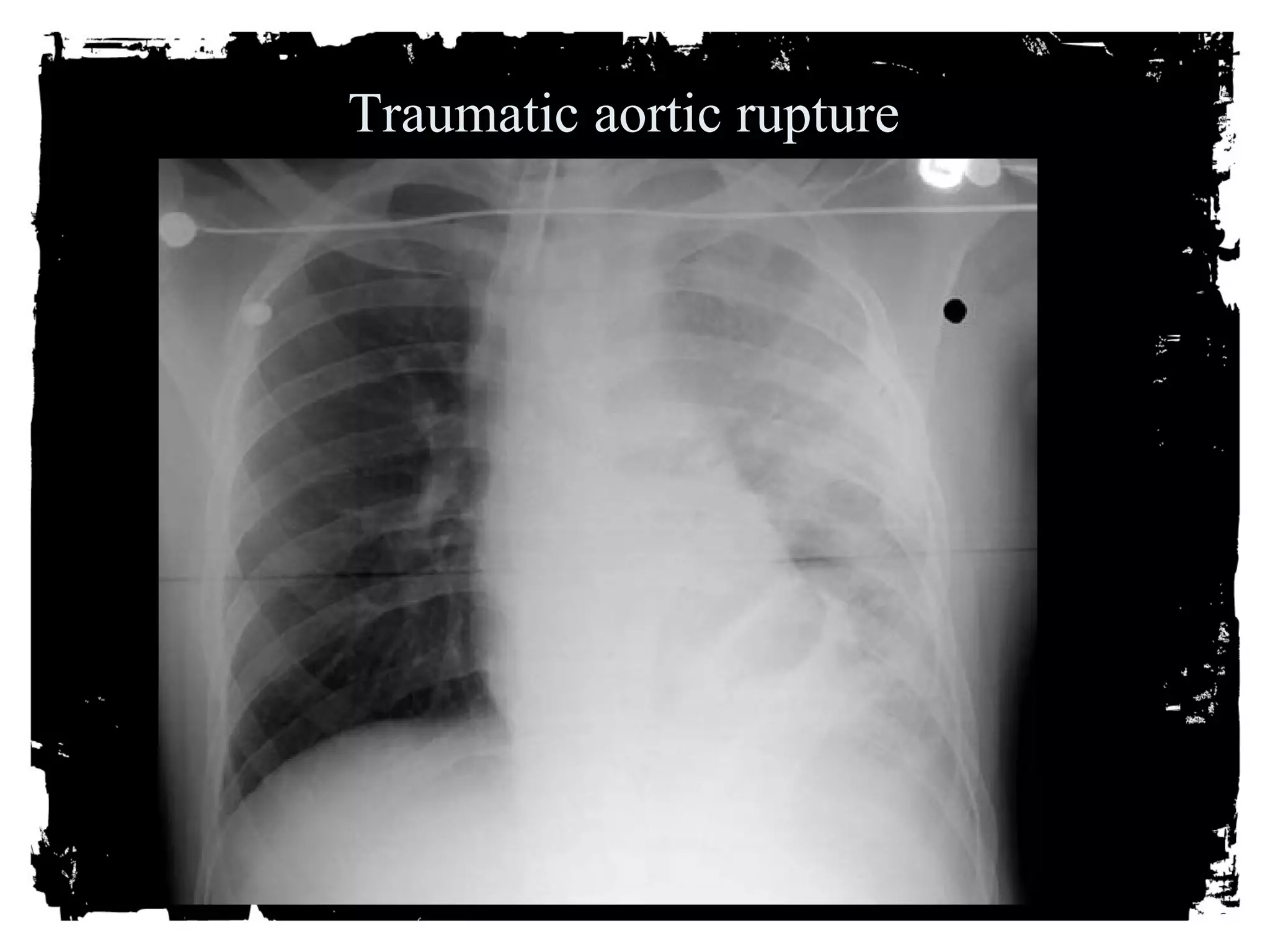
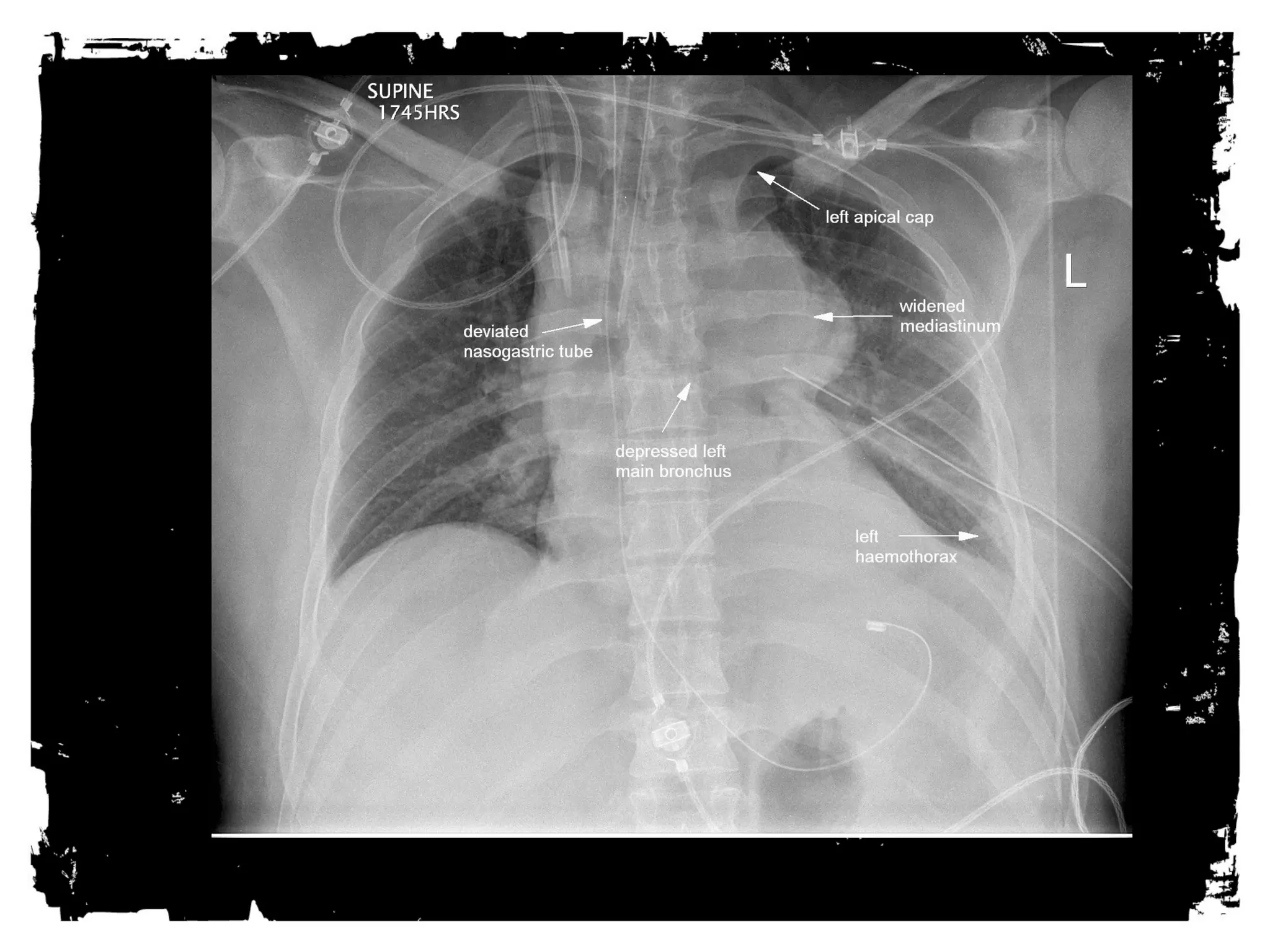
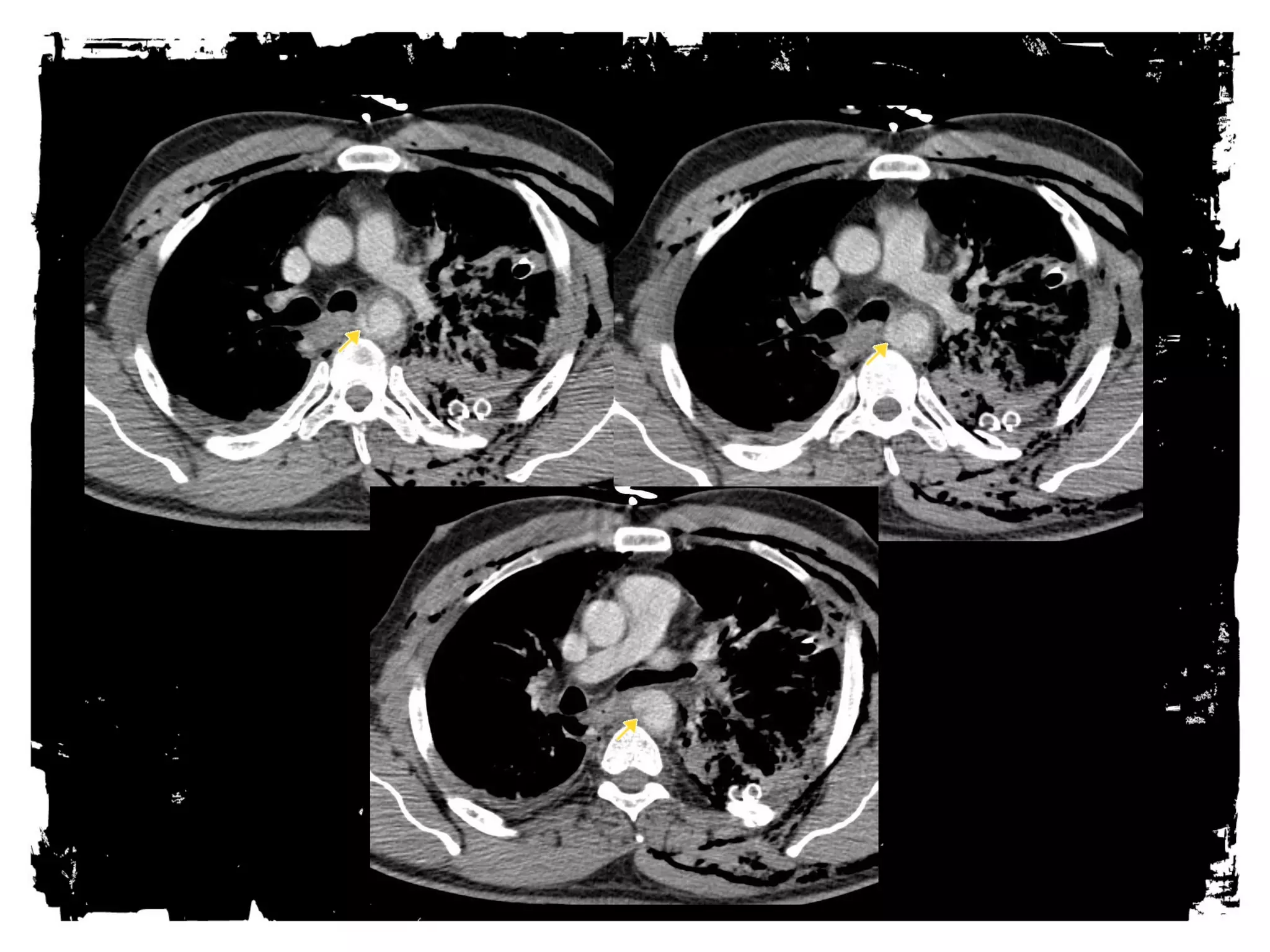
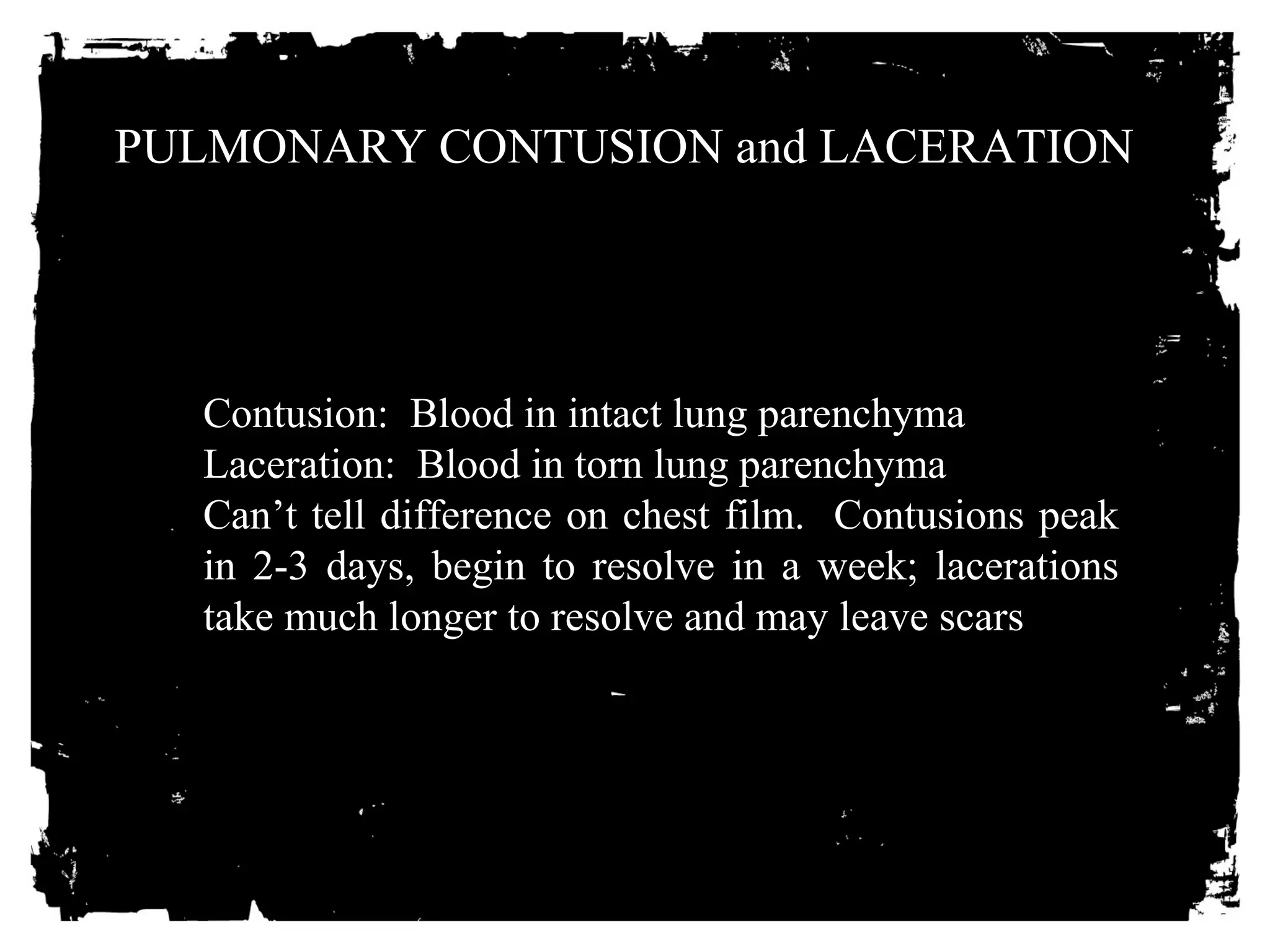
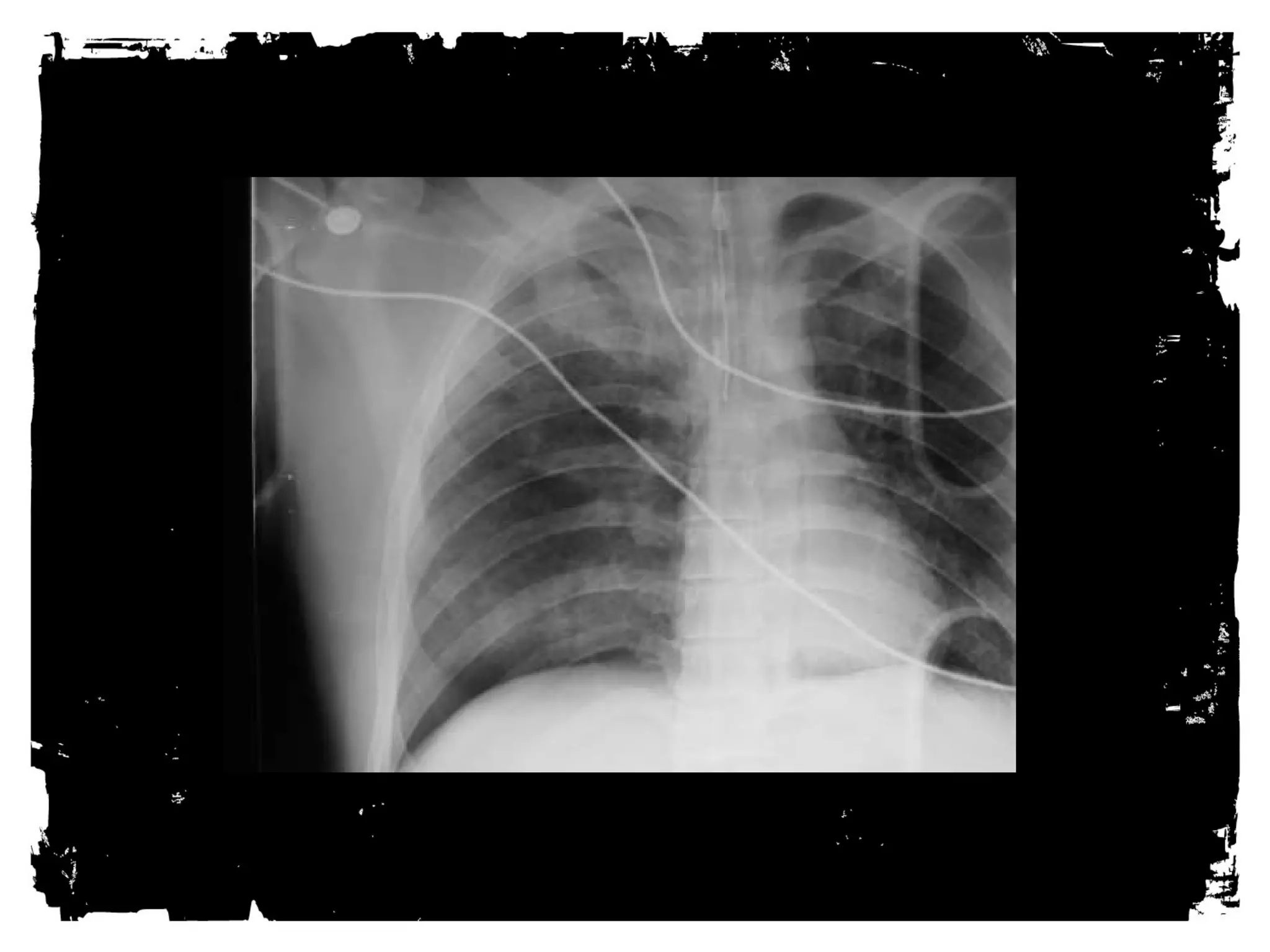
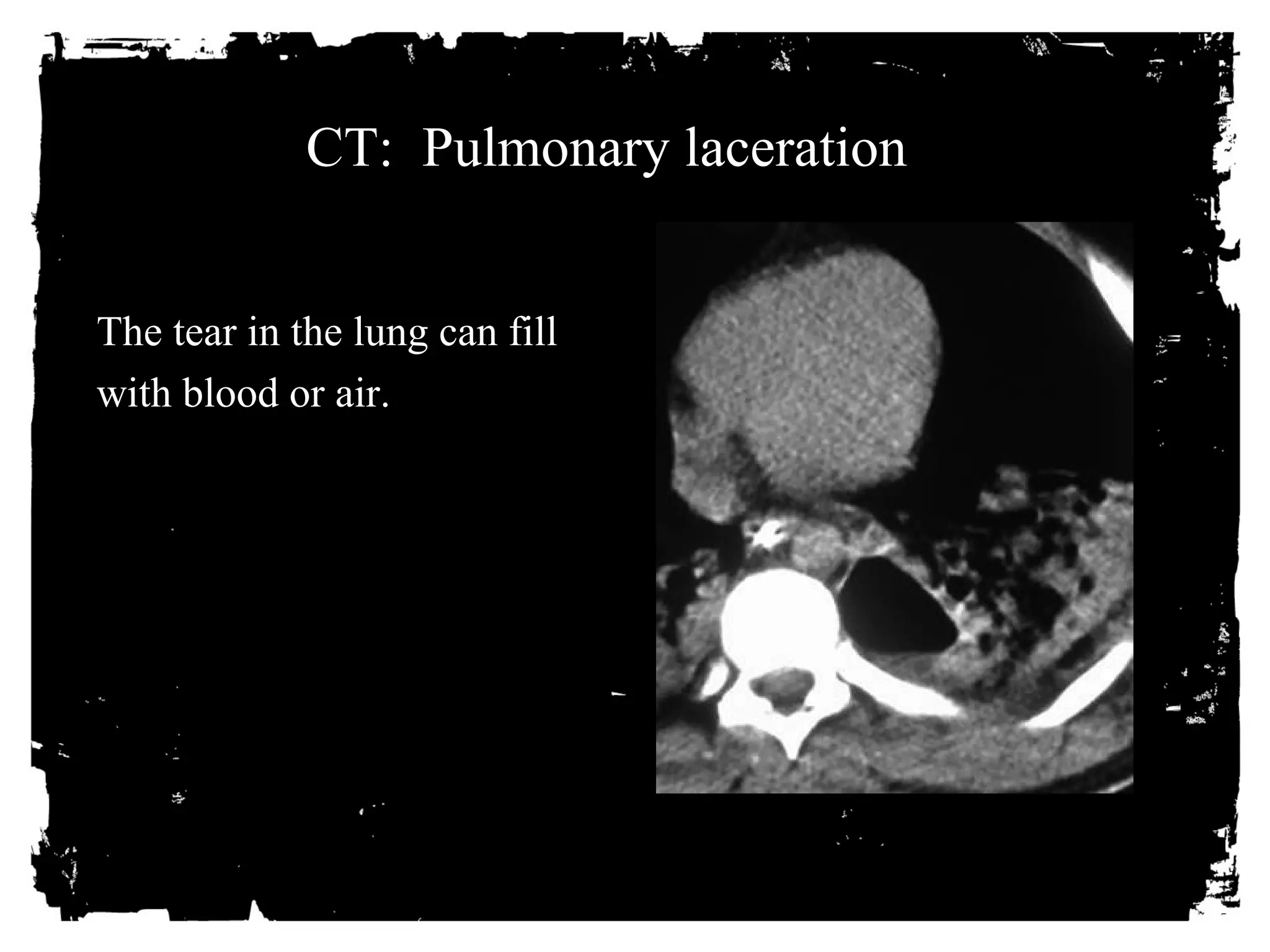
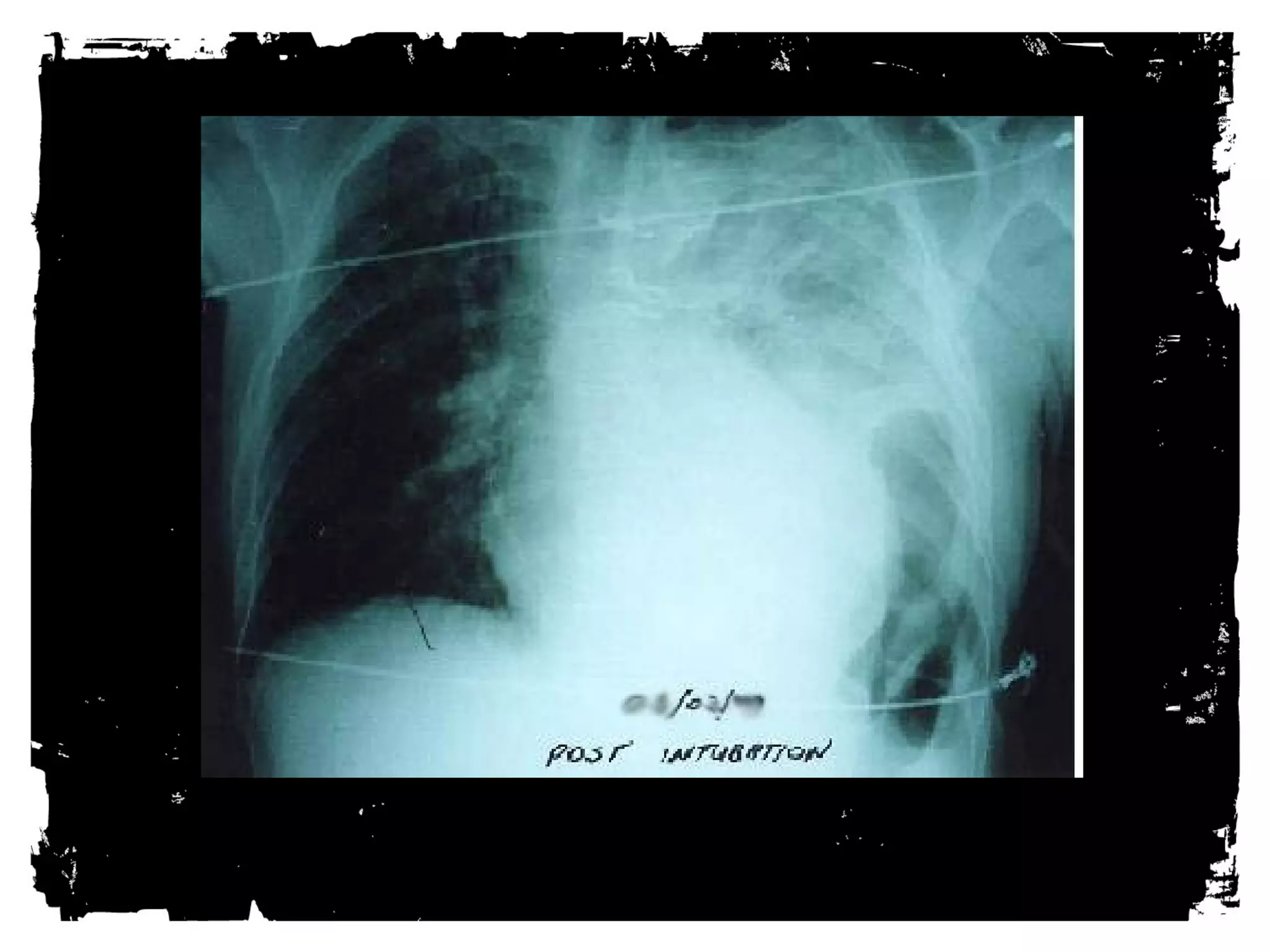
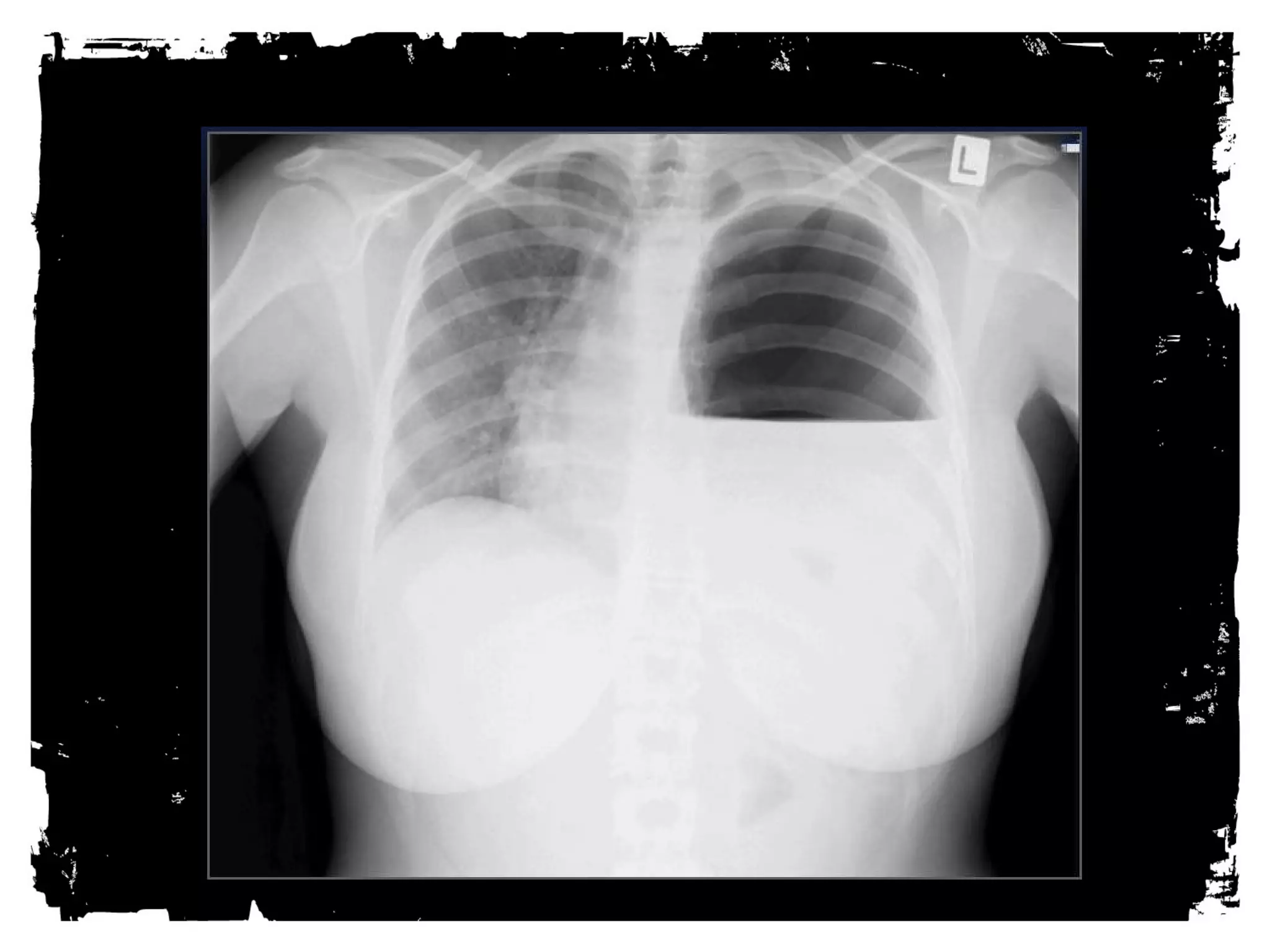
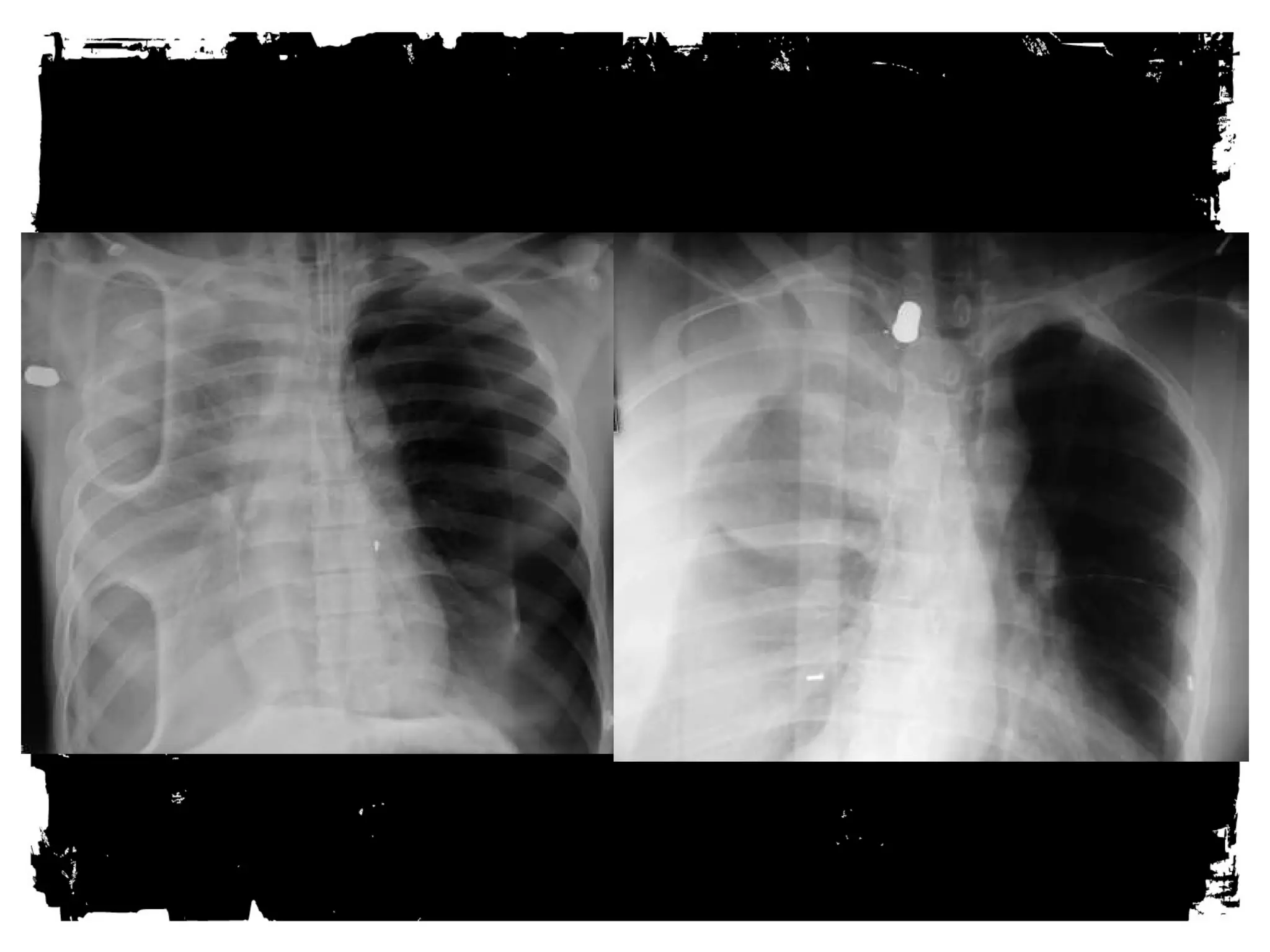
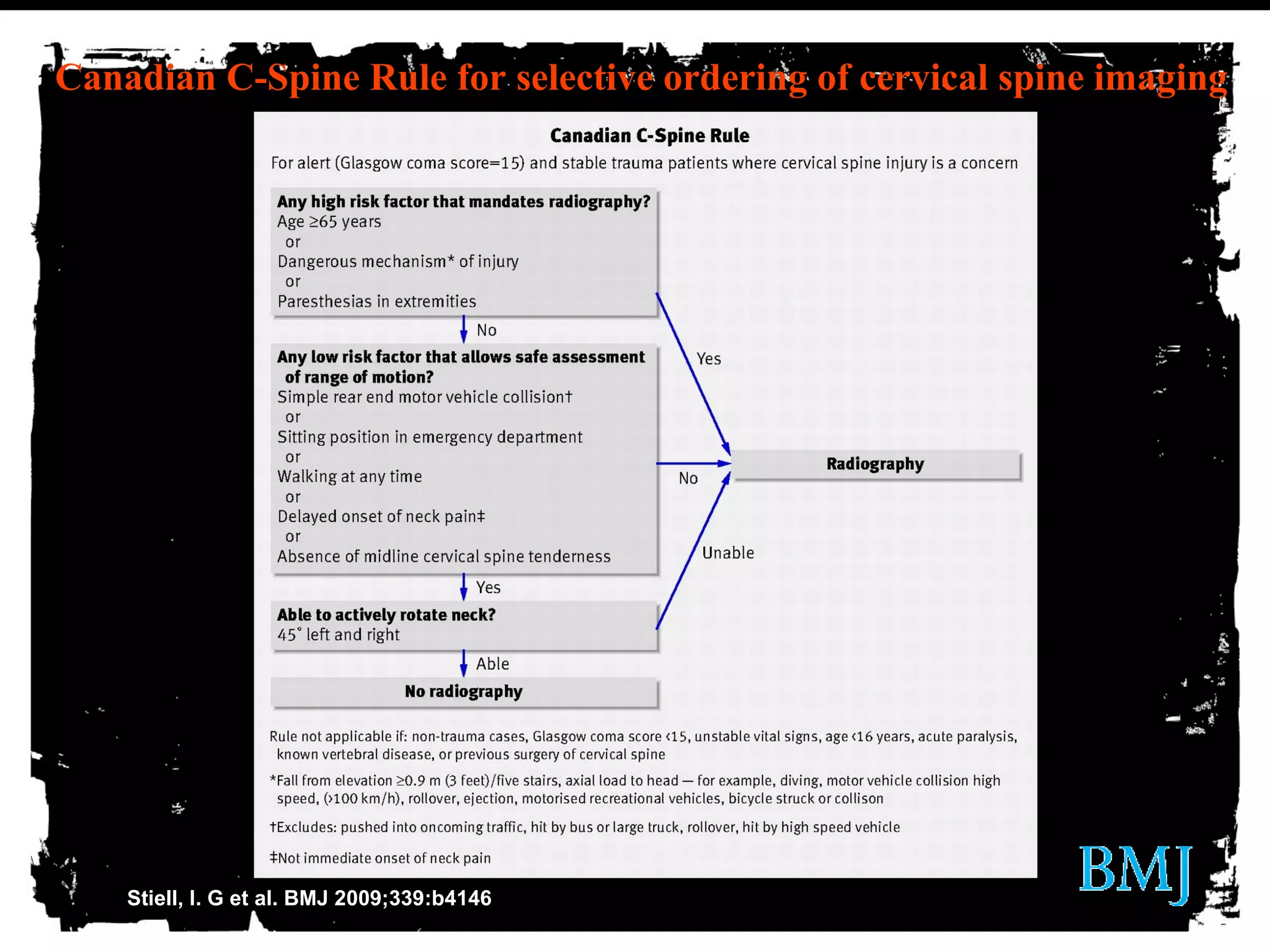
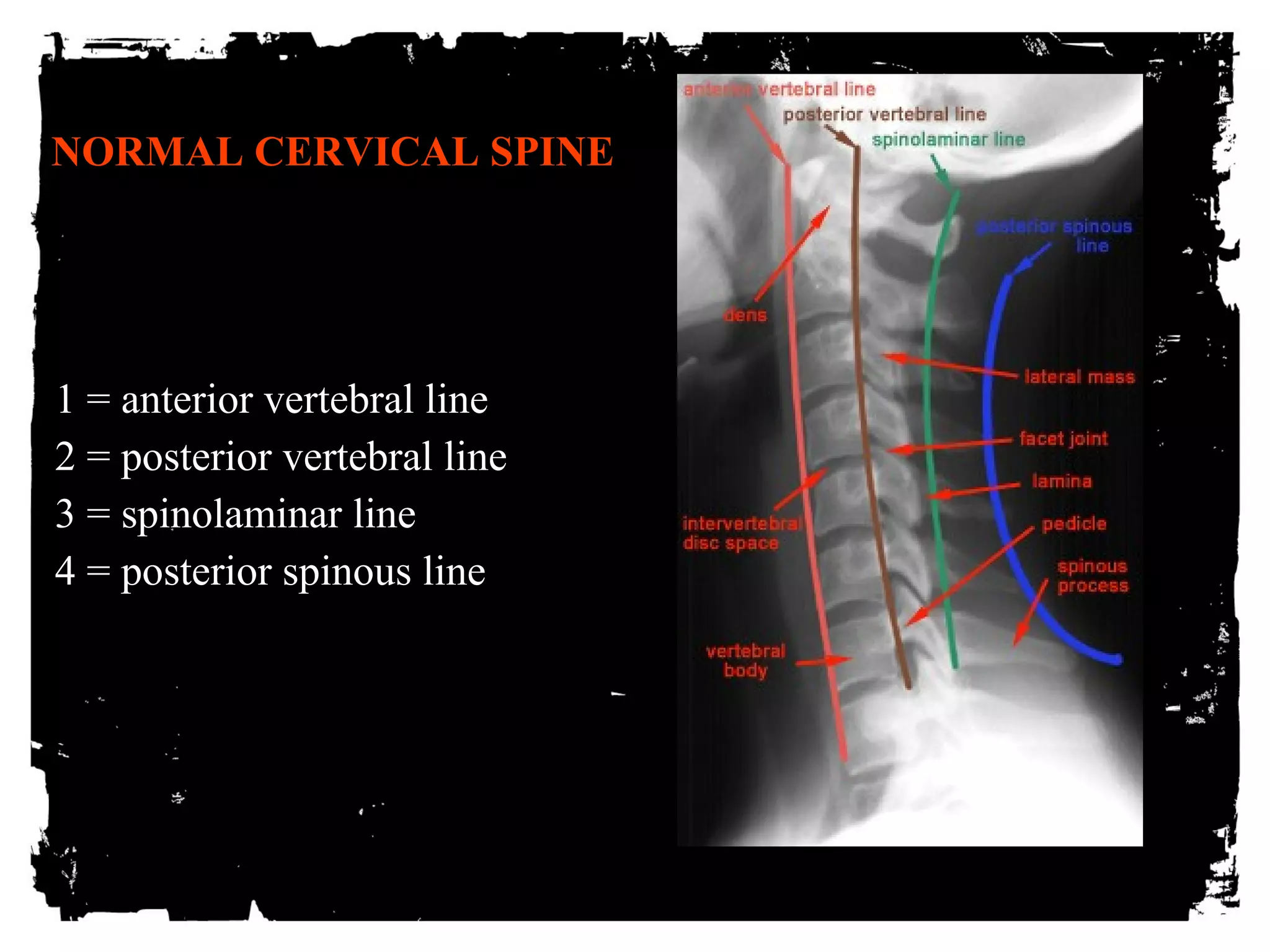
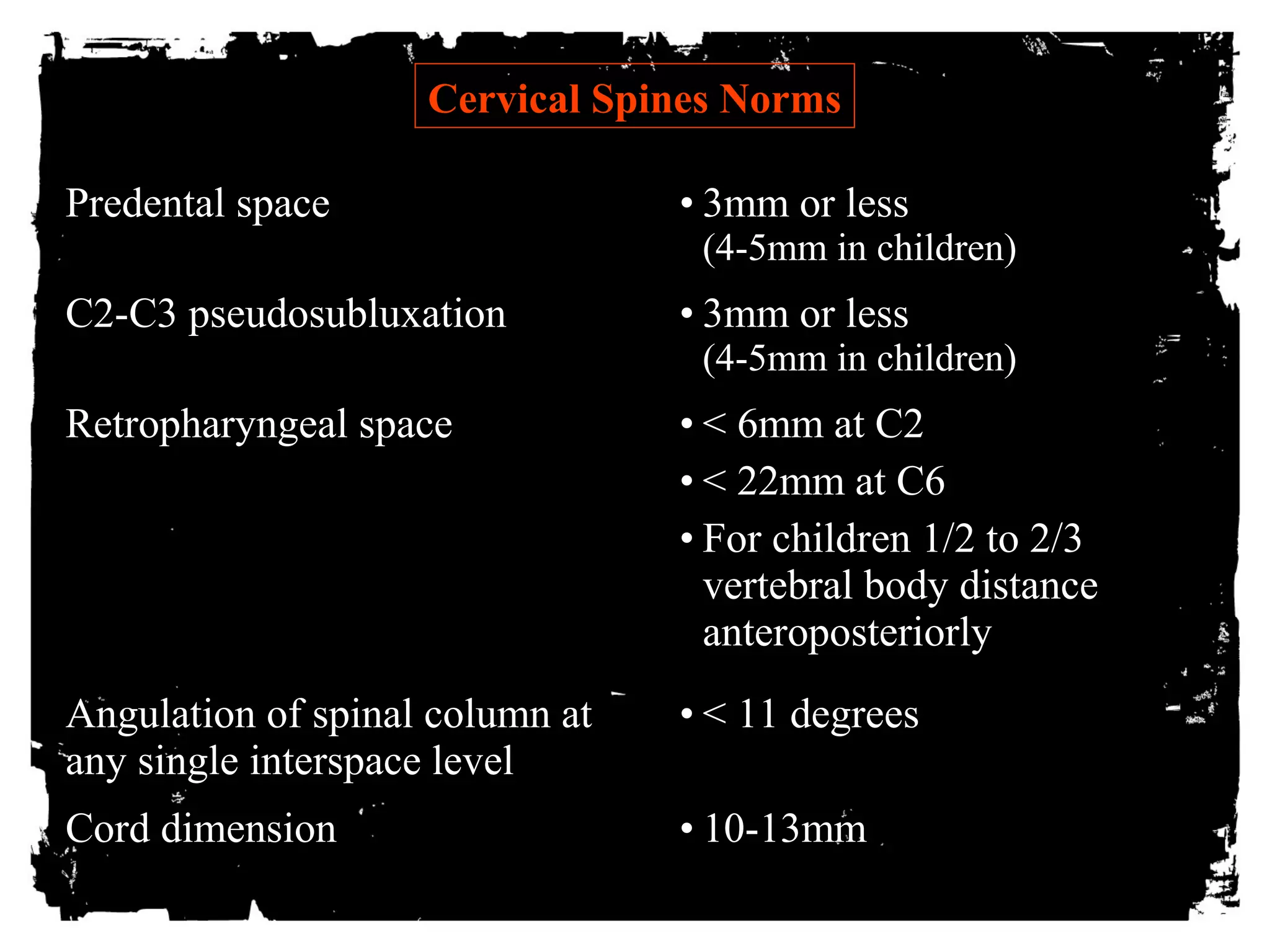
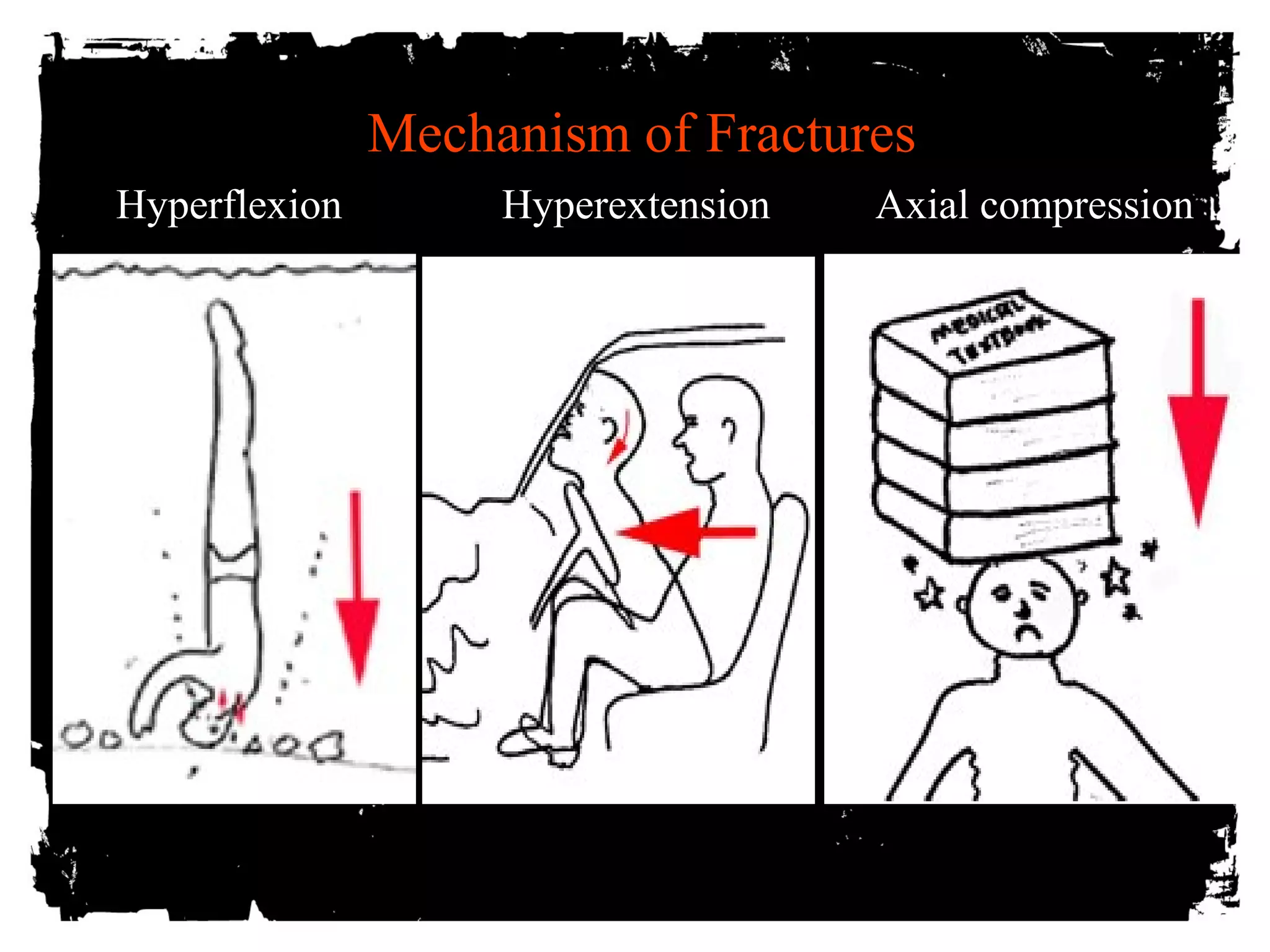
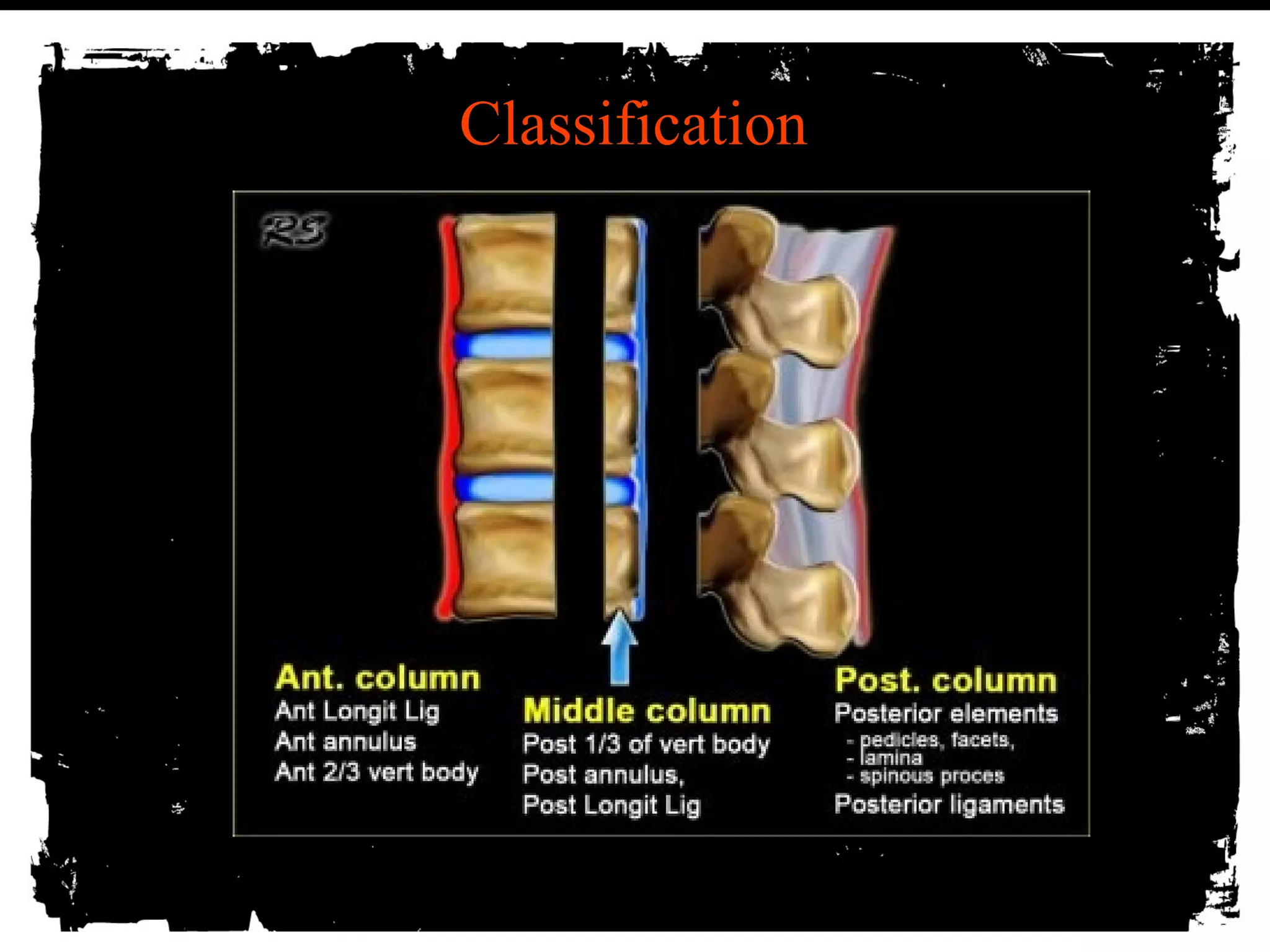
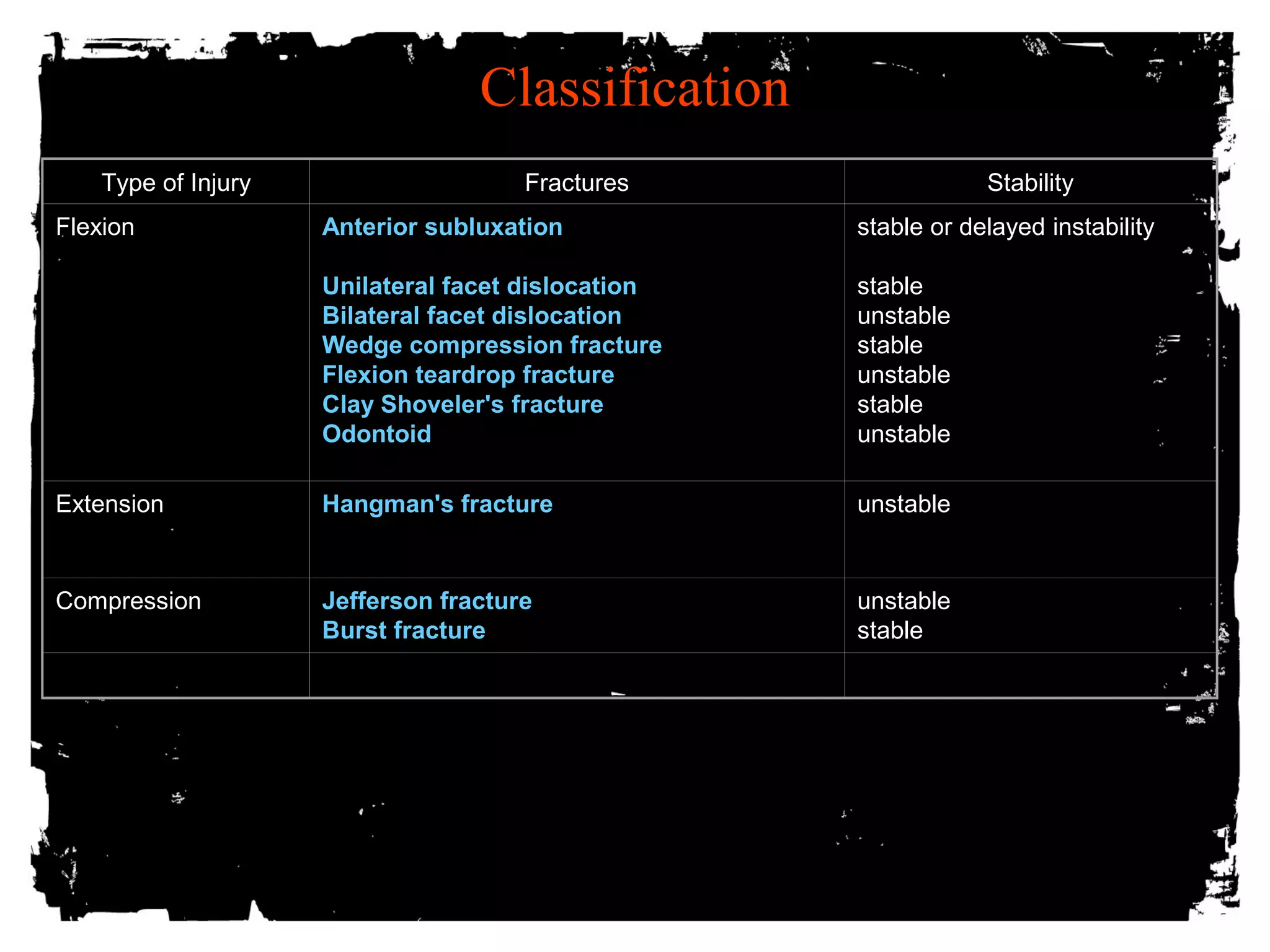
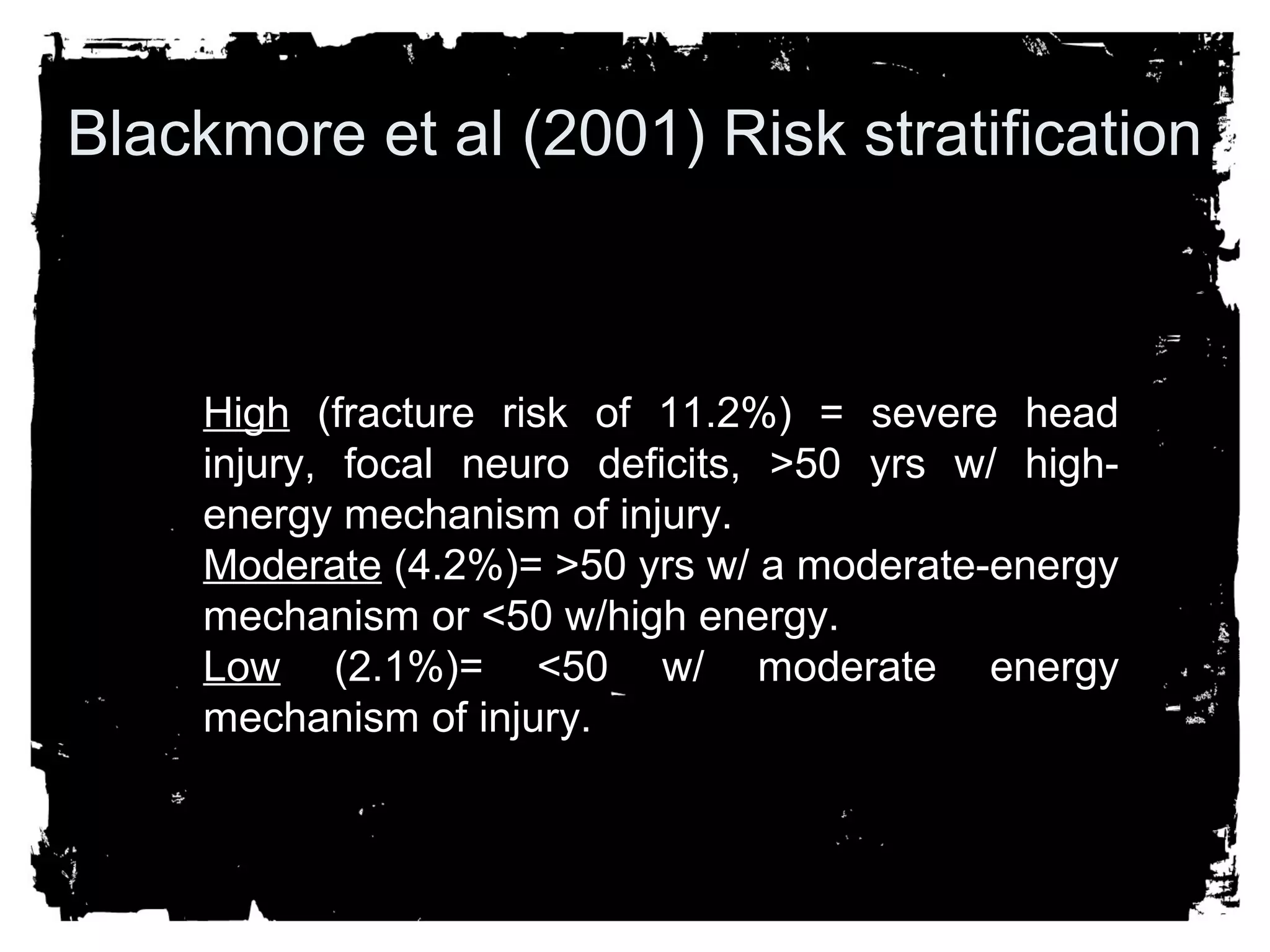
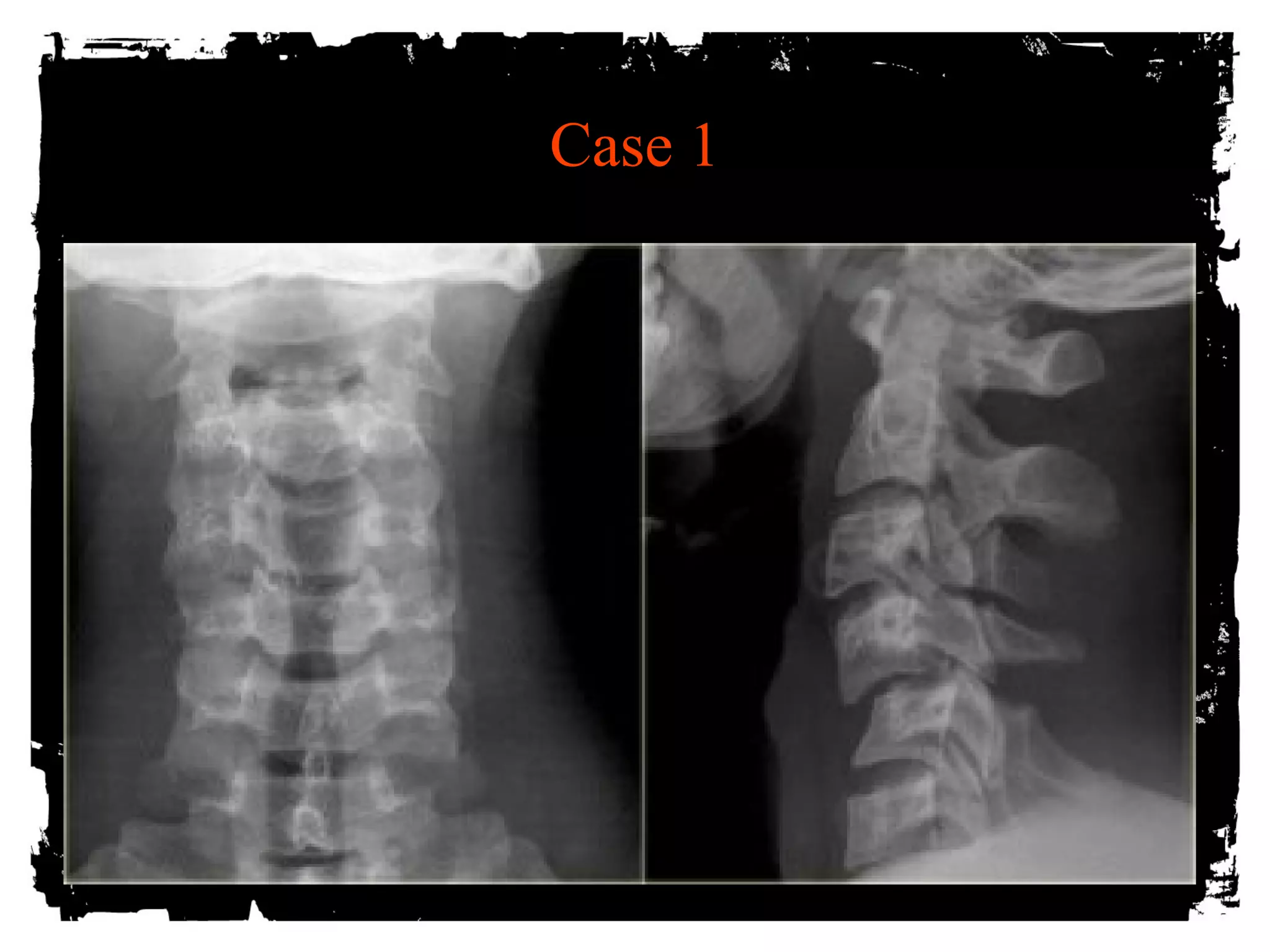
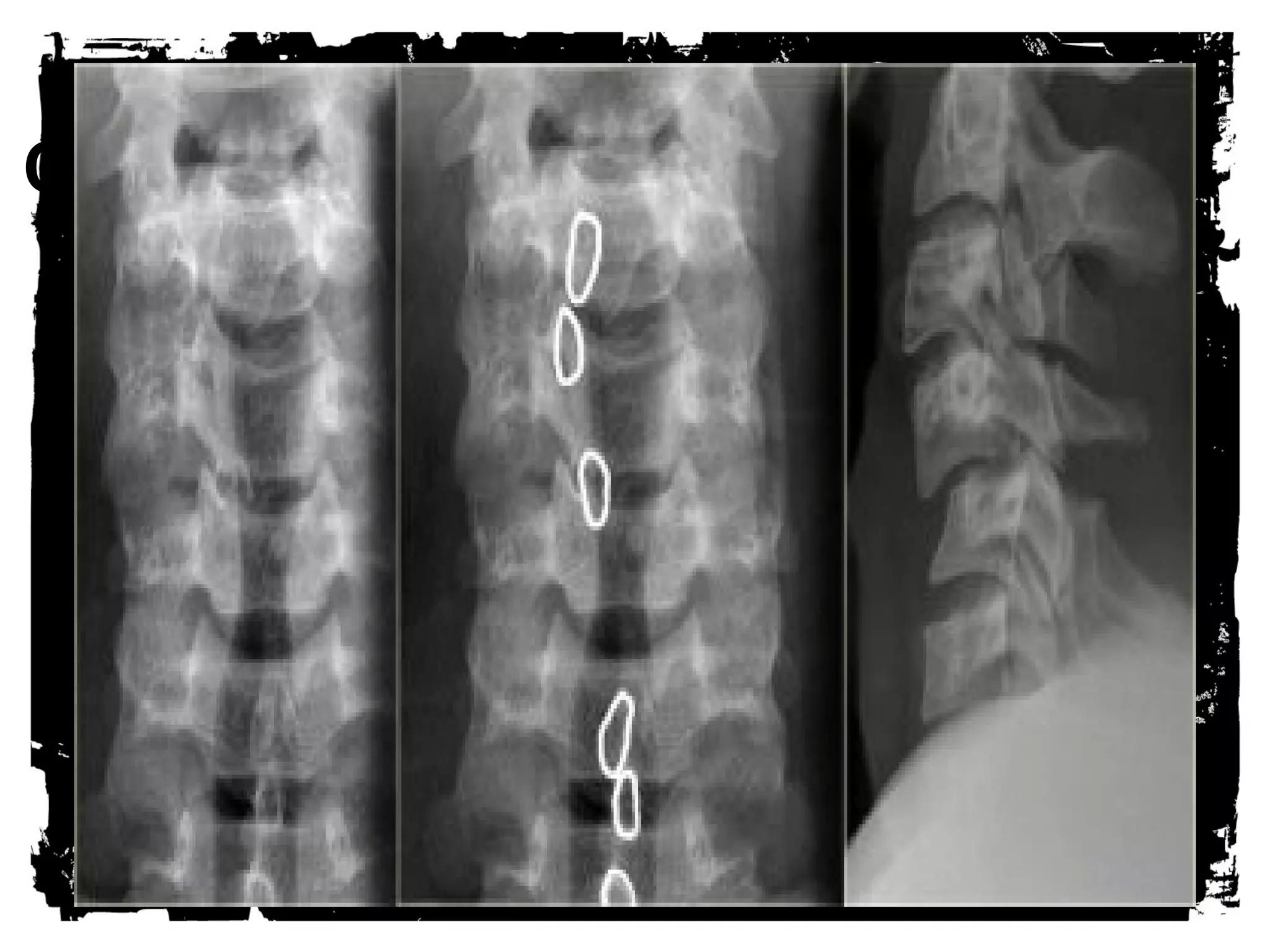
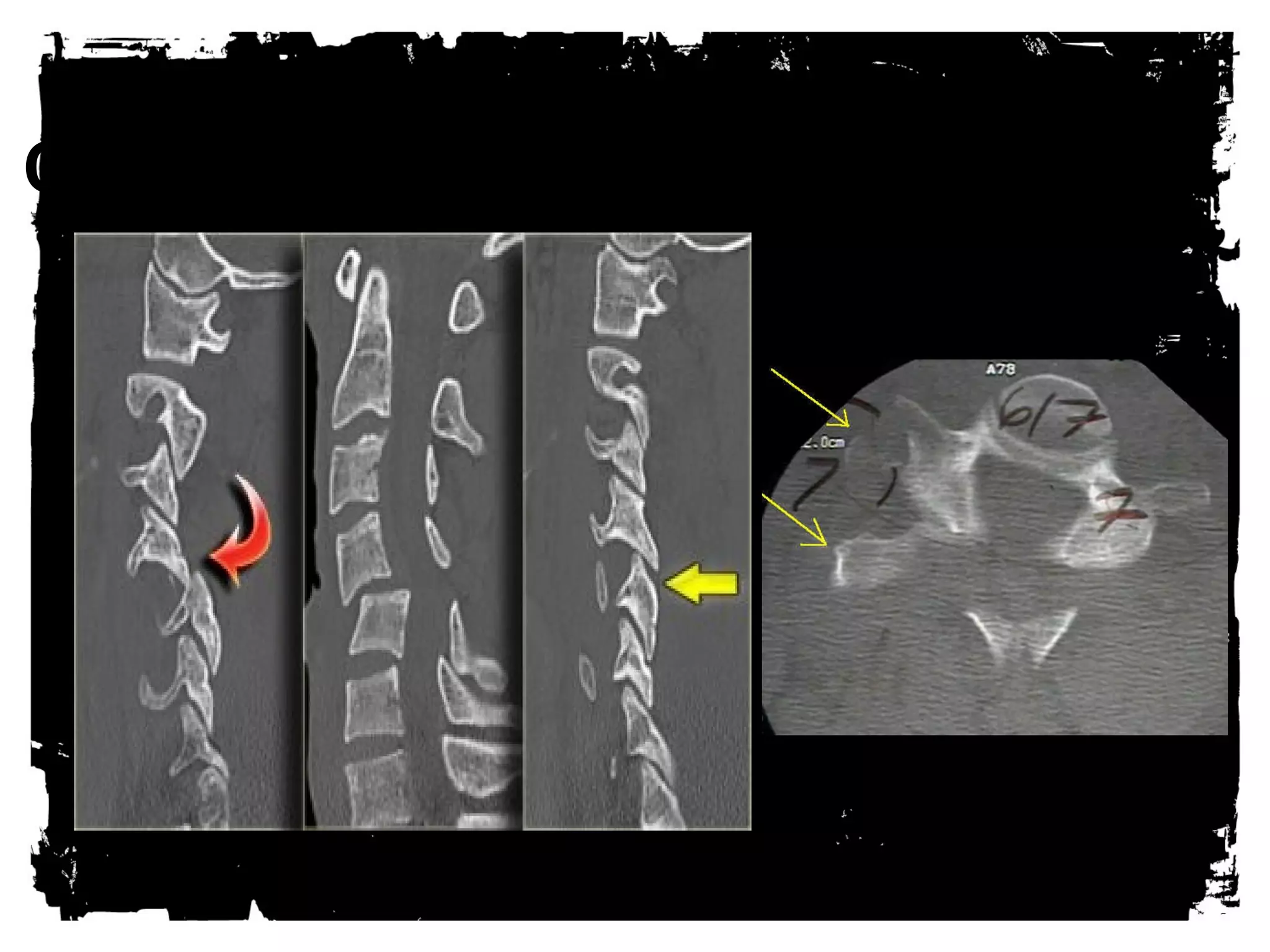
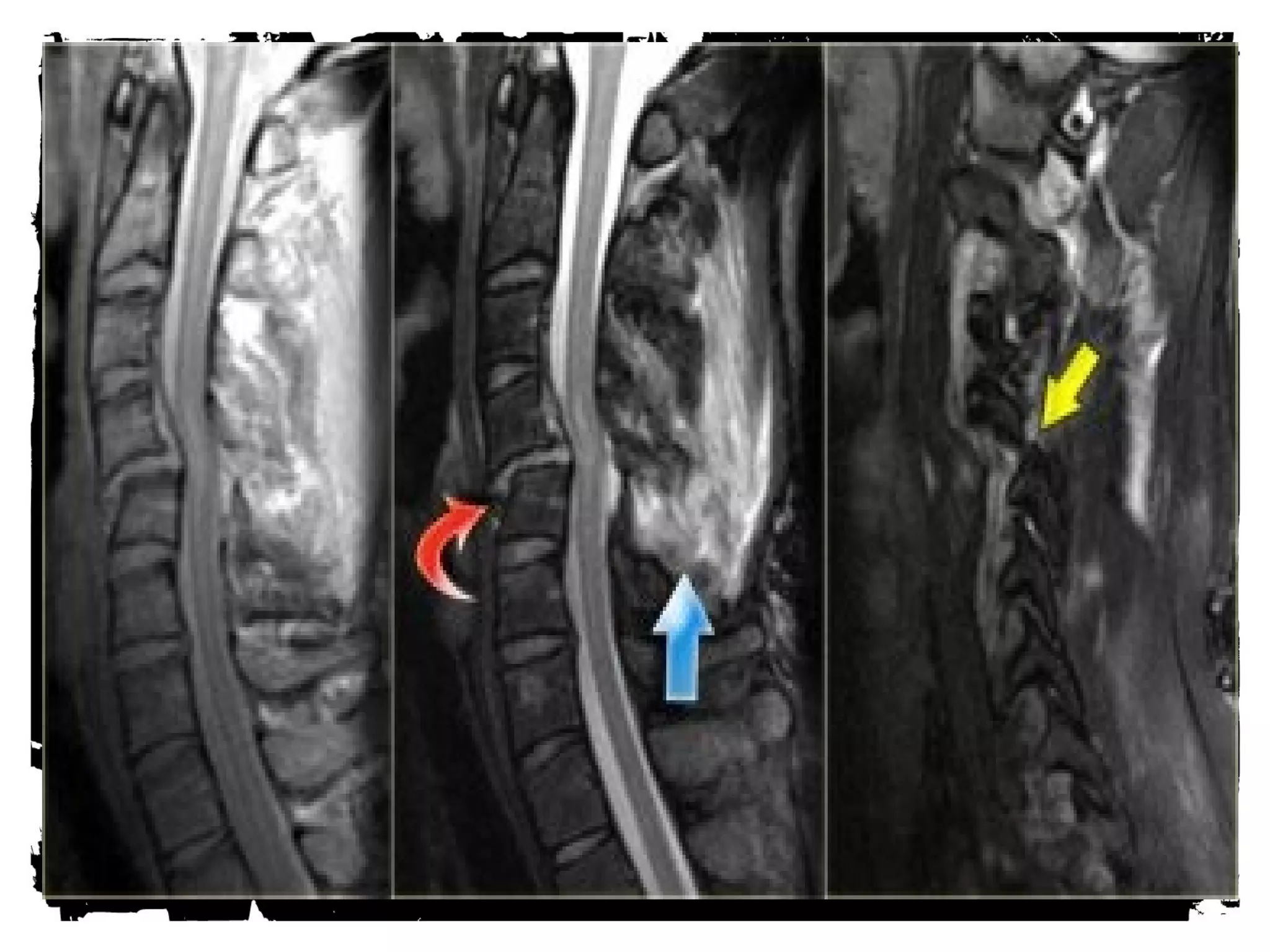
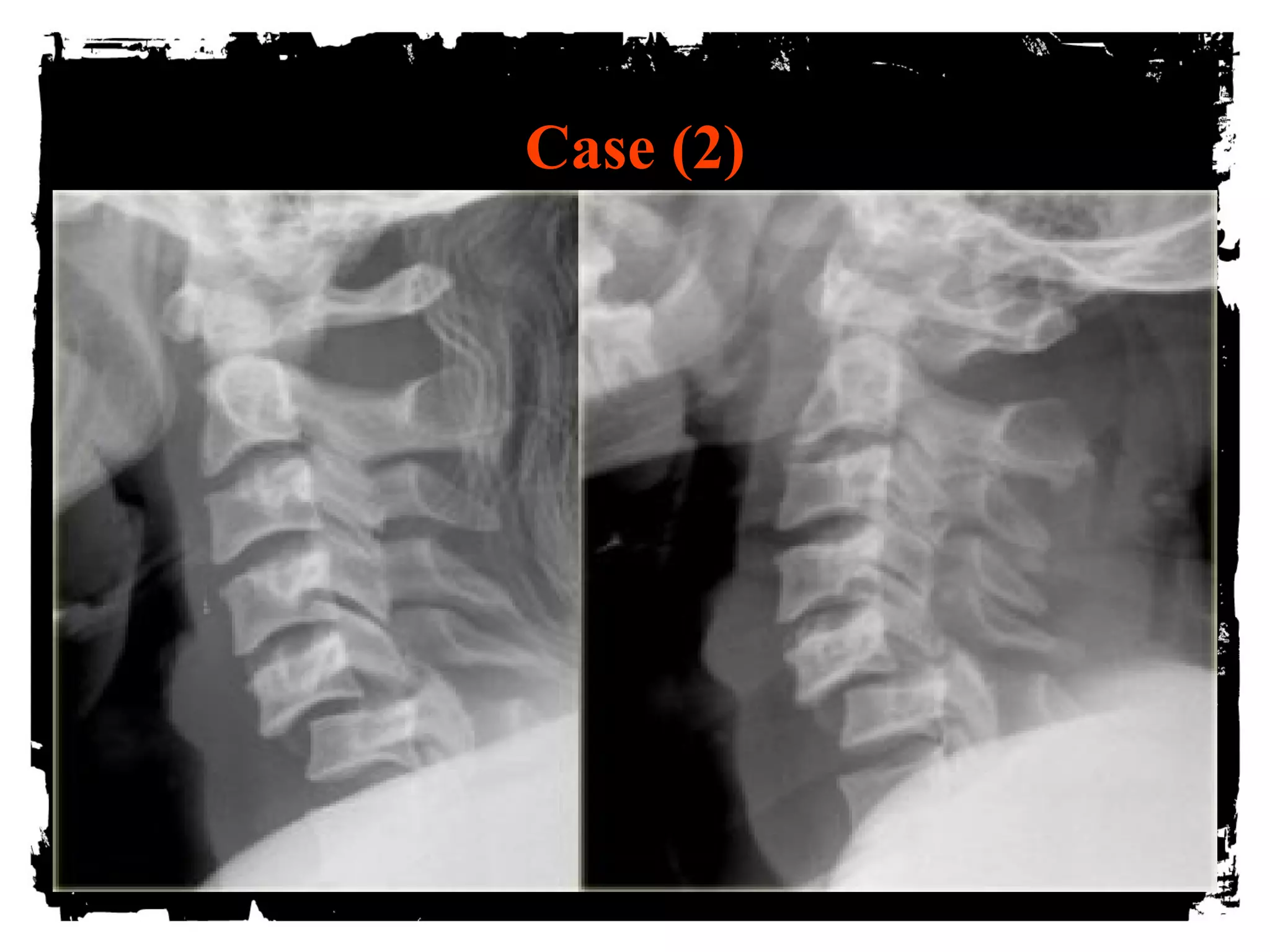
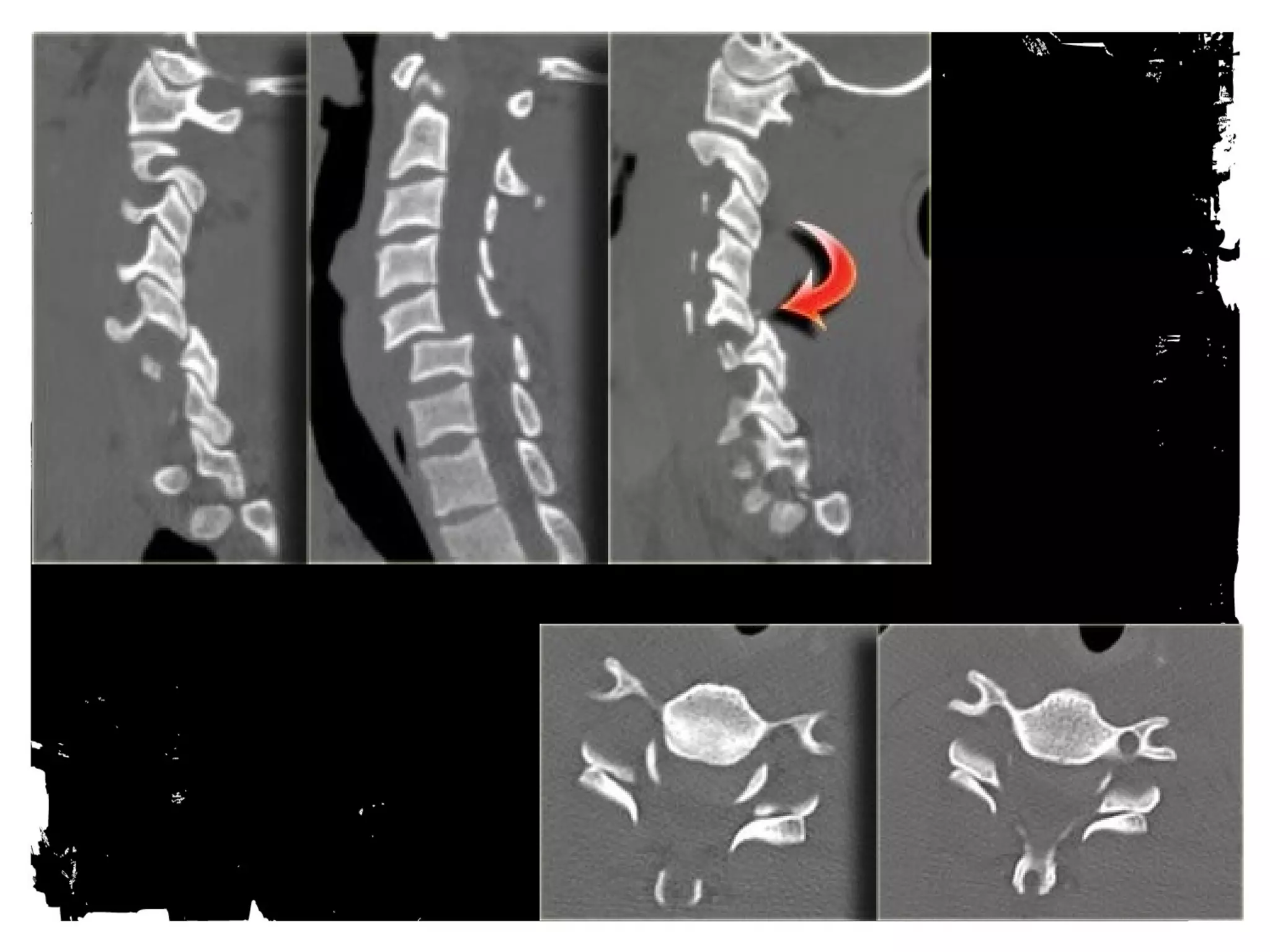
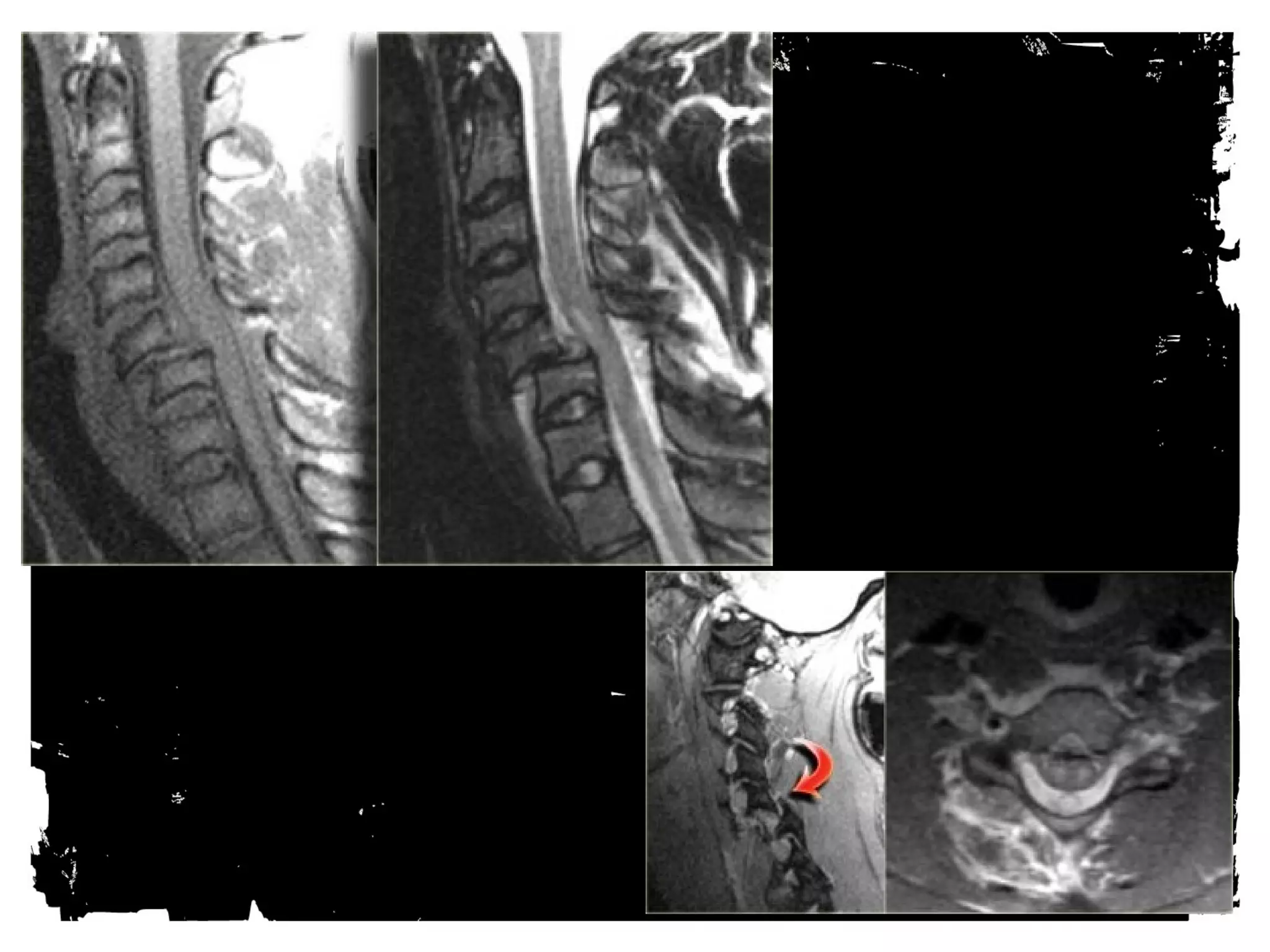
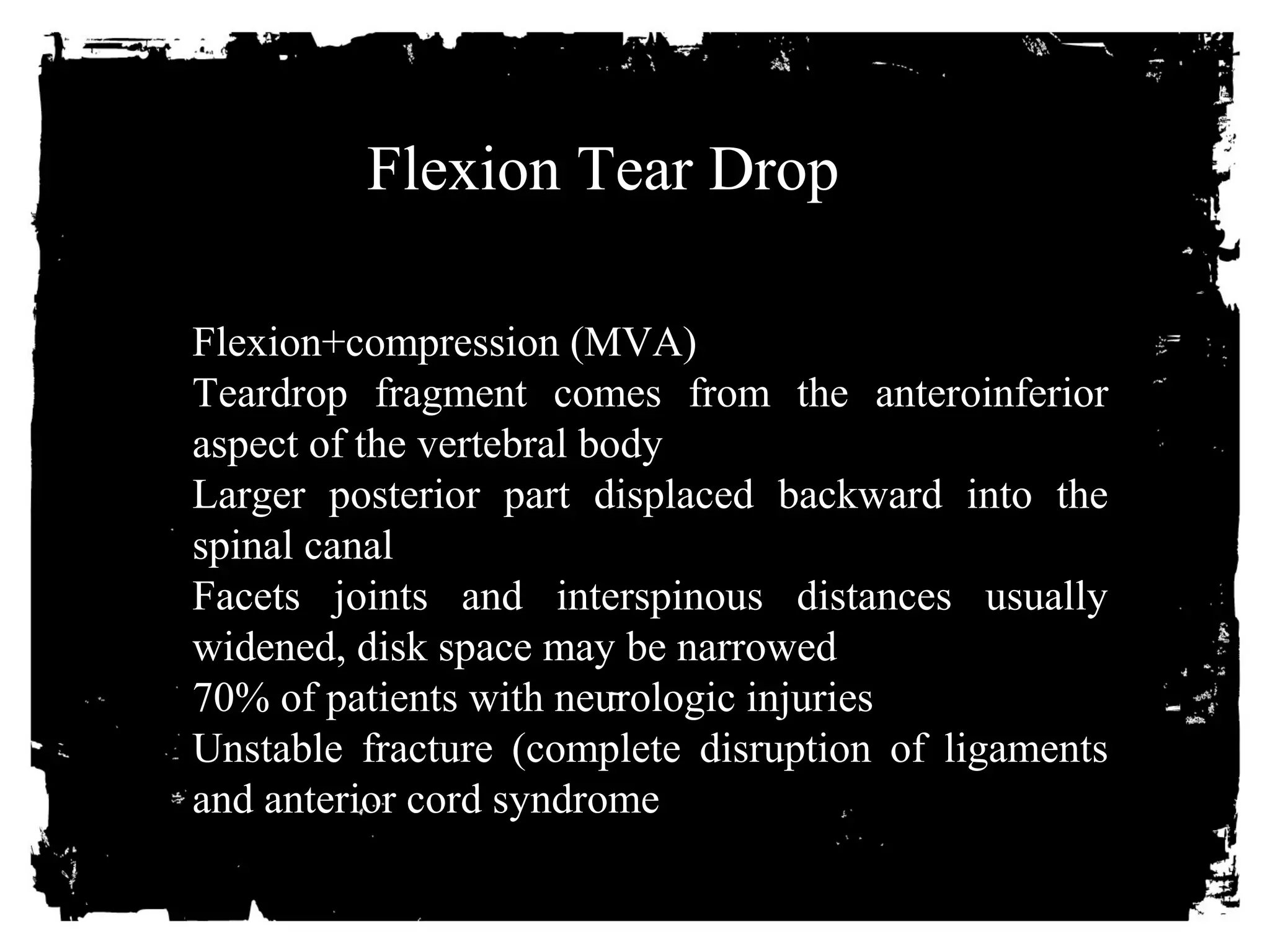
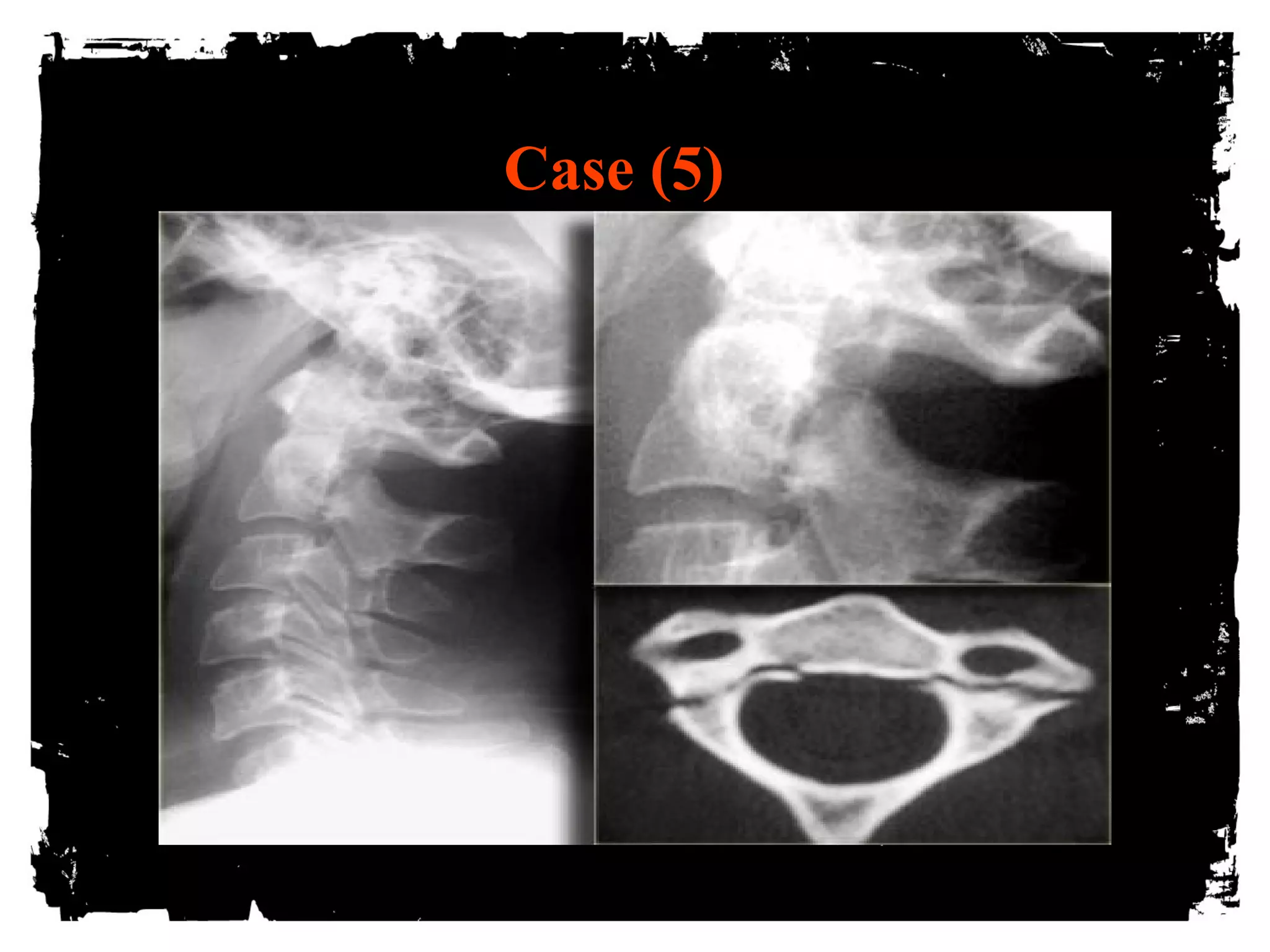
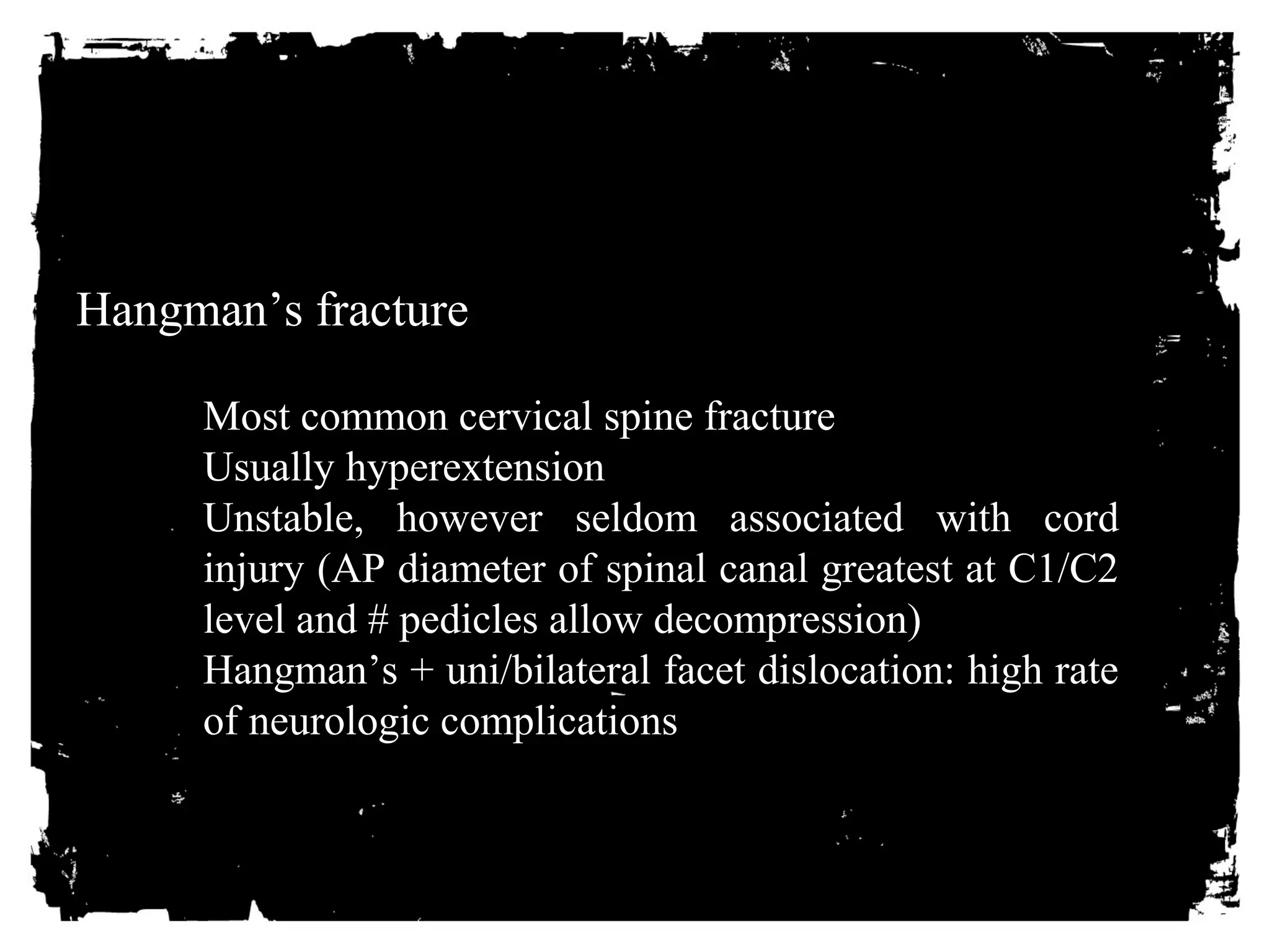
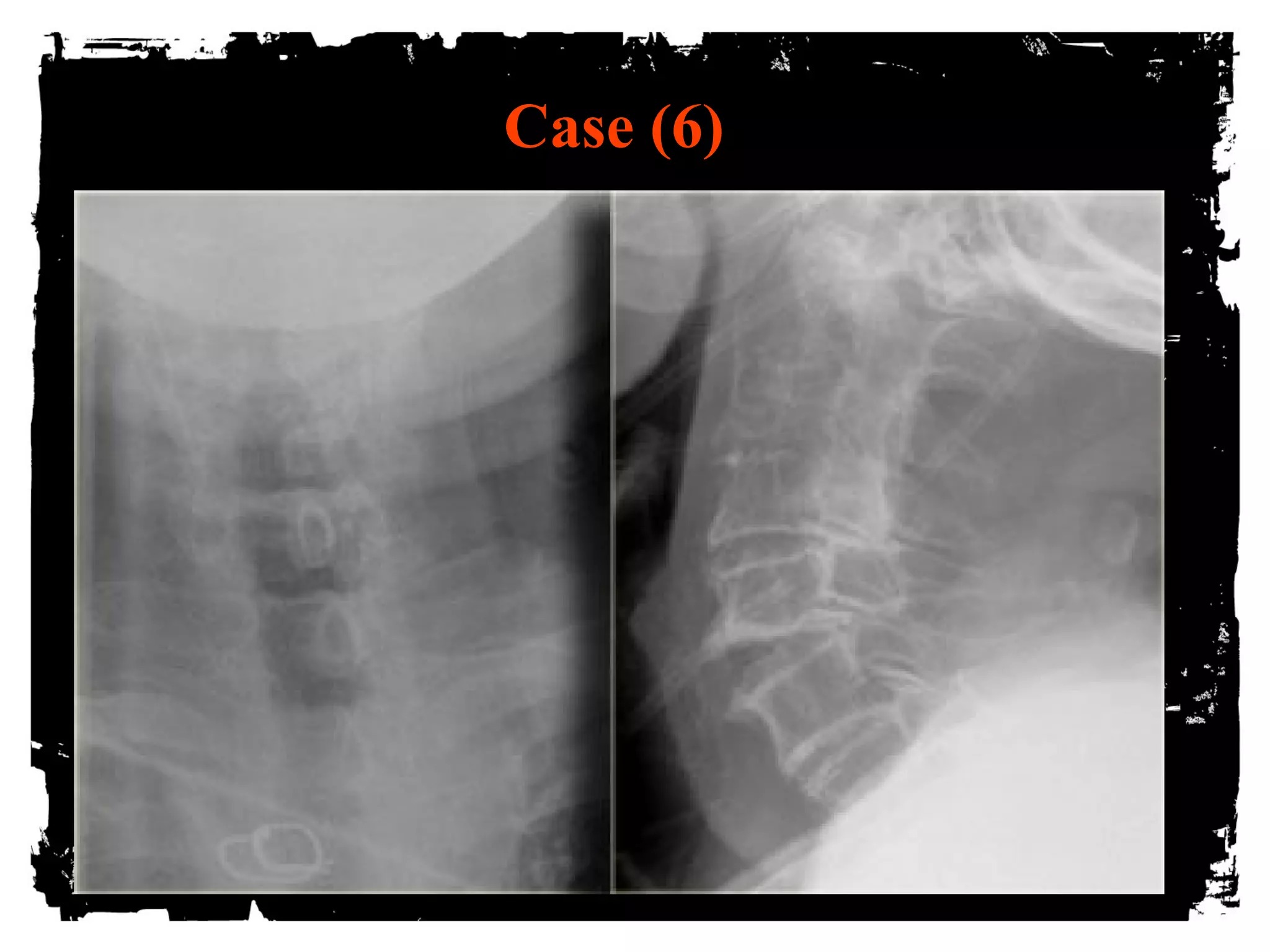
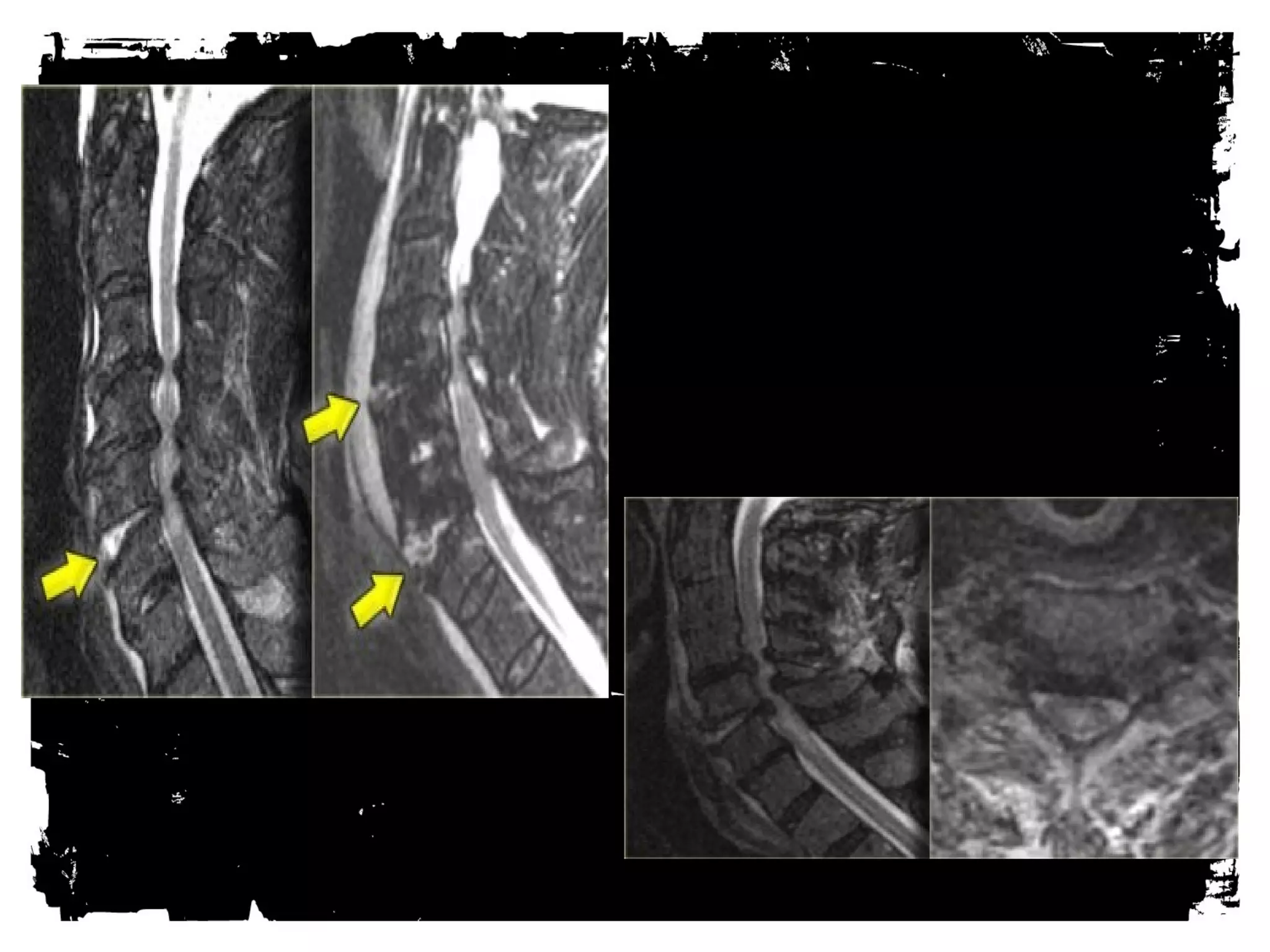
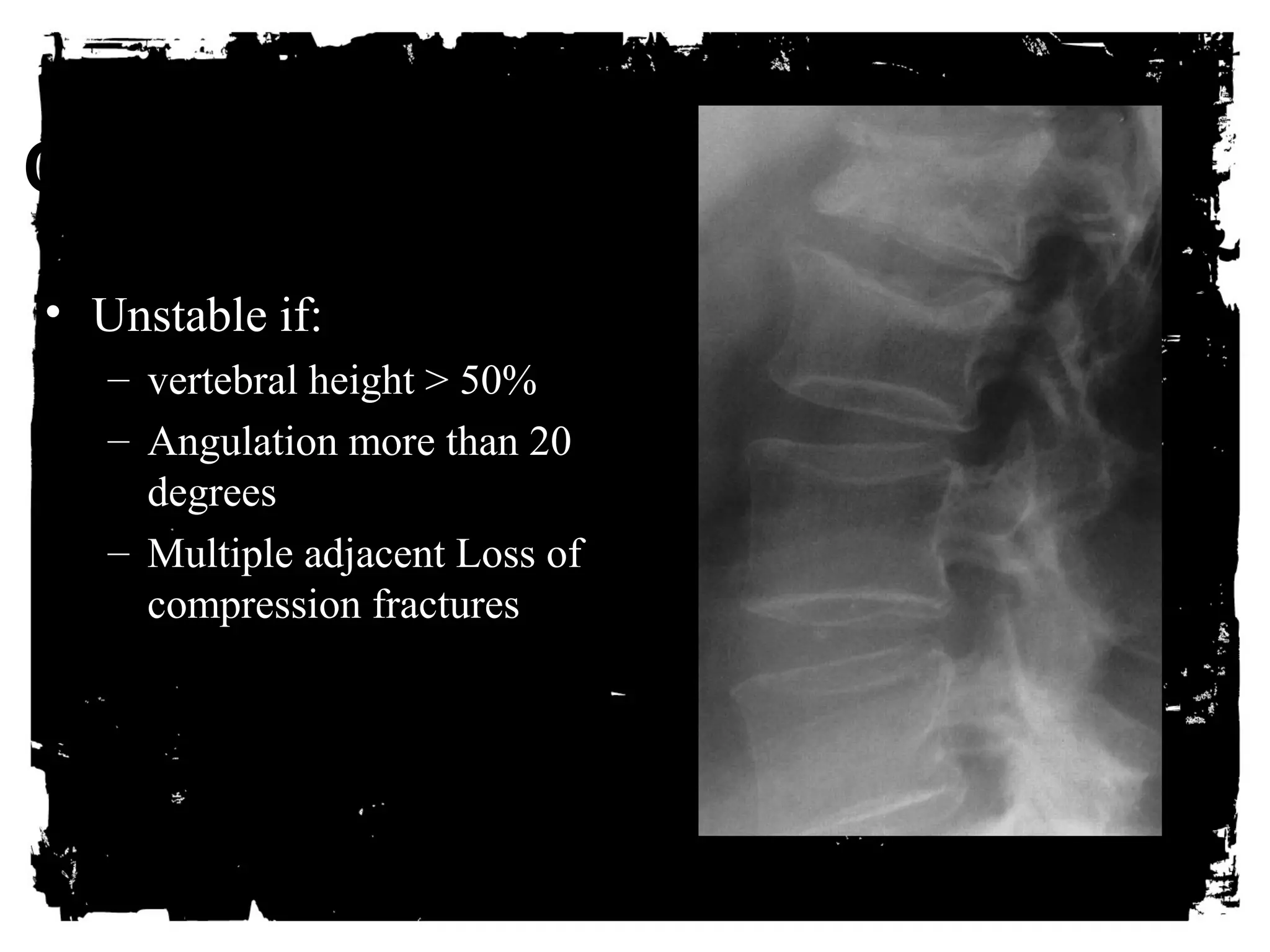
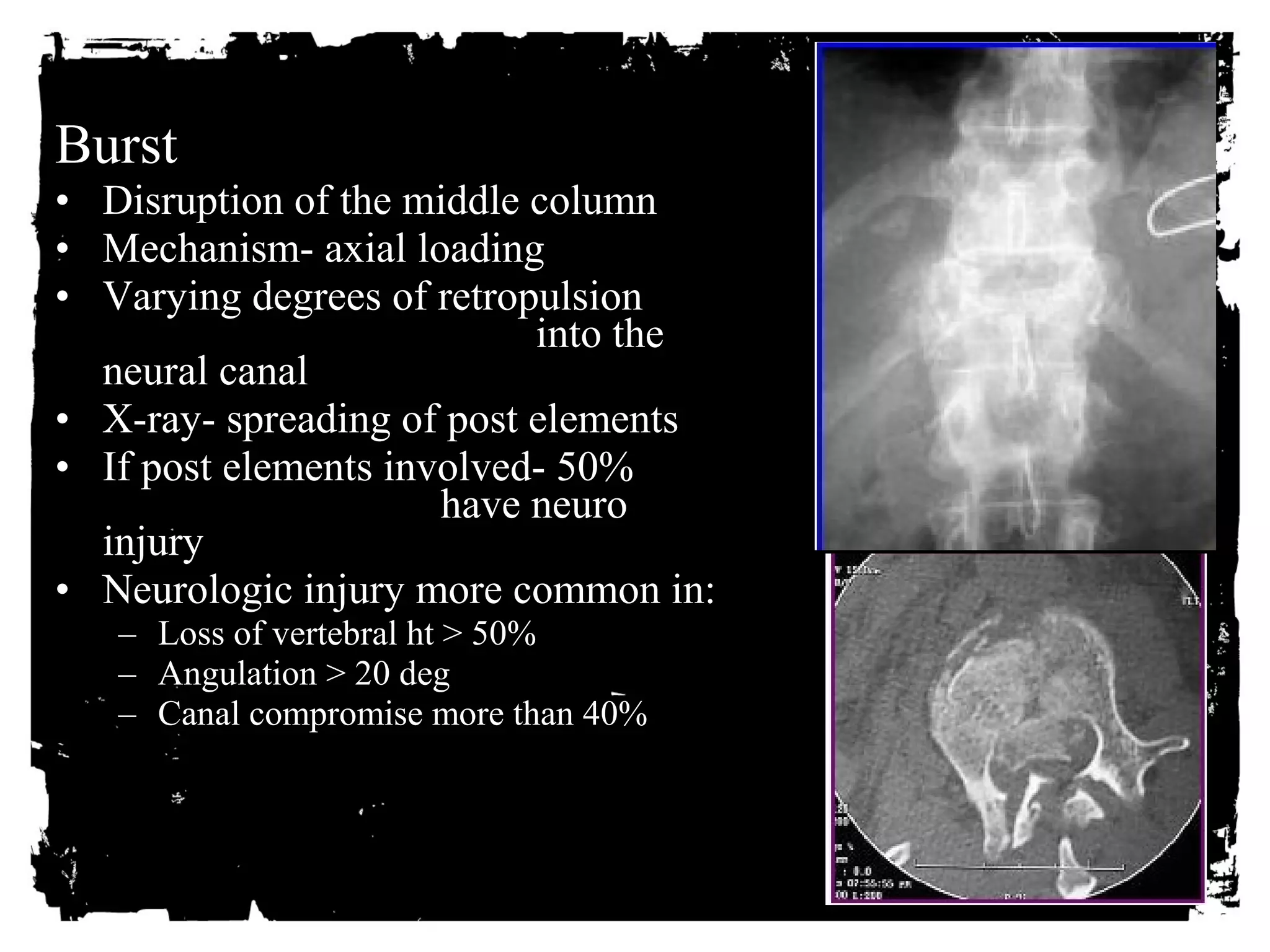
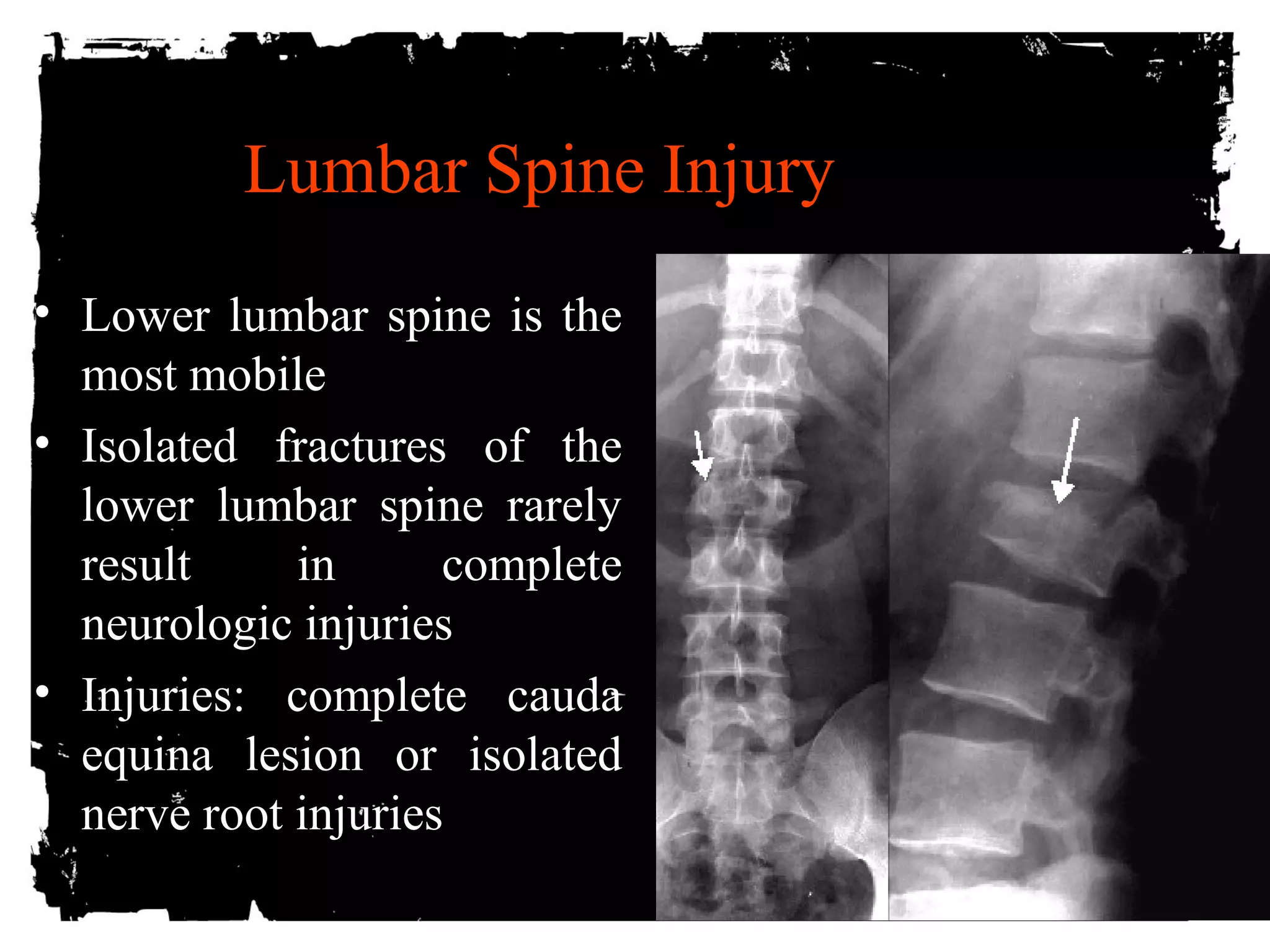
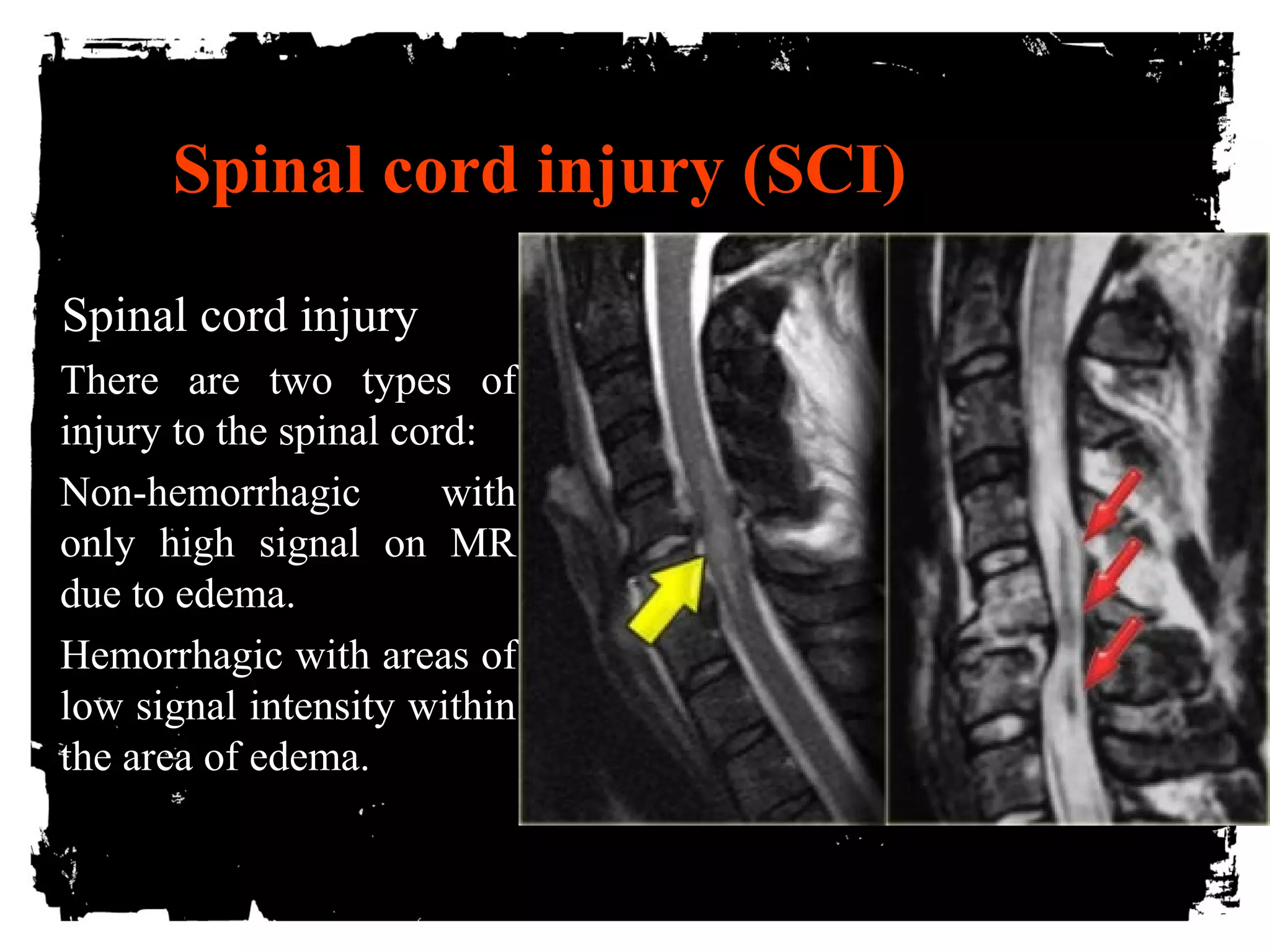
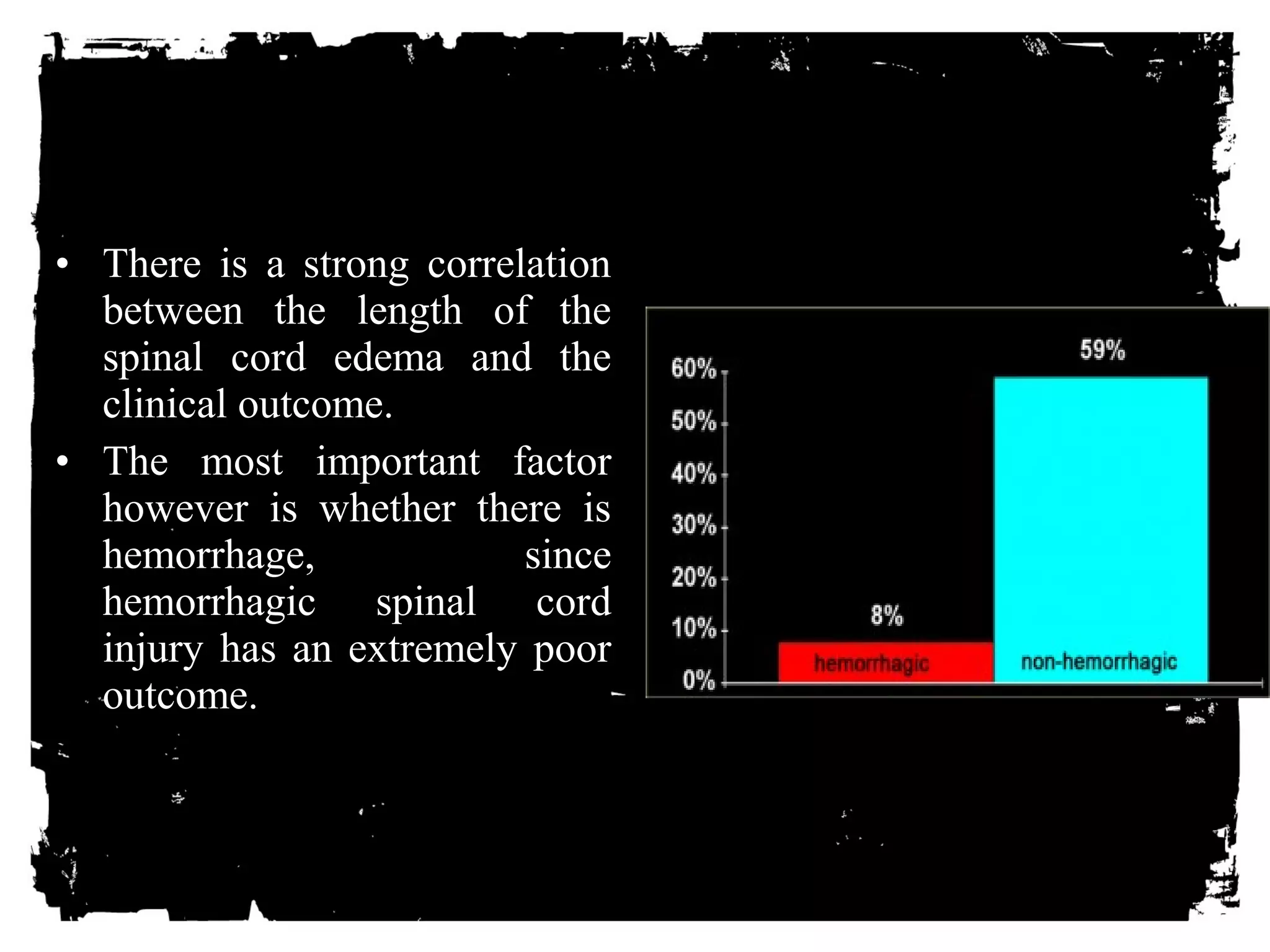
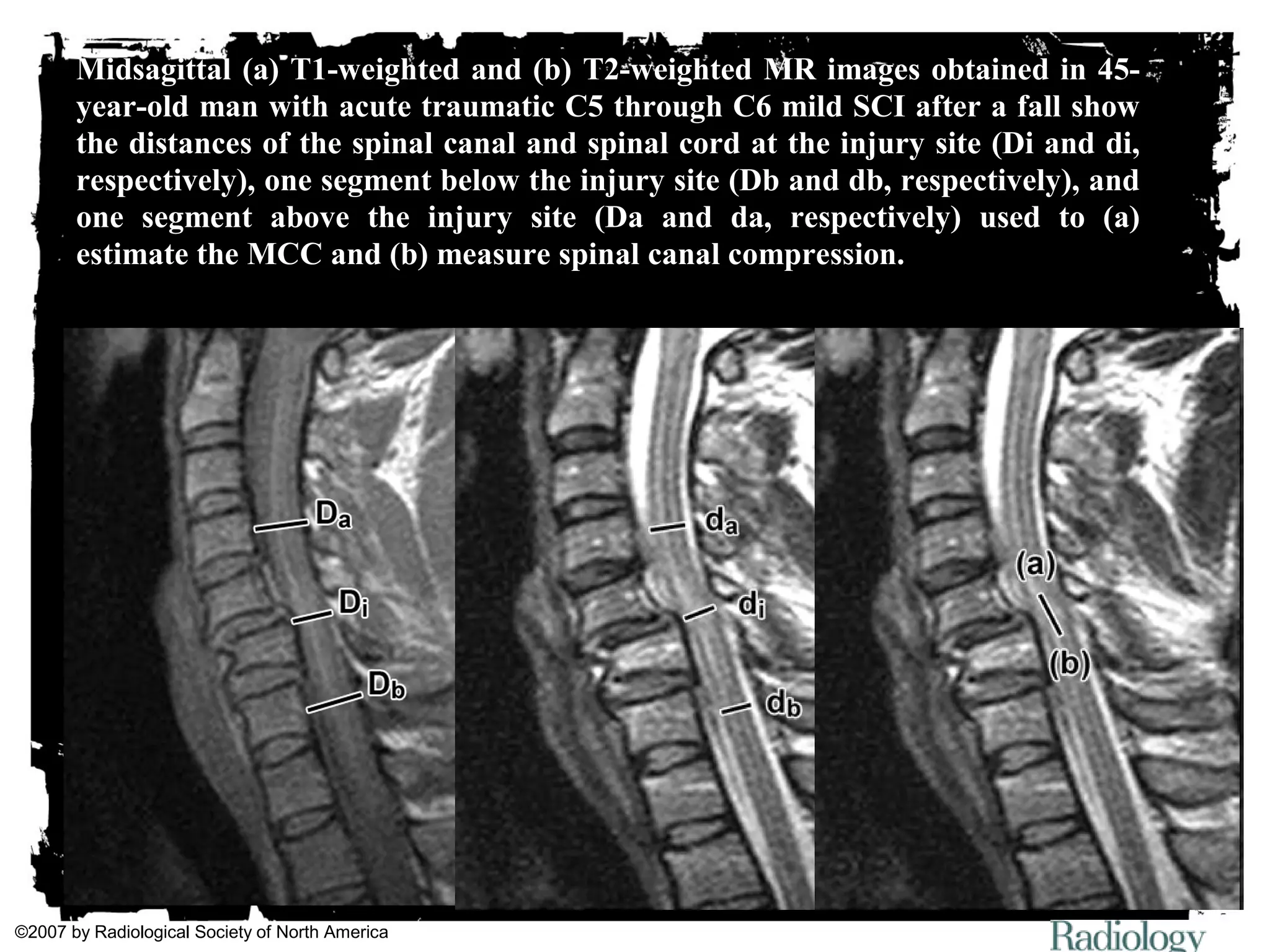
The document outlines trauma imaging guidelines and techniques presented at the Assiut University Trauma Course in March 2010, emphasizing the critical role of timely imaging in trauma care. It discusses specific modalities such as skull radiography and CT scans for diagnosing head and chest injuries, while advocating against routine skull X-rays in pediatric cases. Additionally, it covers the diagnostic approach to spinal injuries and the importance of utilizing various imaging modalities based on clinical indications.