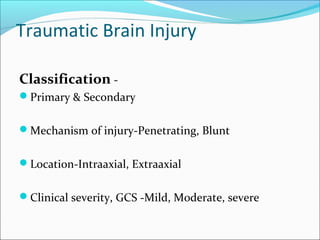
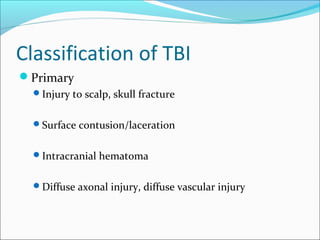
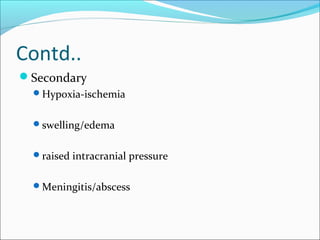
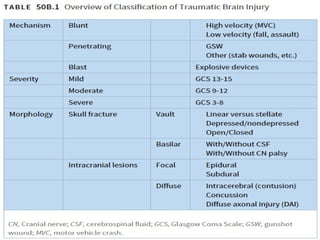
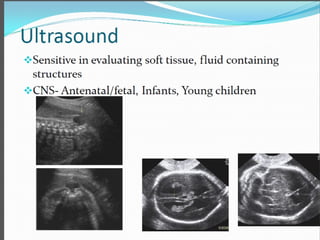
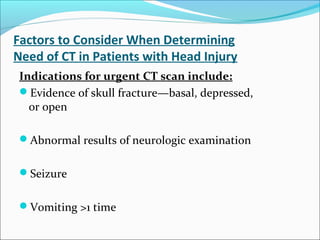
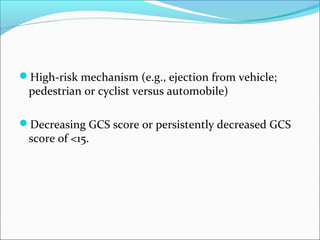
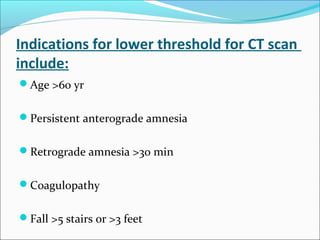
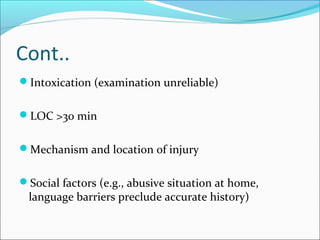
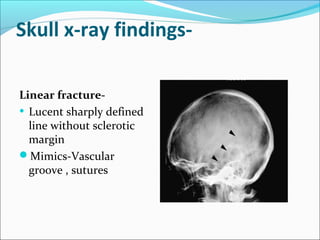
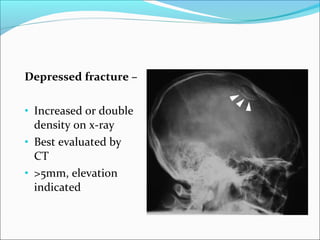
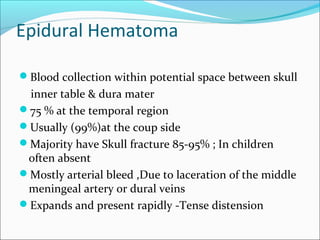
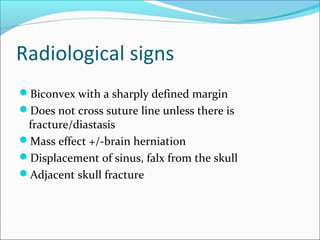
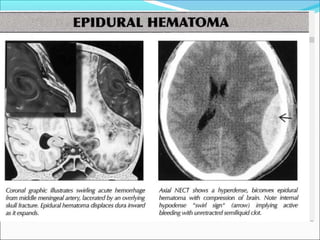
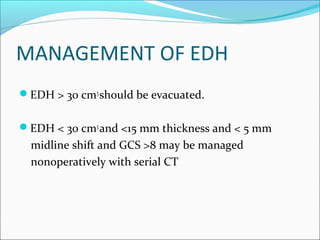
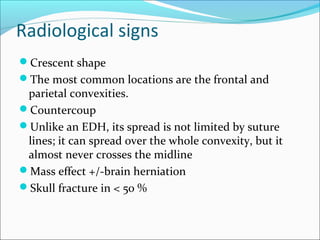
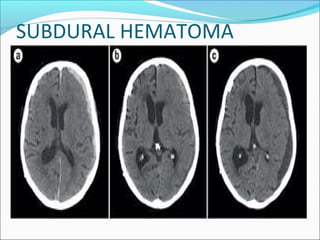
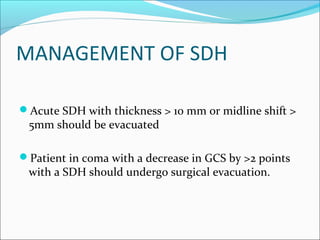
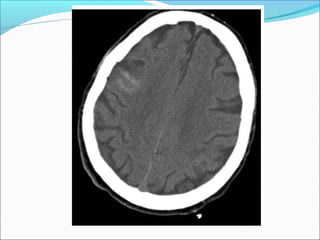
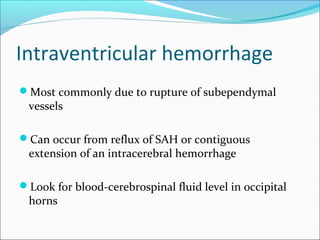
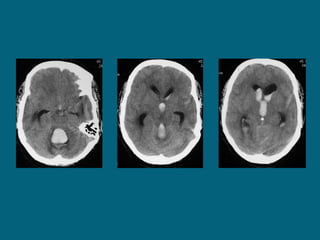
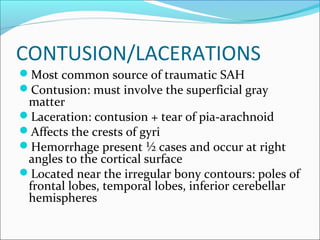
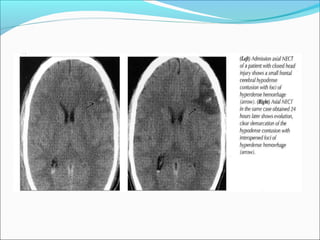
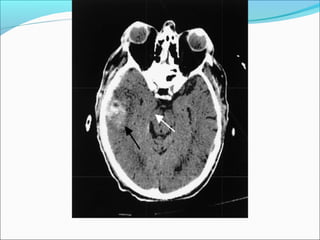
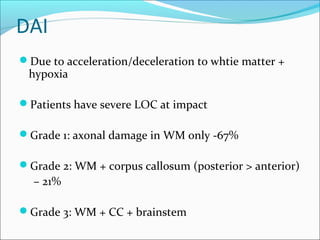
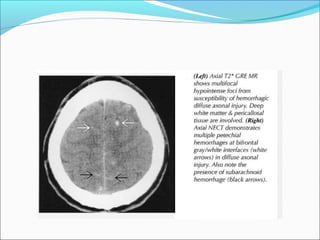
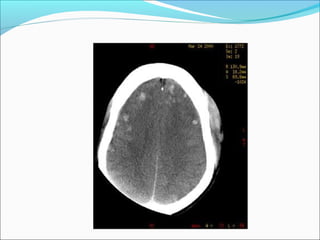
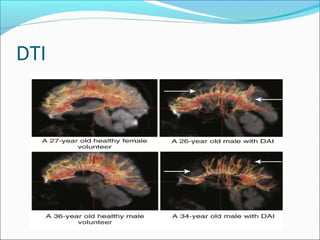
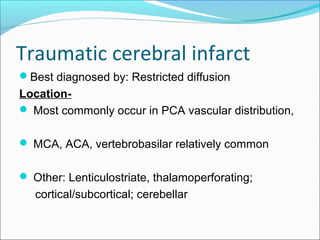
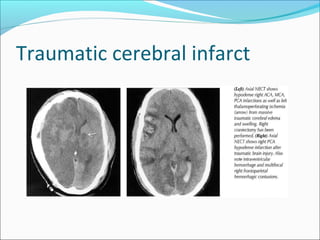
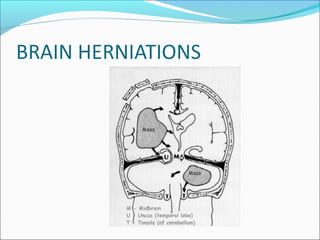
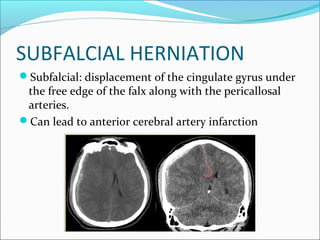
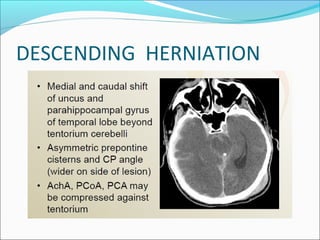
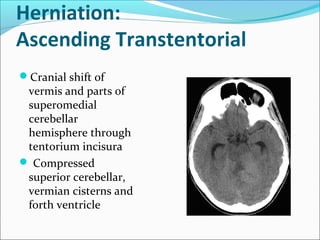
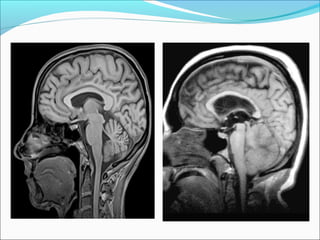
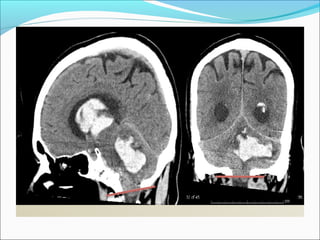
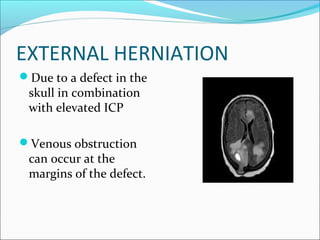
This document discusses traumatic brain injury and the use of various imaging modalities like CT and MRI to evaluate brain injuries. It begins by outlining the aims and providing background on head trauma. It then covers classifications of traumatic brain injury, clinical indications for imaging, and different imaging techniques. The bulk of the document describes various abnormalities that can be seen on imaging after brain trauma, including extraaxial hemorrhages, intraaxial injuries, and brain herniations. It provides details on indications for CT and MRI and emphasizes that CT is usually the first-line imaging modality for emergency brain evaluation.