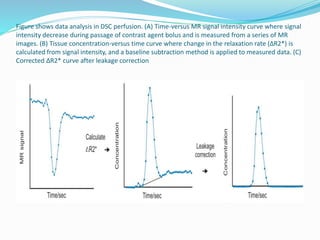
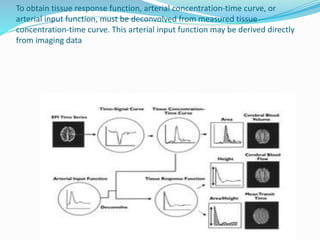
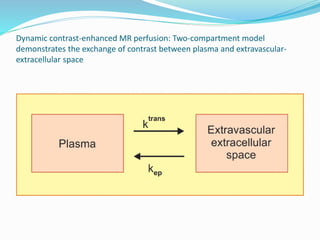
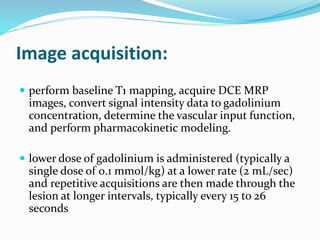
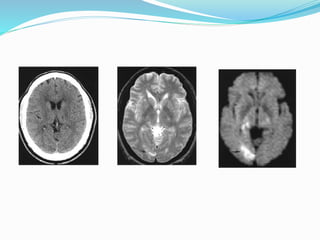
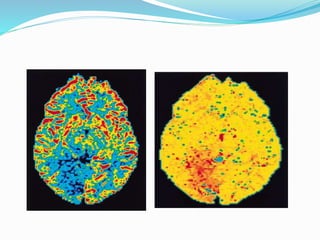
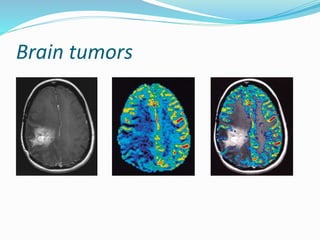
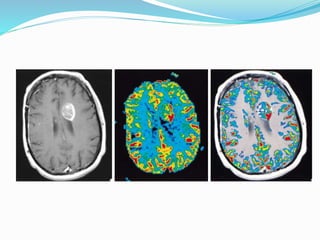
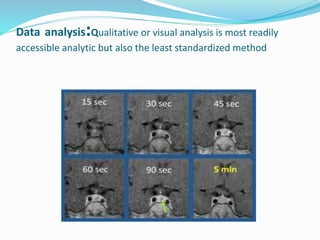
This document discusses dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) techniques for measuring tissue perfusion. It describes how DCE-MRI analyzes the passage of gadolinium contrast agents through tissue over time to provide quantitative measurements of microvascular properties like permeability and blood flow. The document outlines the principles, image acquisition, and qualitative, semi-quantitative, and quantitative analysis methods for DCE-MRI. It also discusses applications for evaluating brain tumors and other disorders.