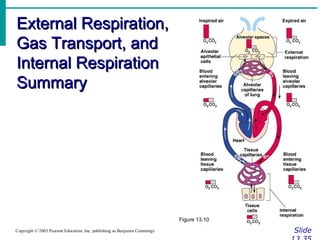
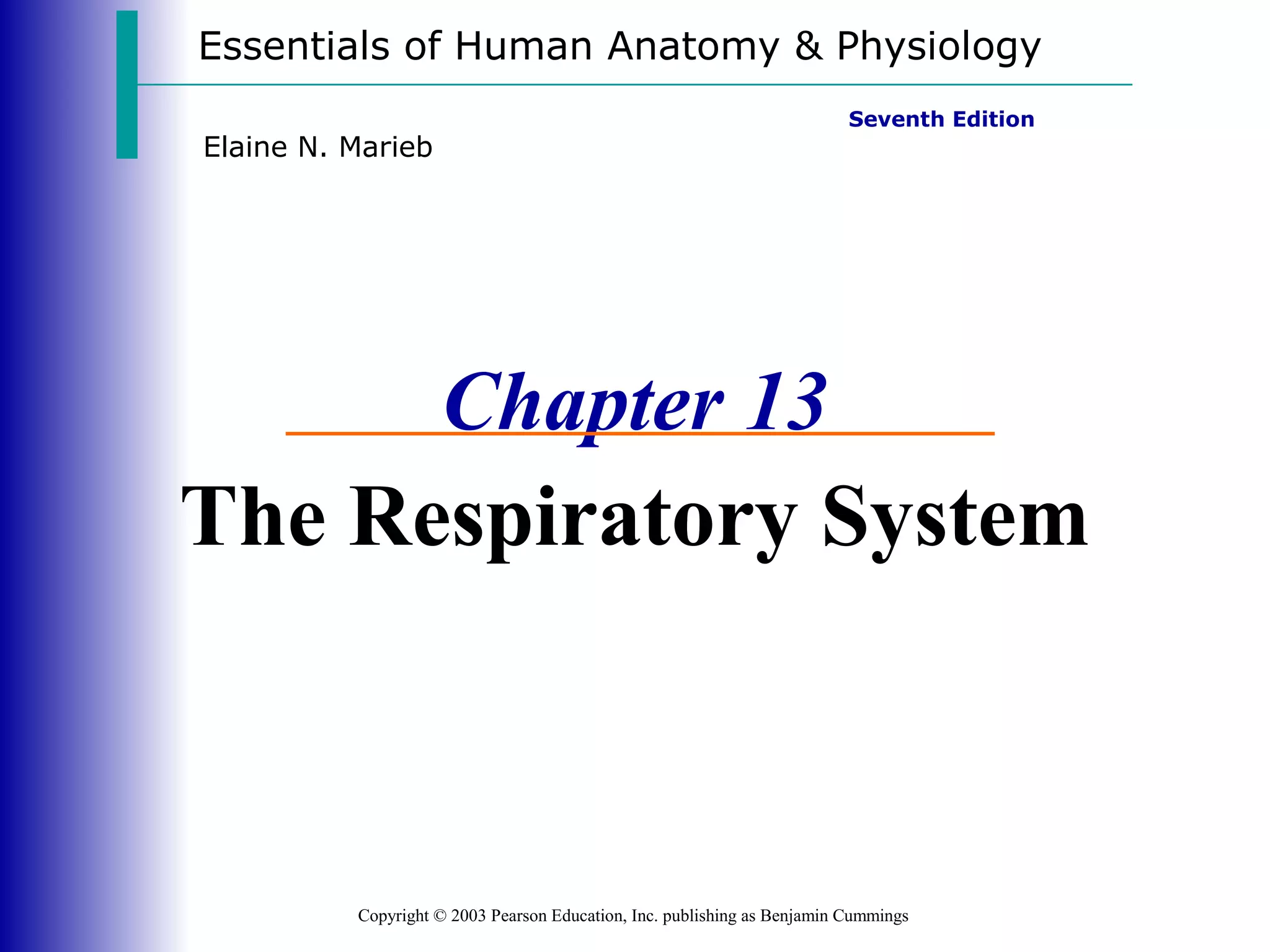
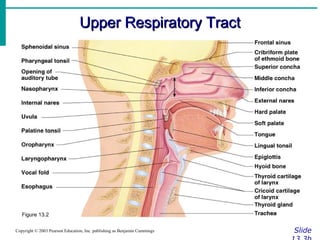
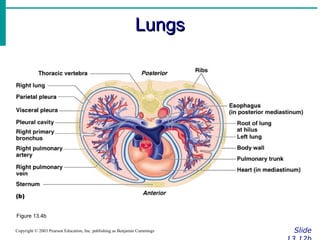
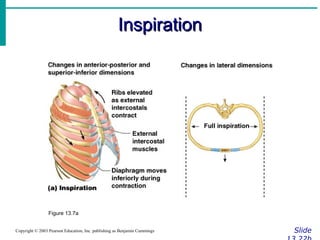
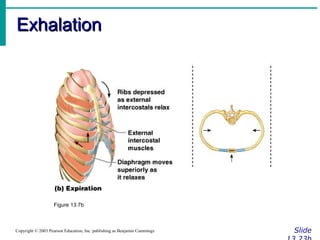
This document summarizes the key components and functions of the respiratory system. It describes the major organs involved, including the nose, pharynx, larynx, trachea, bronchi and lungs. It explains that gas exchange occurs in the alveoli of the lungs. It also outlines the mechanics of breathing, including inspiration and expiration. Pulmonary ventilation moves air in and out of the lungs, while external respiration is the gas exchange between the lungs and blood.
![Respiratory Volumes and CapacitiesRespiratory Volumes and Capacities
SlideCopyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings
• Normal breathing moves about 500 ml of air
with each breath (tidal volume [TV])
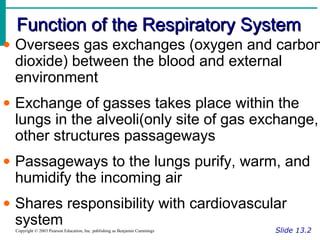
• Many factors that affect respiratory capacity
•A person’s size
•Sex
•Age
•Physical condition
• Residual volume of air – after exhalation,
about 1200 ml of air remains in the lungs](https://image.slidesharecdn.com/introductiontorespiratorysystem-170222021934/85/Introduction-to-respiratory-system-38-320.jpg)
![Gas Transport in the BloodGas Transport in the Blood
SlideCopyright © 2003 Pearson Education, Inc. publishing as Benjamin Cummings
• Oxygen transport in the blood
•Inside red blood cells attached to
hemoglobin (oxyhemoglobin [HbO2])
•A small amount is carried dissolved in the
plasma](https://image.slidesharecdn.com/introductiontorespiratorysystem-170222021934/85/Introduction-to-respiratory-system-47-320.jpg)