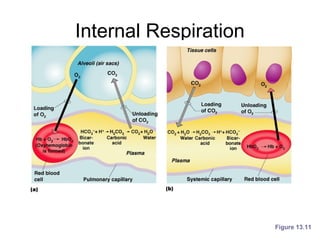
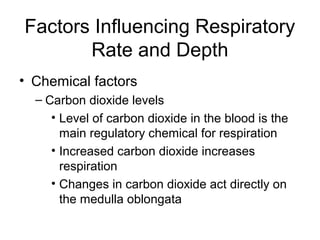
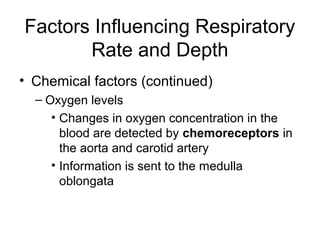
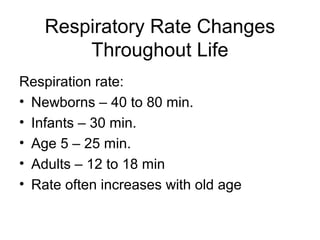
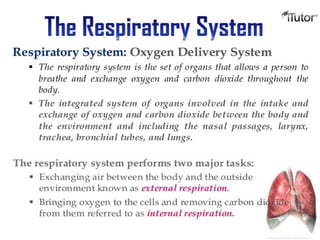
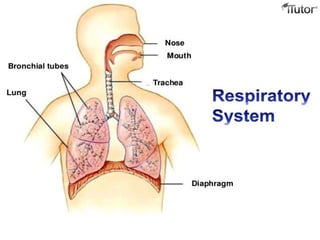
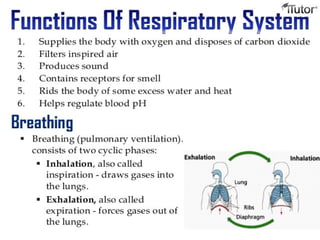
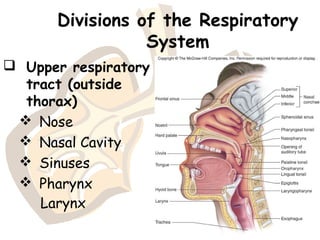
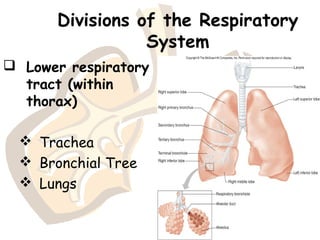
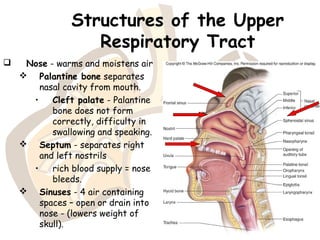
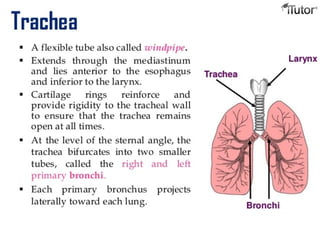
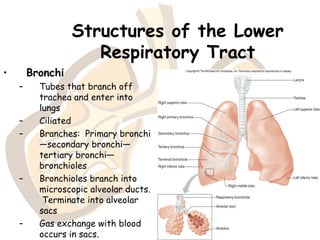
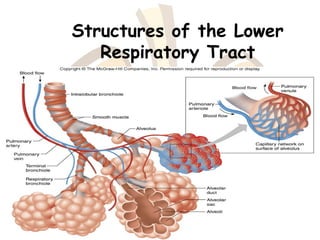
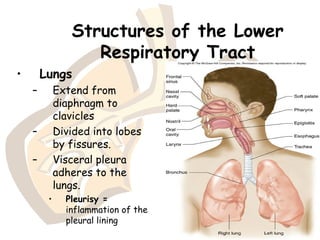
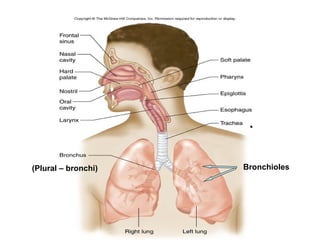
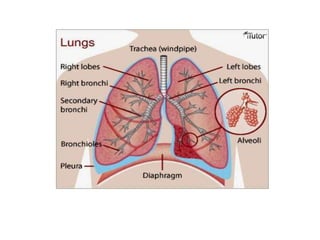
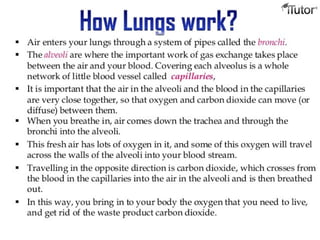
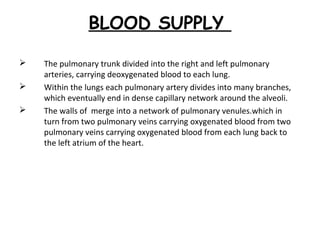
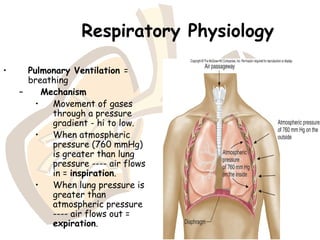
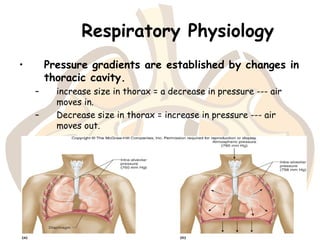
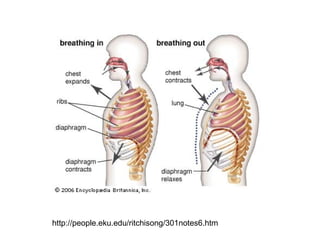
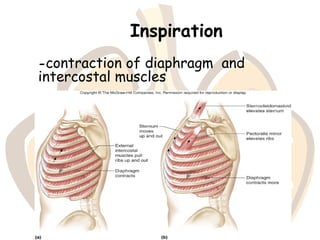
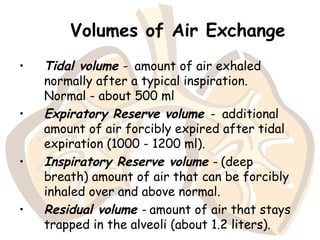
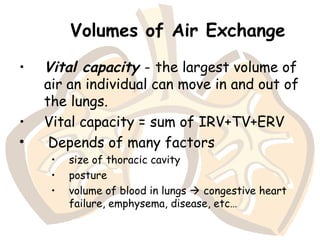
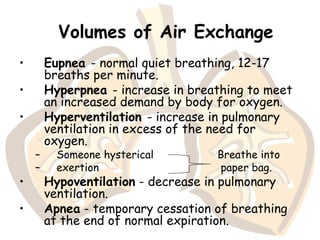
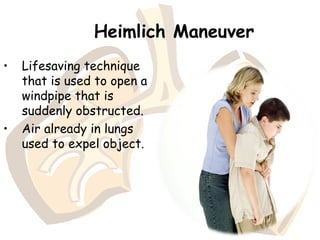
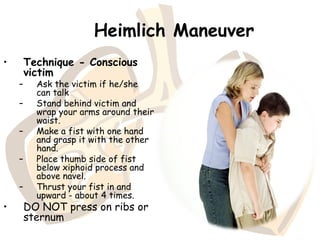
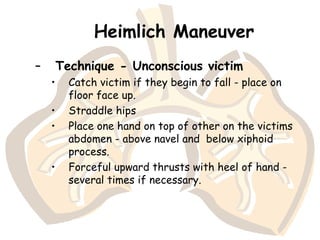
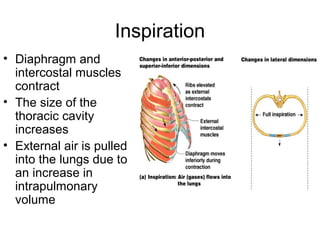
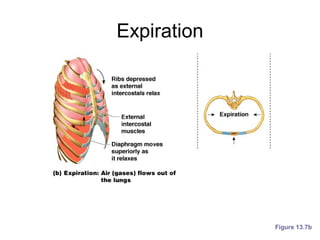
The document provides an overview of the respiratory system, detailing its divisions into the upper and lower respiratory tracts, and the various structures involved, including the nose, larynx, trachea, bronchi, and lungs. It explains the mechanics of breathing, gas exchange, and respiratory volumes, along with the physiological processes of respiration and factors influencing respiratory rates. Additionally, it covers emergency techniques like the Heimlich maneuver and highlights the role of neural and chemical factors in regulating respiration.
![Gas Transport in the Blood
• Oxygen transport in the blood
– Inside red blood cells attached to hemoglobin
(oxyhemoglobin [HbO2])
– A small amount is carried dissolved in the
plasma
• Carbon dioxide transport in the blood
– Most is transported in the plasma as
bicarbonate ion (HCO3–)
– A small amount is carried inside red blood
cells on hemoglobin, but at different binding
sites than those of oxygen](https://image.slidesharecdn.com/respiratorysystem161-180412143958/85/The-Respiratory-system-58-320.jpg)