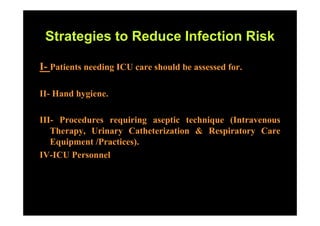
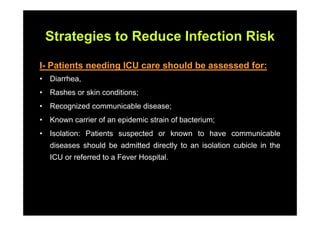
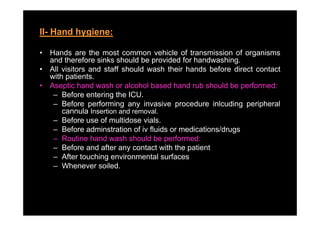
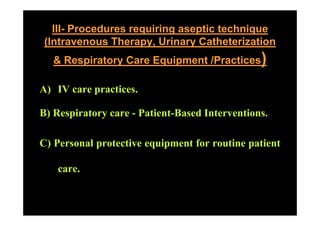
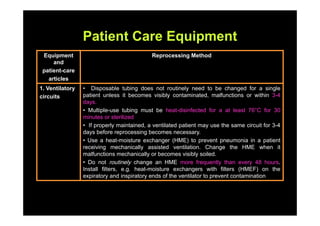
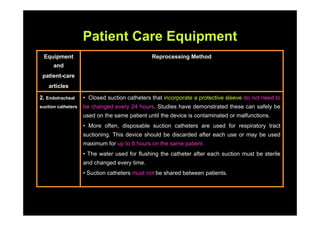
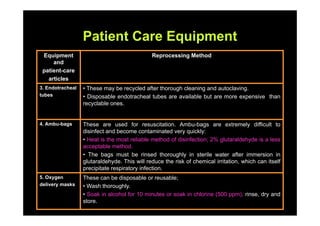
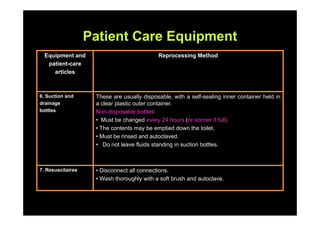
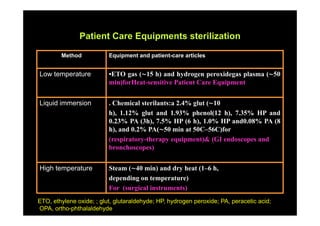
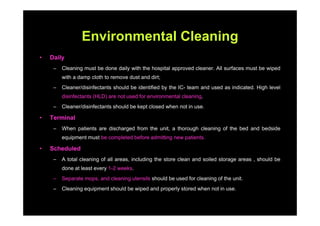
The document outlines infection control protocols for the intensive care unit, including strategies to reduce infection risks such as hand hygiene, aseptic techniques during procedures, and environmental cleaning. It discusses sources of cross-infection in the ICU and recommendations for patient care equipment reprocessing. The document also provides guidance on unit design, ventilation, traffic flow, and protocols for visitors and non-ICU staff.