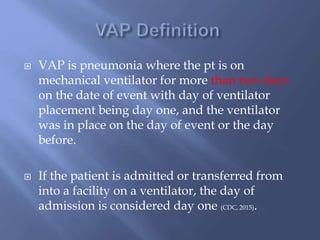
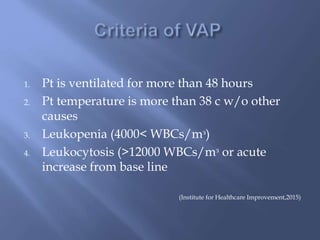
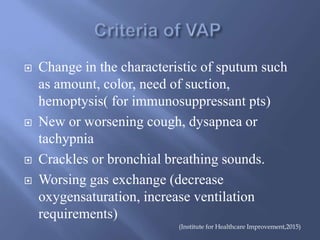
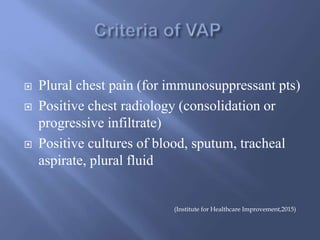
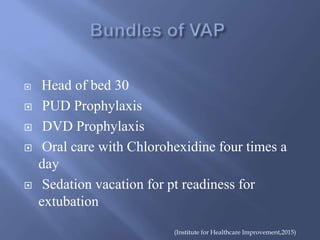
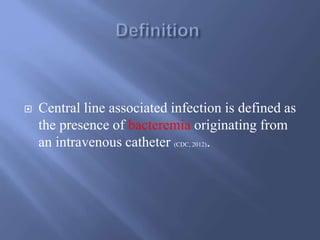
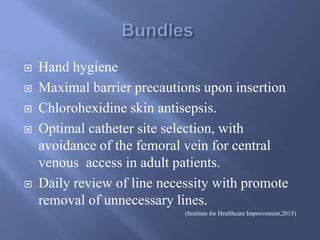
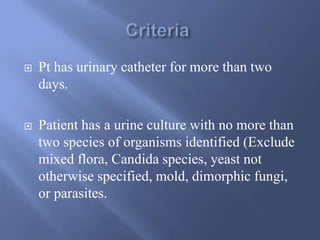
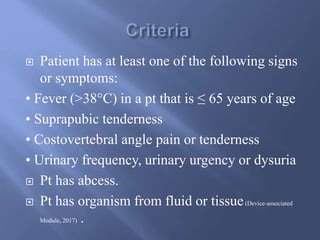
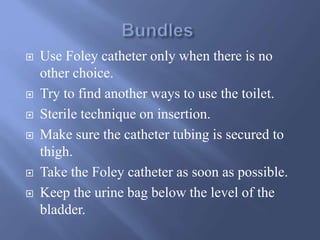
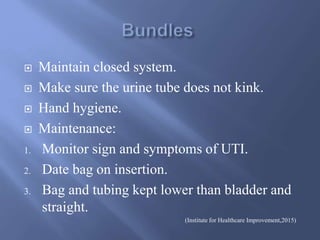
The document discusses strategies for reducing ventilator-associated pneumonia (VAP), catheter-associated urinary tract infections (CAUTI), and central line-associated infections (CLABSI) in intensive care units through proper education and guidelines. It details the definitions and assessment criteria for these infections, as well as interventions to improve patient safety and care quality. Key recommendations include adherence to safety bundles, proper hygiene practices, and regular evaluation of catheter necessity.



![ Blackwood, B., Alderdice, F., Burns, K. E. A., Cardwell, C. R., Lavery, G. G., &
O'Halloran, P. (2009). Protocolized vs. non-protocolized weaning for reducing the duration
of mechanical ventilation in critically ill adult patients: Cochrane review protocol. Journal
Of Advanced Nursing, 65(5), 957-964.
Centers for Disease Control and Prevention. Guidelines for preventing health-care-
associated pneumonia, 2015: recommendations of CDC and the Healthcare
Infection Control Practices Advisory Committee.
Central for Disease Control and Prevention. Device-associated Module (2017). Urinary
Tract Infection (Catheter-Associated Urinary Tract Infection [CAUTI] and Non-Catheter-
Associated Urinary Tract Infection [UTI]) and Other Urinary System Infection [USI])
Events.](https://image.slidesharecdn.com/icubundles-190306105255/85/ICU-Bundles-24-320.jpg)