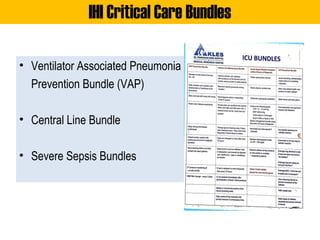
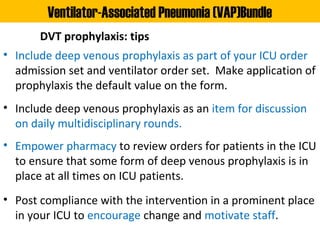
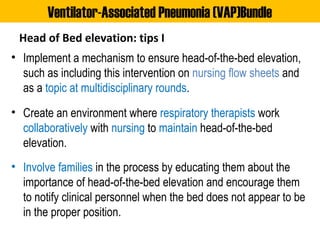
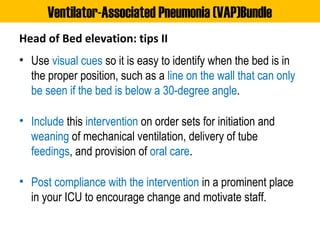
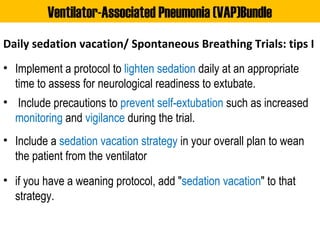
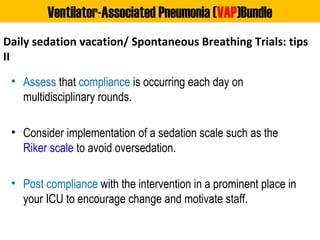
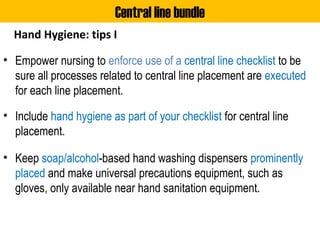
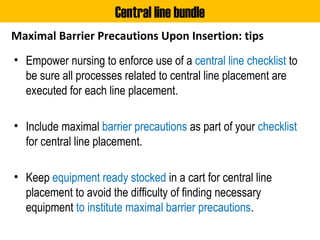
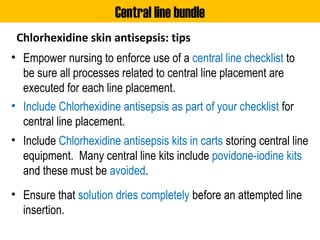
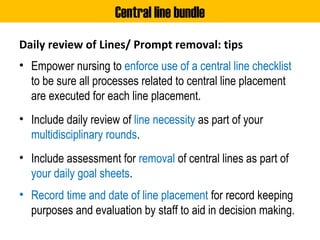
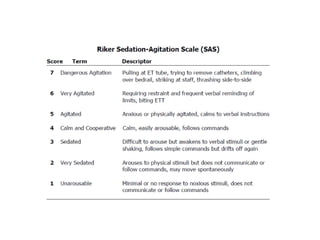
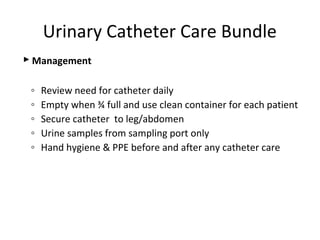
The document outlines evidence-based care bundles in intensive care units (ICUs) to improve patient outcomes, including the Ventilator Associated Pneumonia (VAP) bundle, central line bundle, and severe sepsis bundles. Each bundle consists of specific best practices such as daily sedation vacations, hand hygiene, and timely administration of antibiotics, all aimed at preventing complications and promoting safety. The document emphasizes the importance of implementing these bundles as part of standard practice to enhance patient safety and care efficiency.