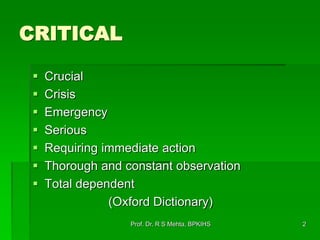
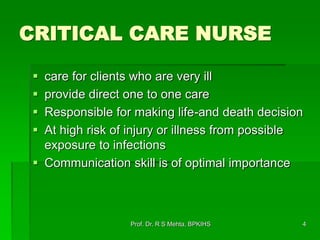
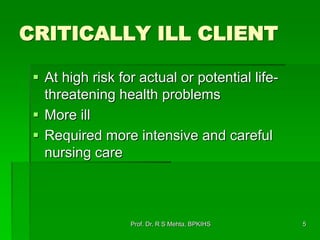
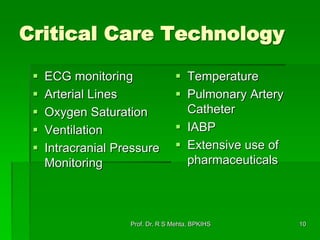
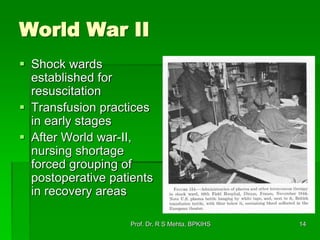
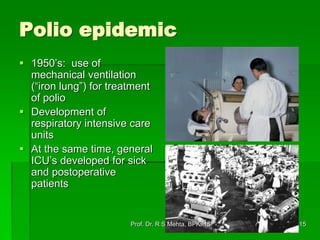
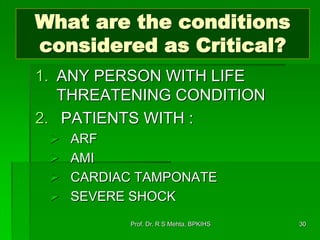
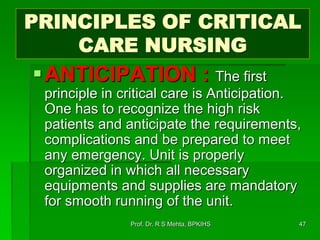
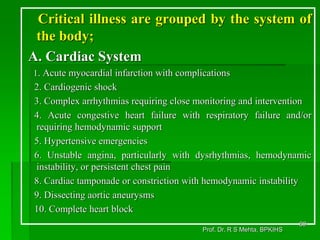
Critical care nursing involves caring for patients with life-threatening illnesses or injuries. It requires thorough observation, intensive nursing care, and management of complex equipment and medications. Critical care nurses provide one-on-one care for critically ill patients in specialized units like intensive care units (ICUs). Their role is highly demanding but crucial for making important decisions that can mean life or death. Critical care has evolved over time with advances in technology and the development of ICUs to treat critically ill patients following World War II and the polio epidemic.











![“It may seem a
strange principle to
enunciate (articulate)
as the very first
requirement in a
Hospital that it should
do the sick no harm.”
[1859]
113Prof. Dr. R S Mehta, BPKIHS](https://image.slidesharecdn.com/1-151005052754-lva1-app6892/85/1-critical-care-113-320.jpg)