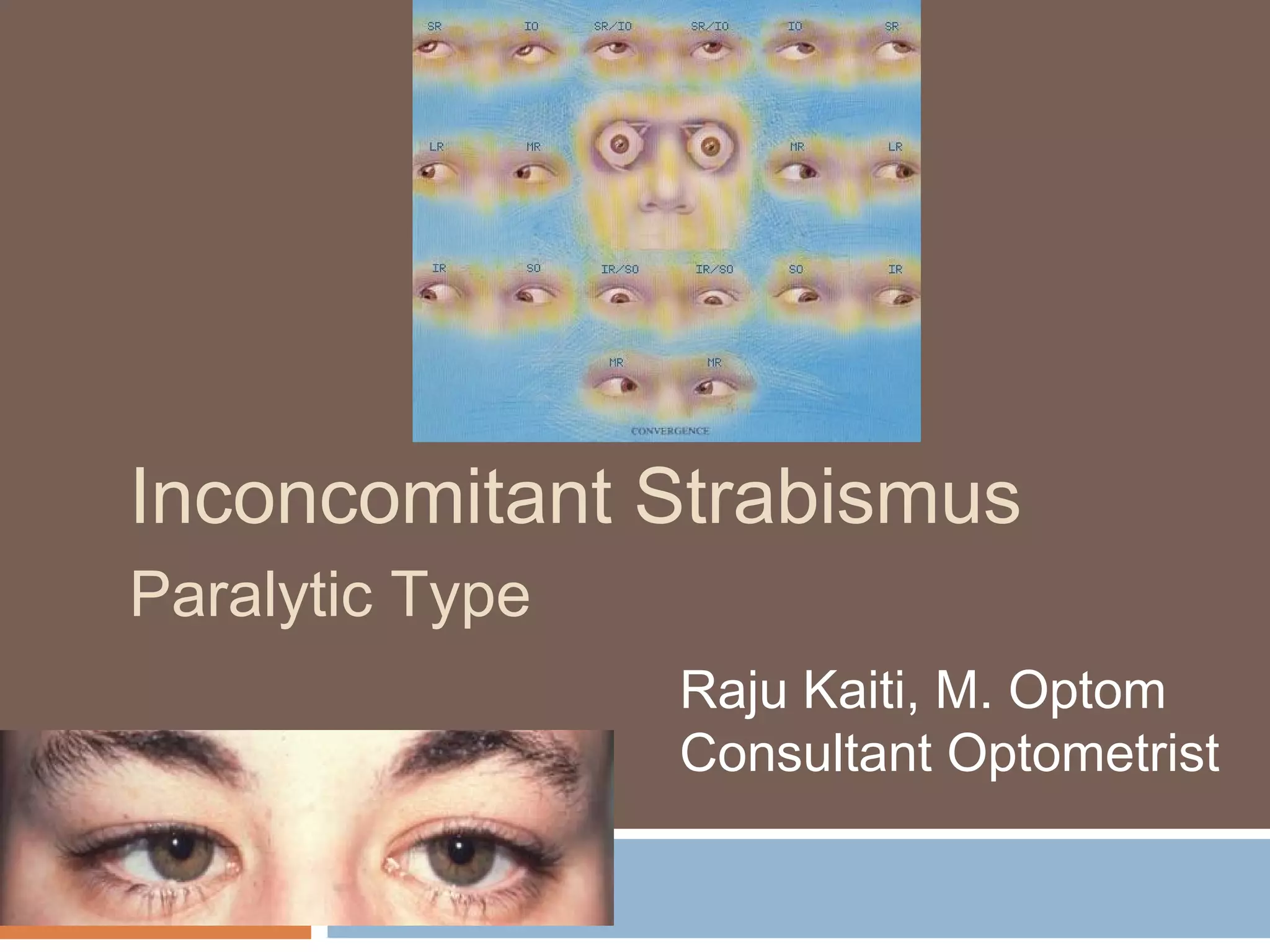
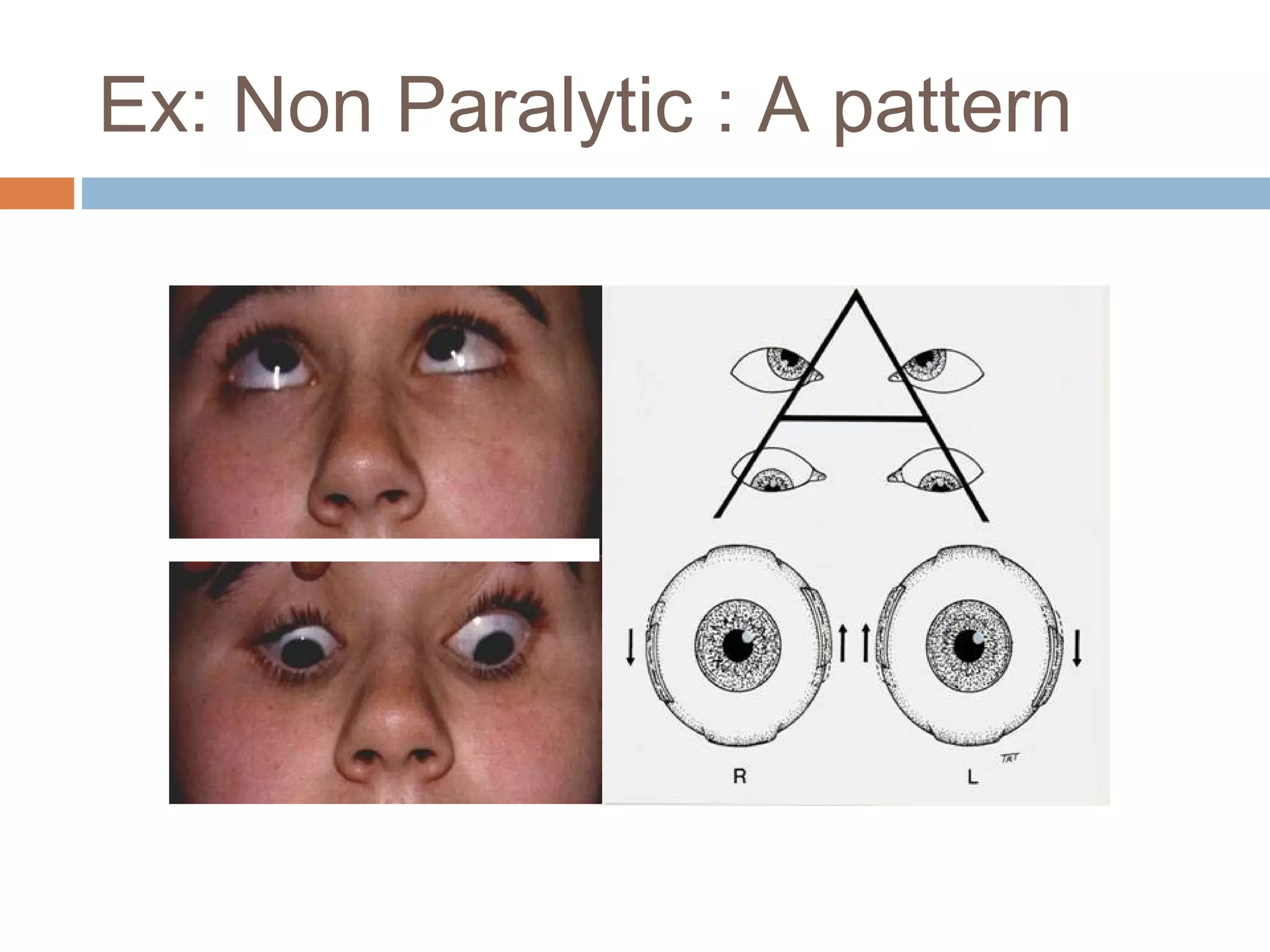
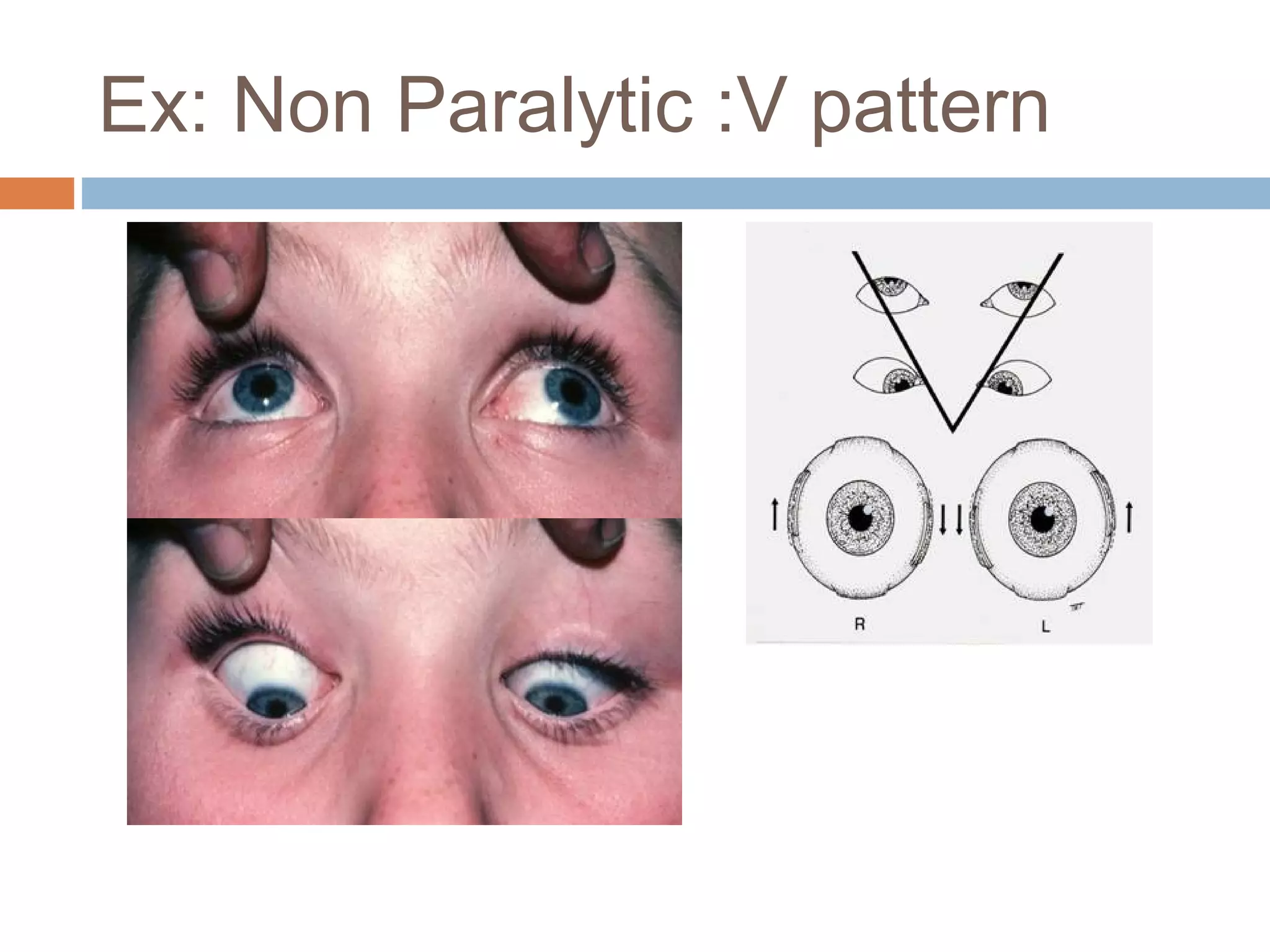
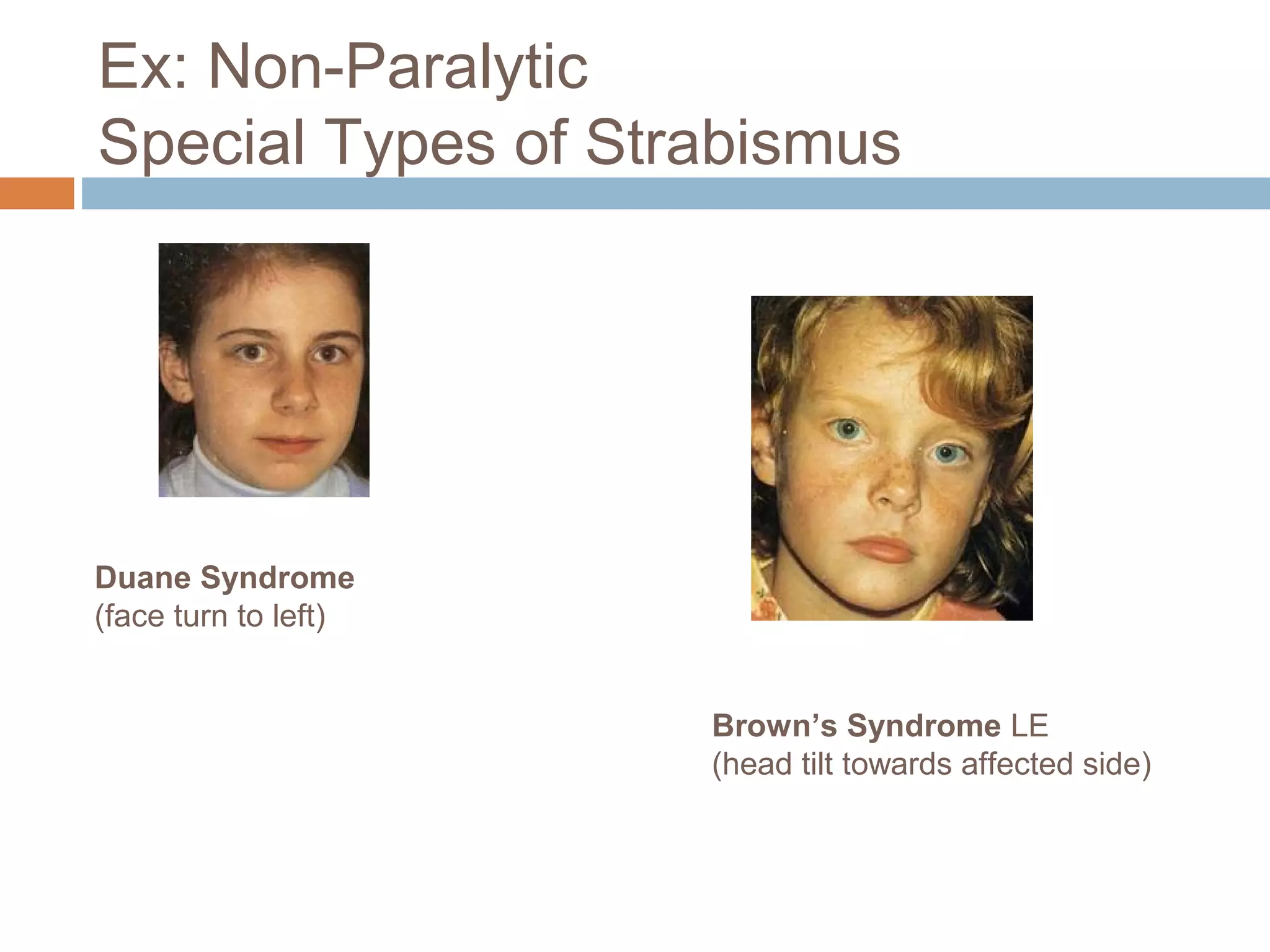
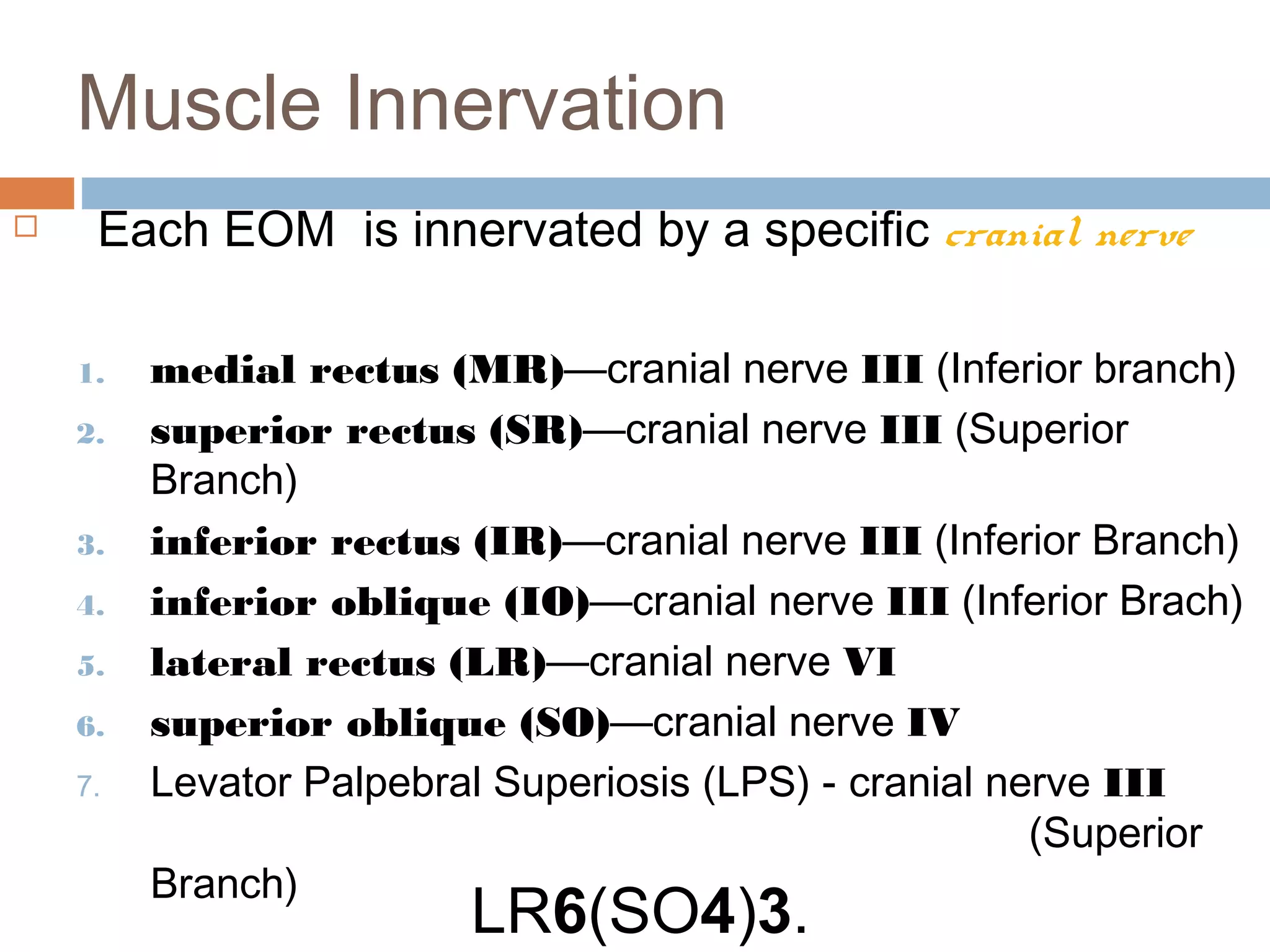
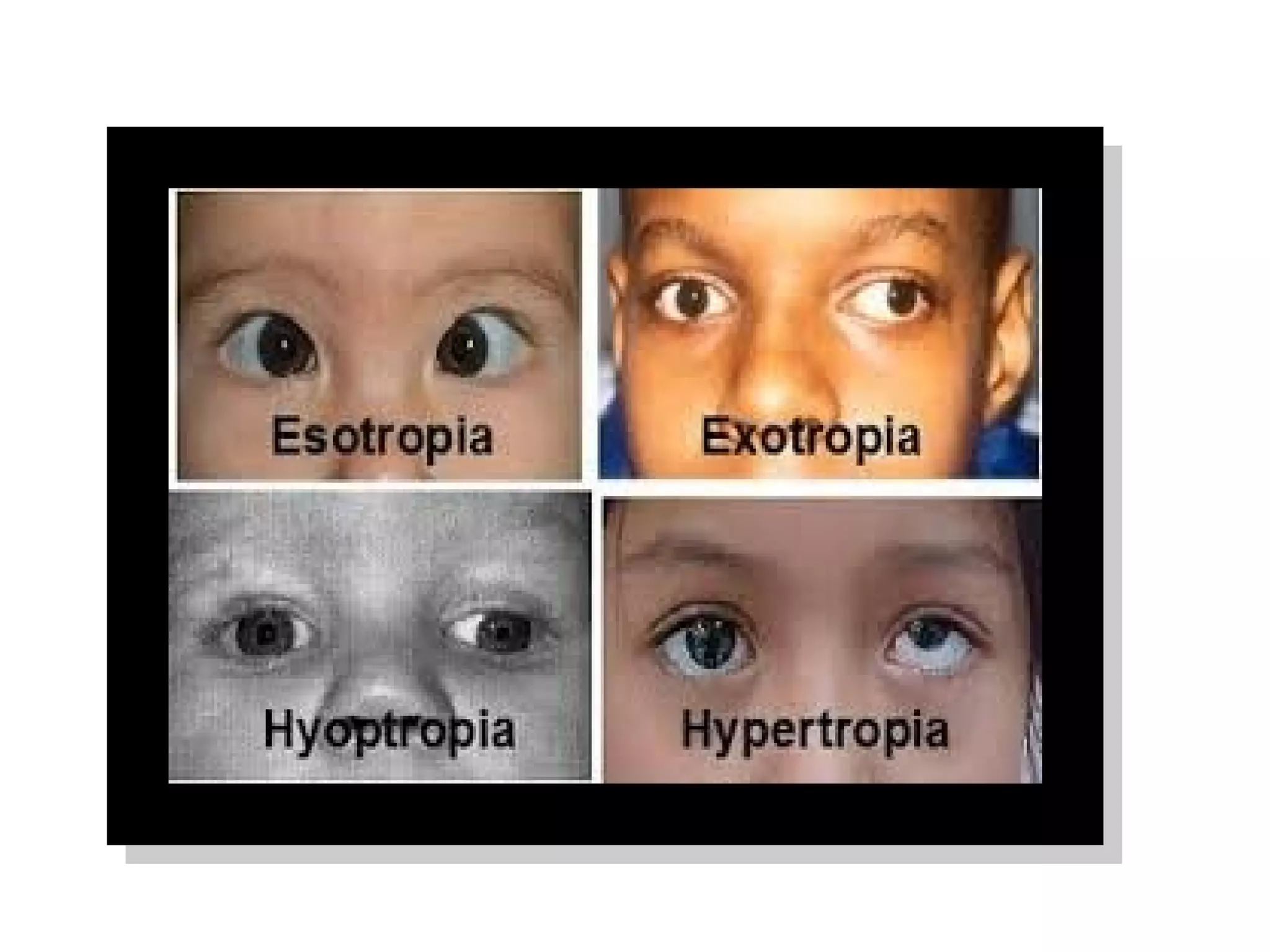
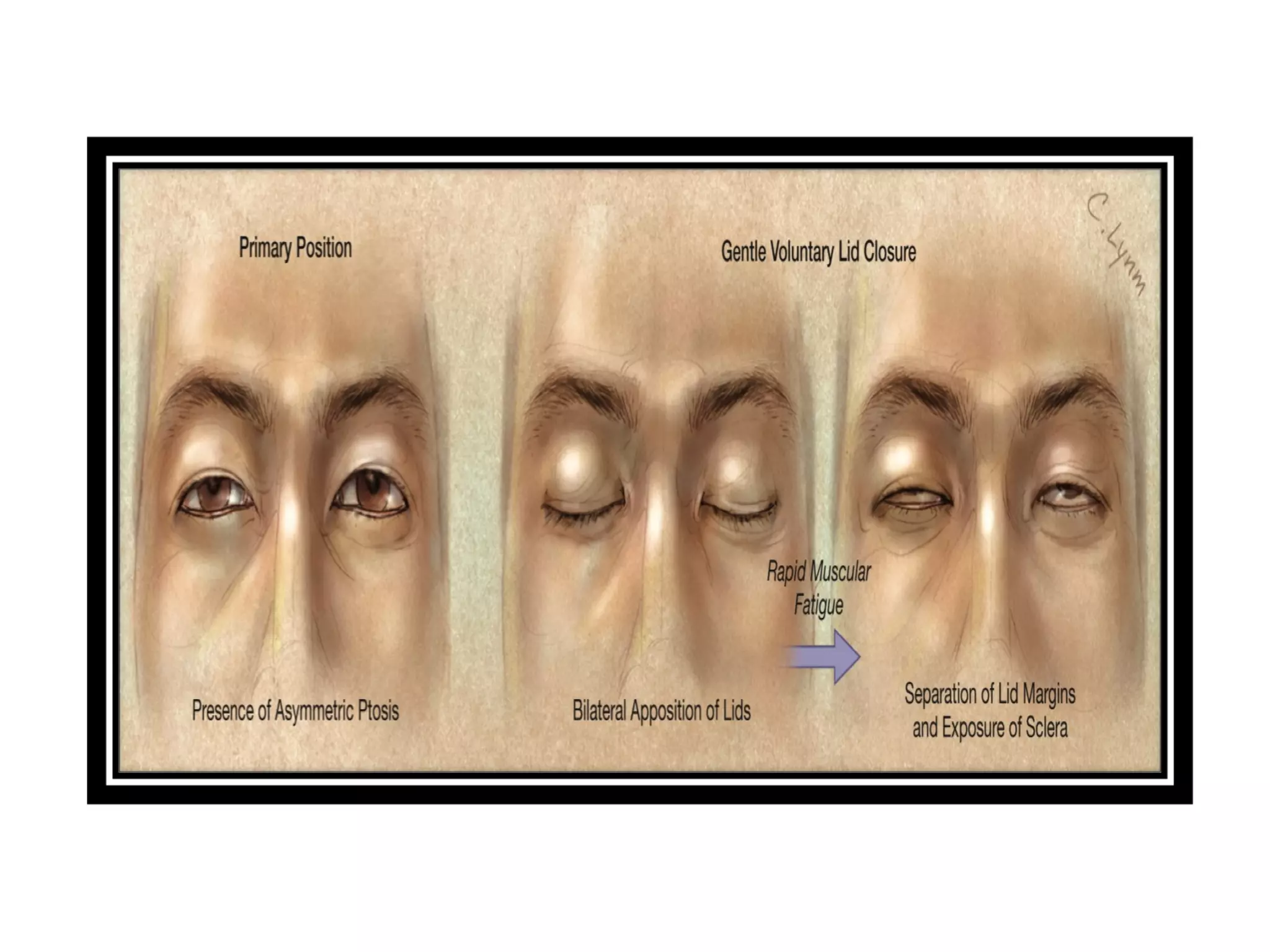
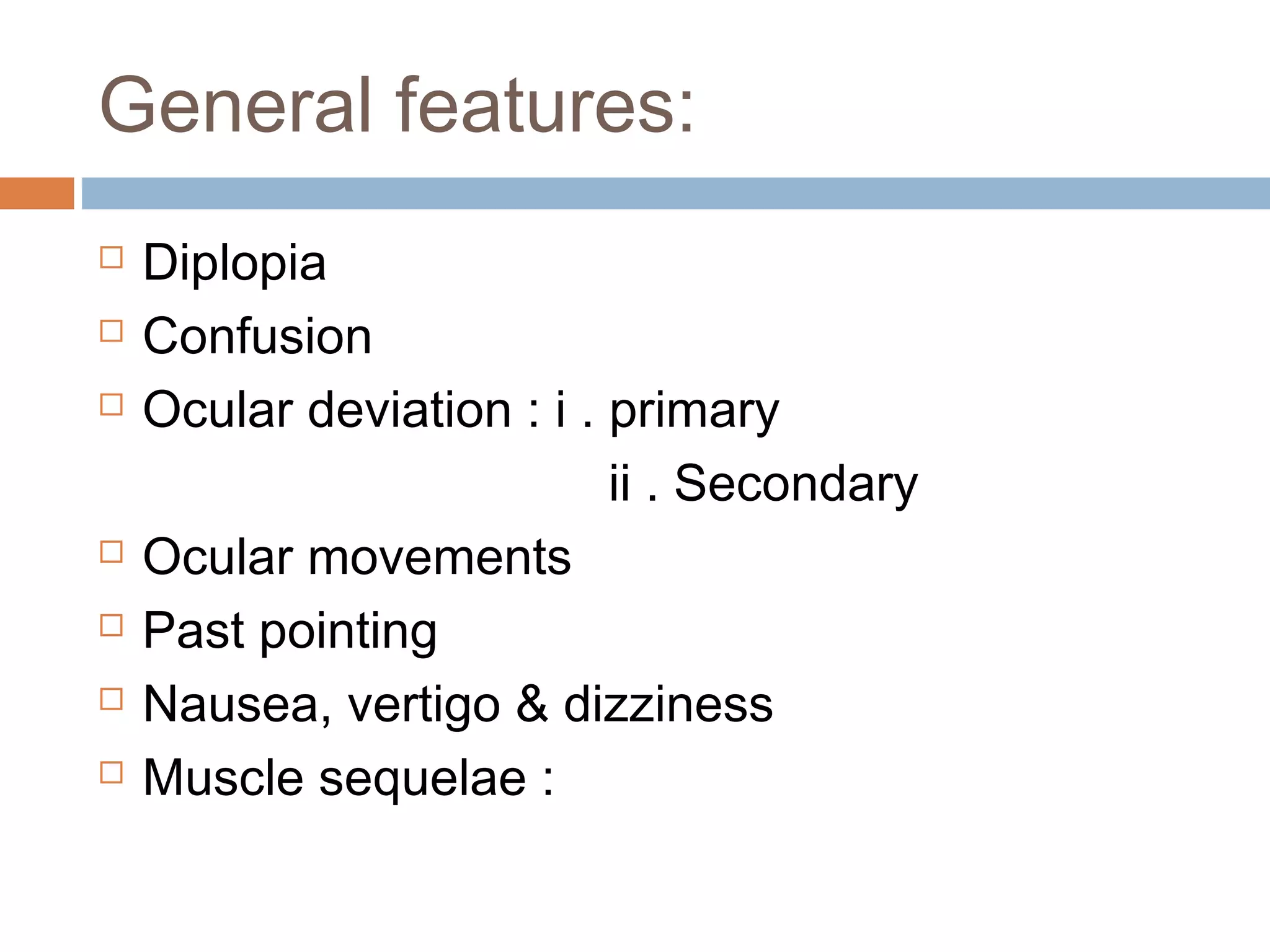
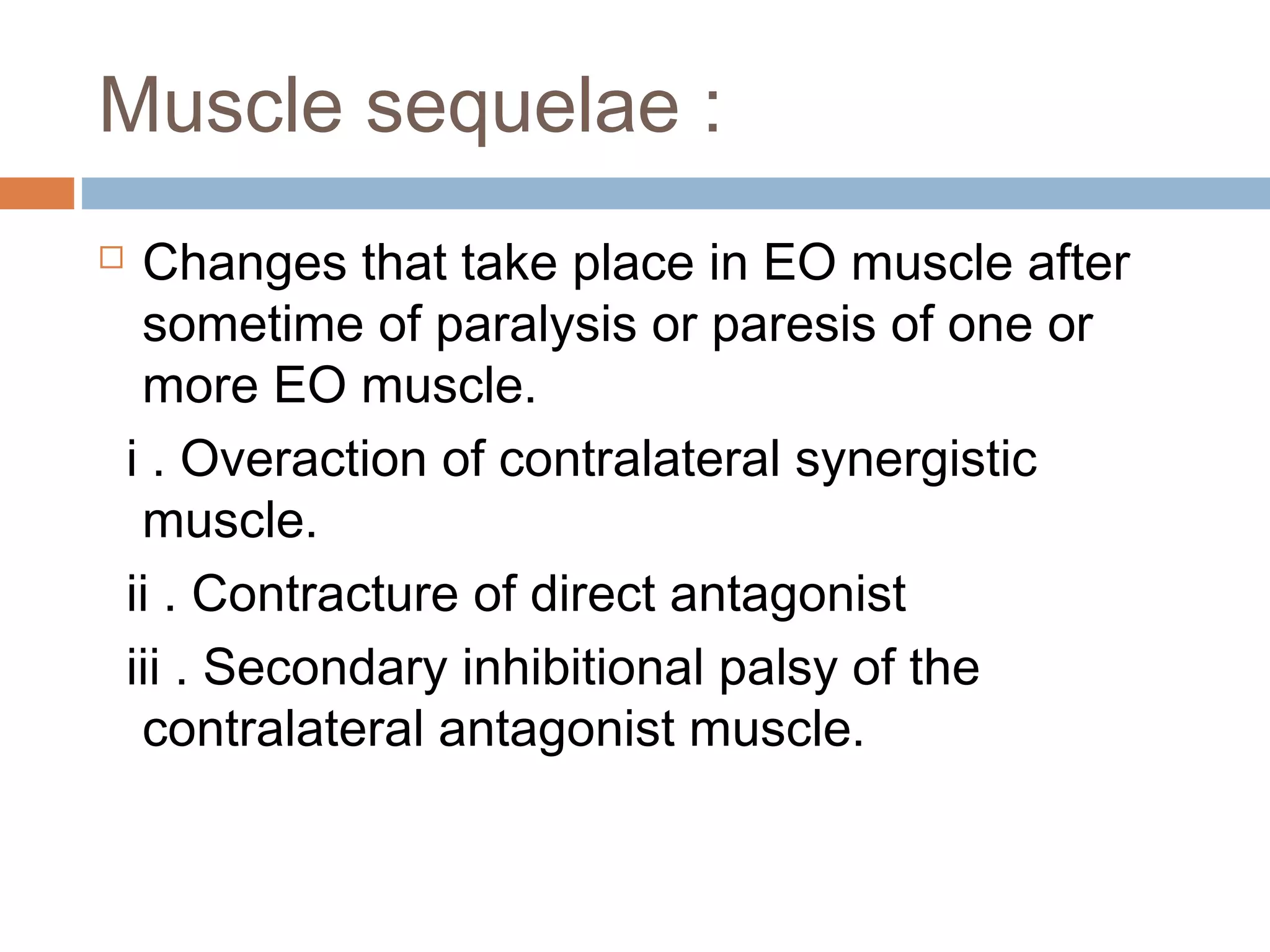
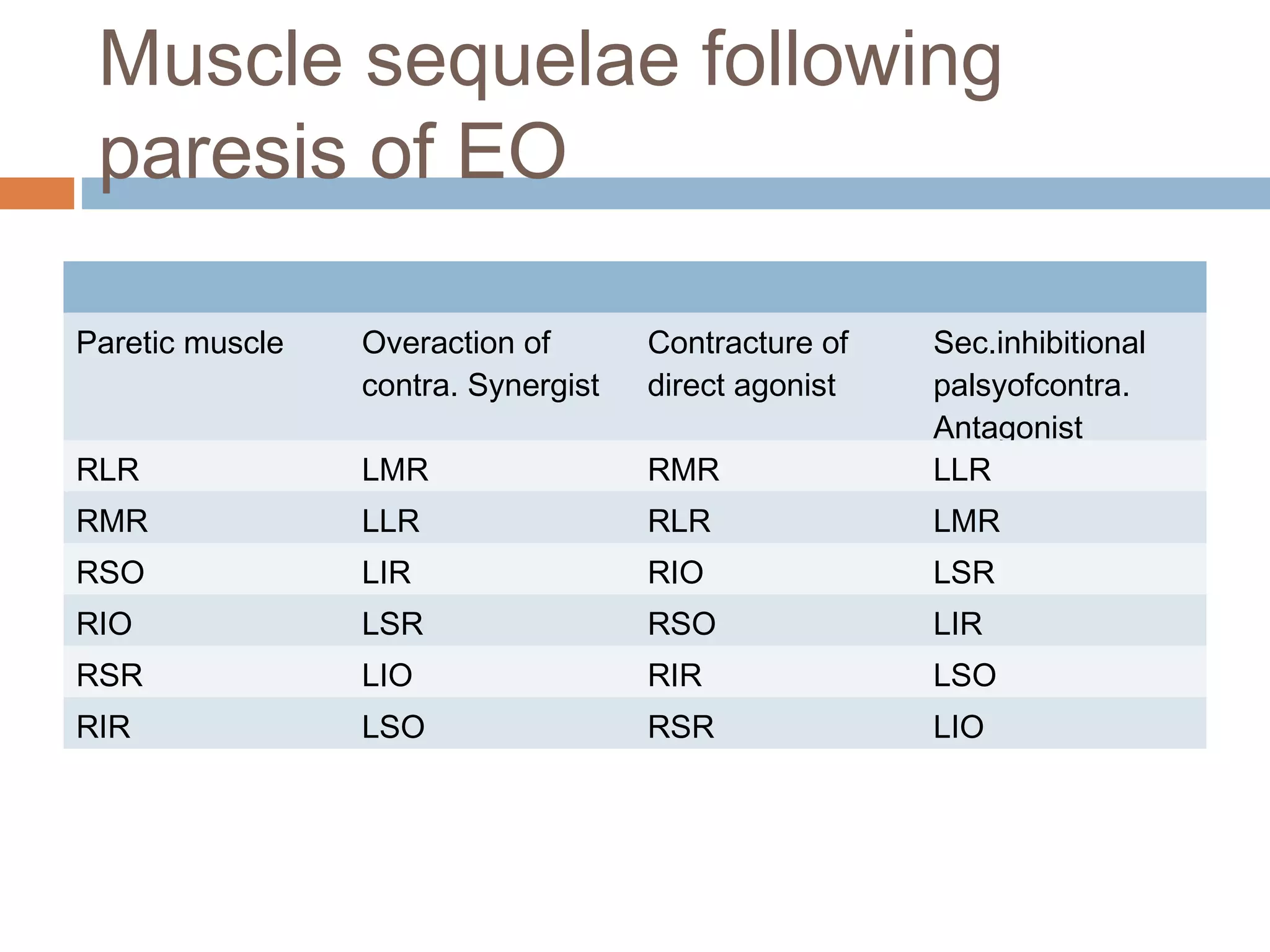
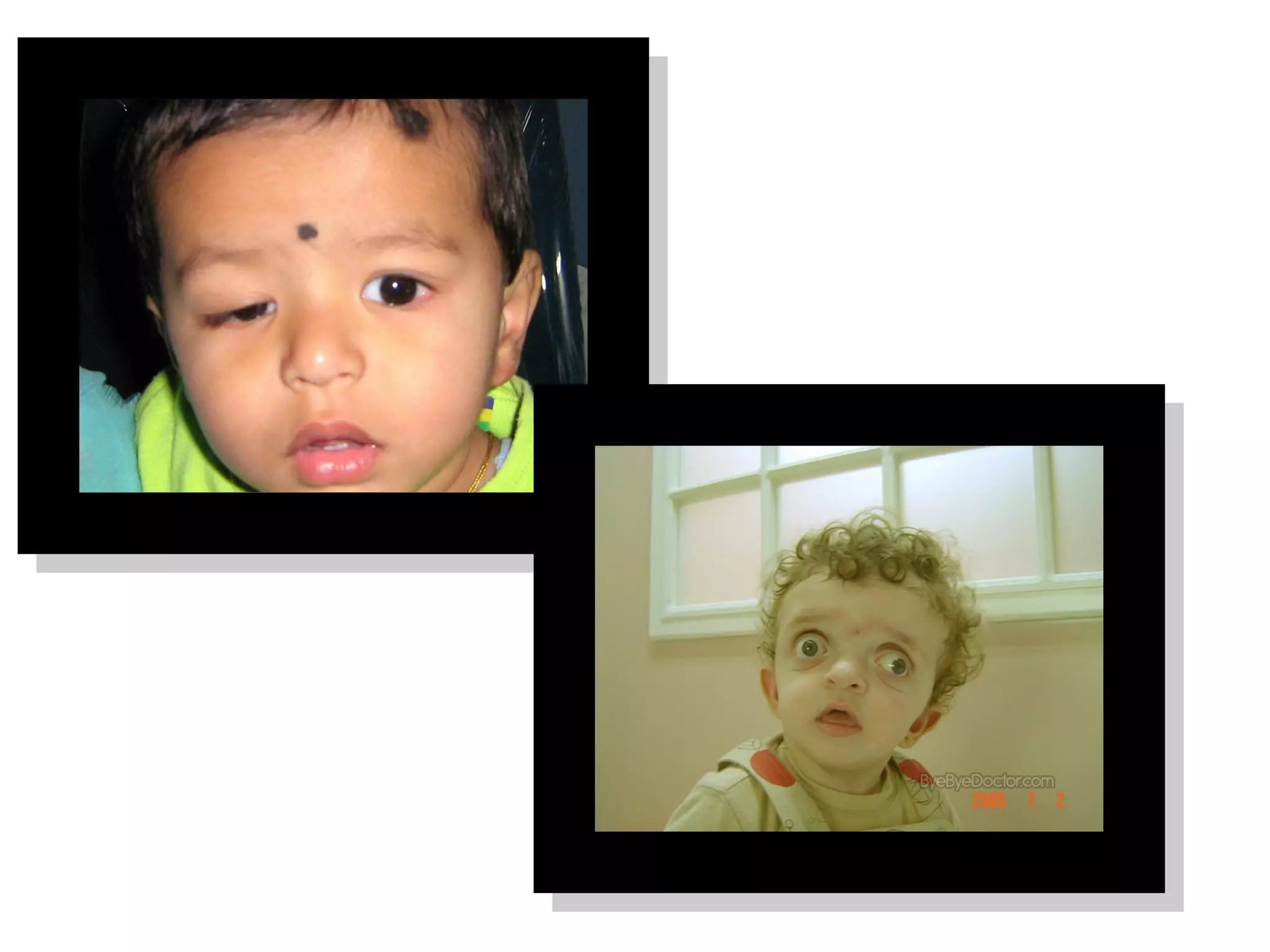
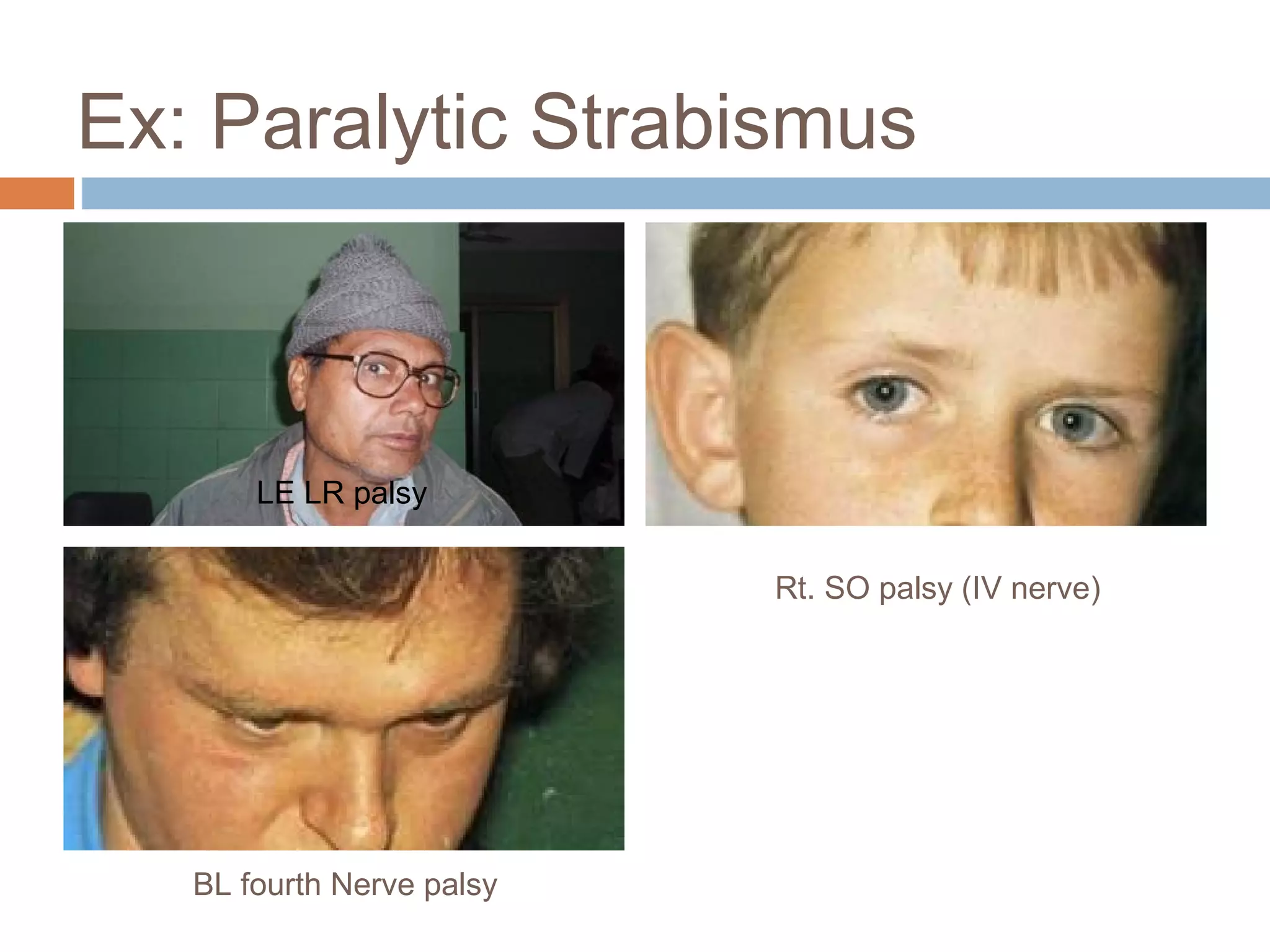
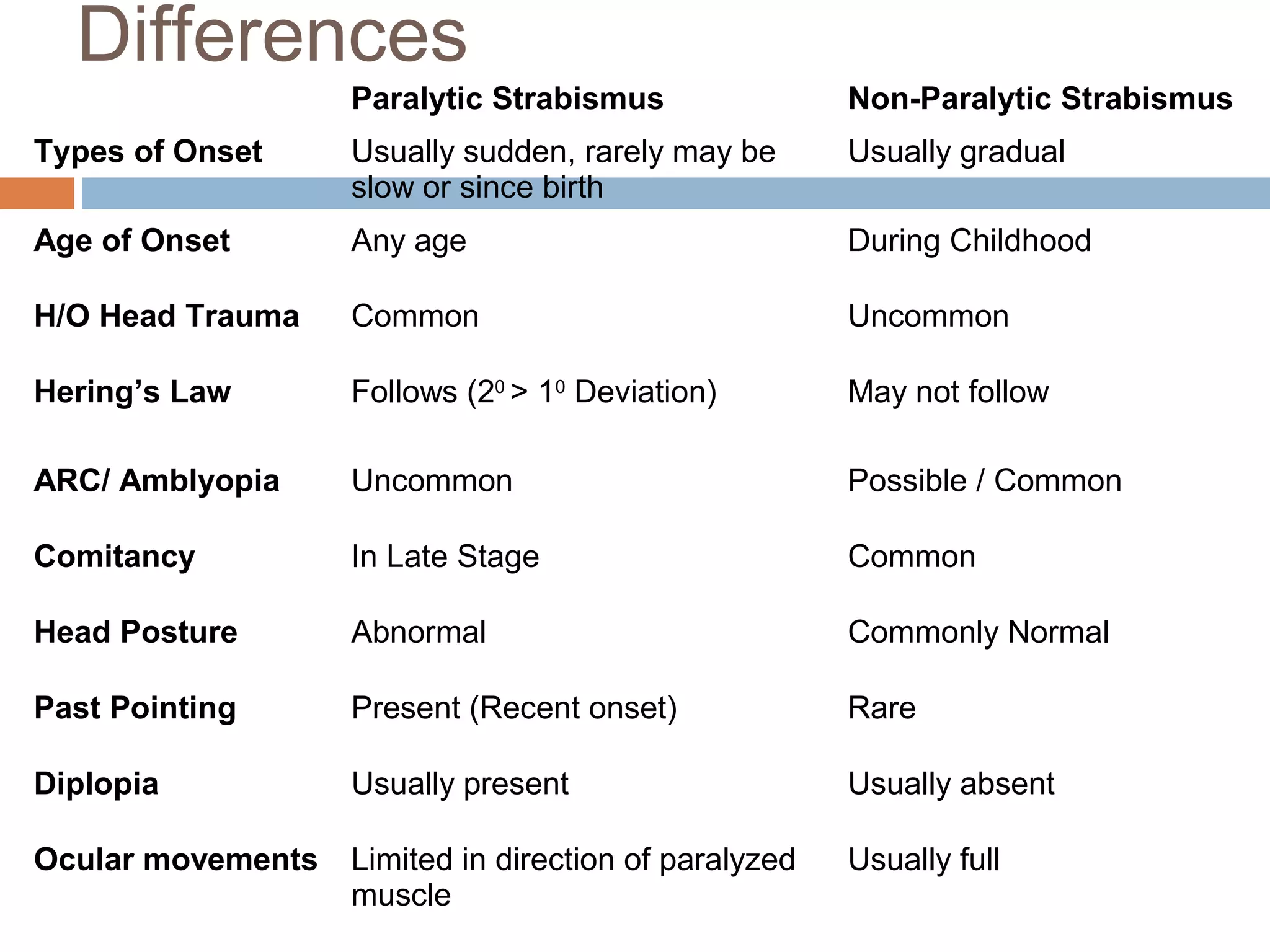
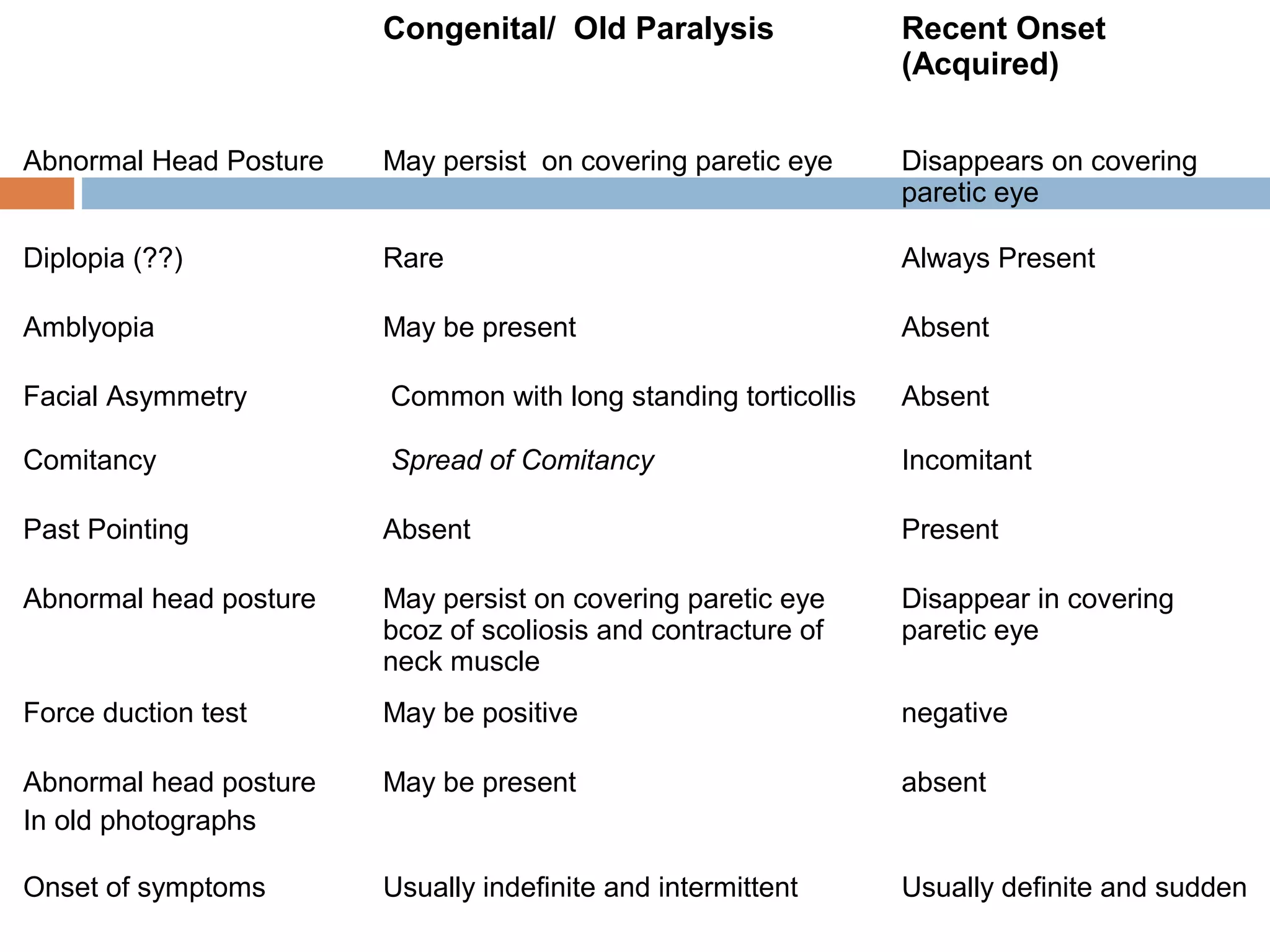
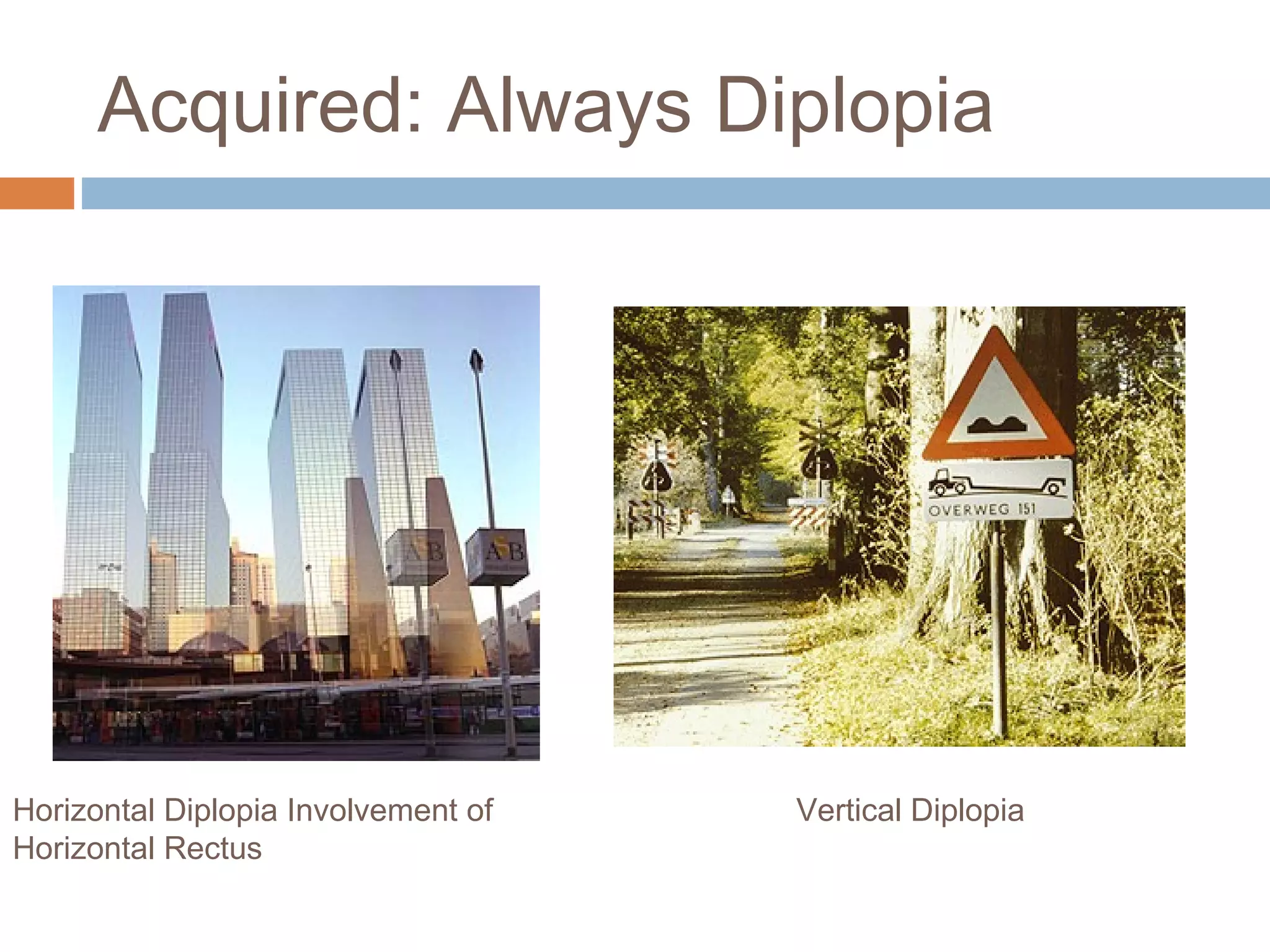
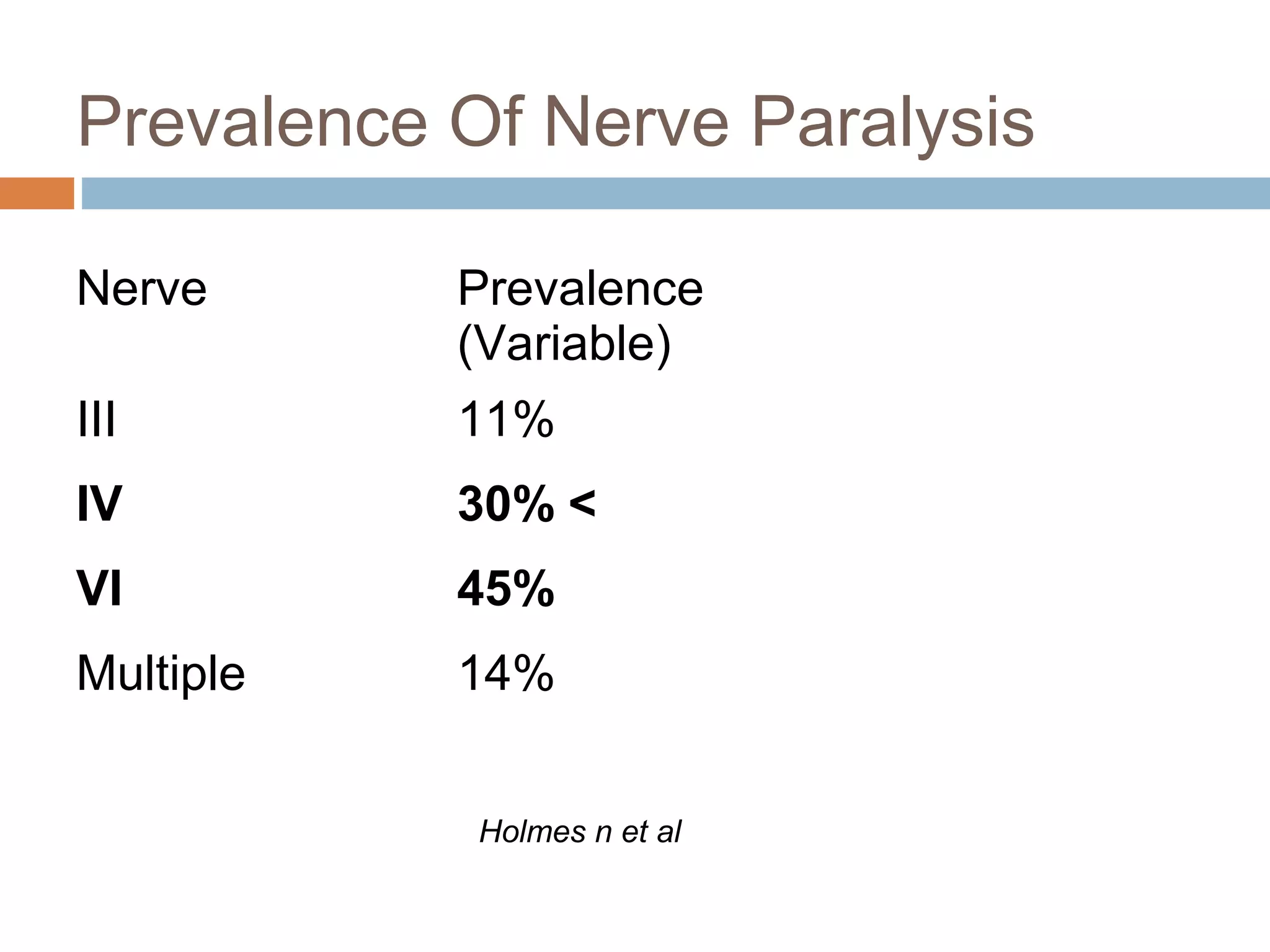
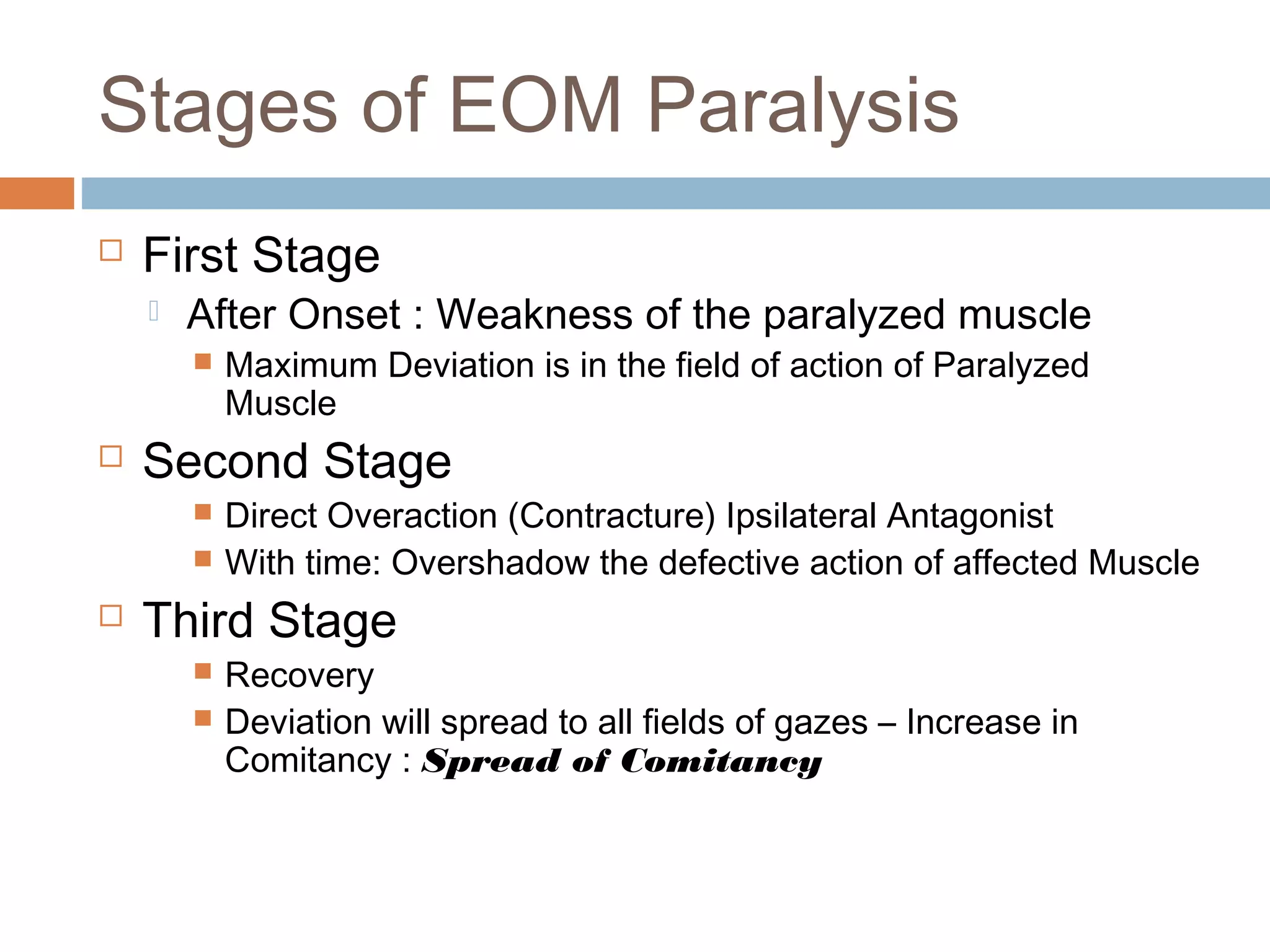
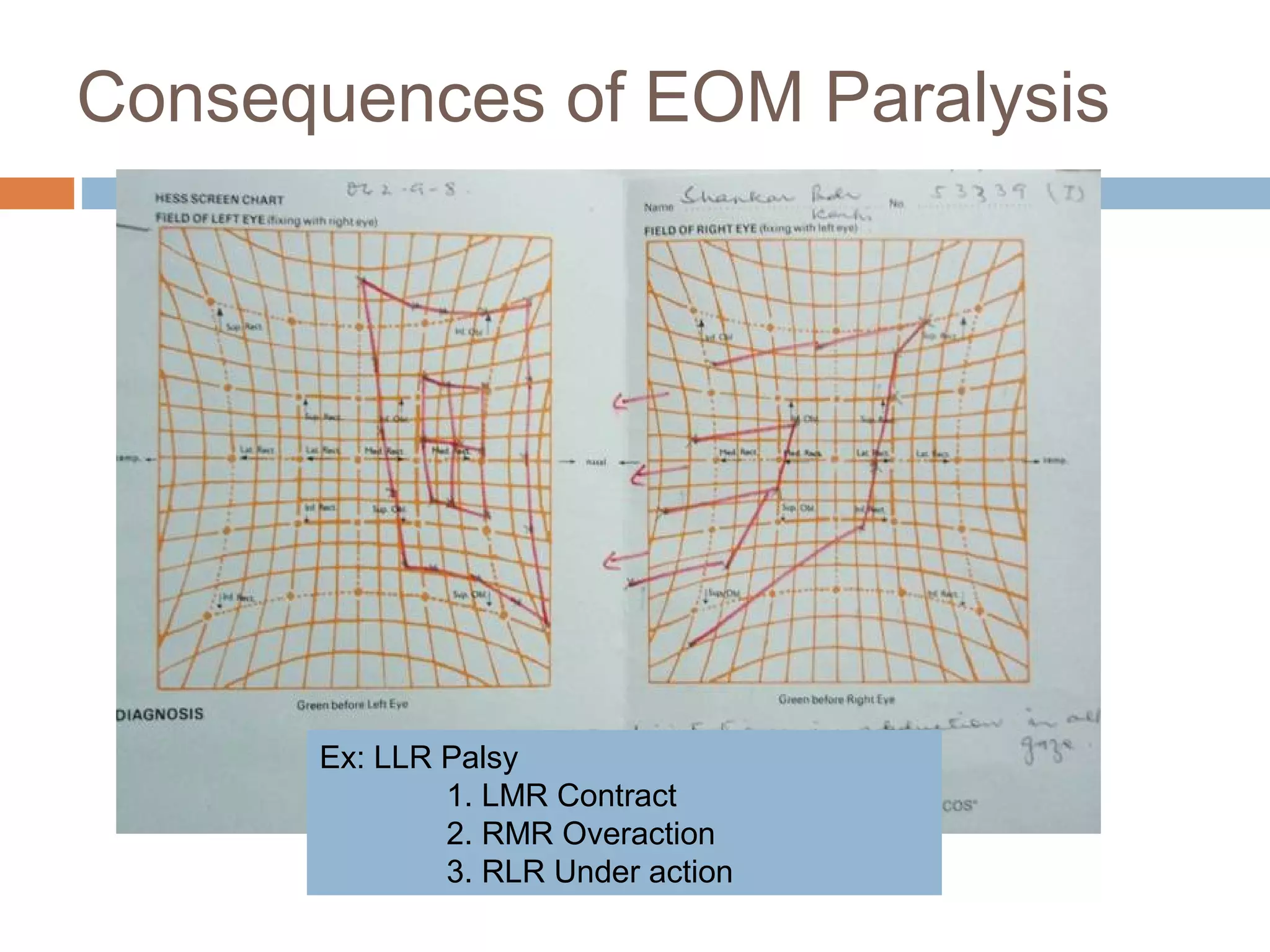
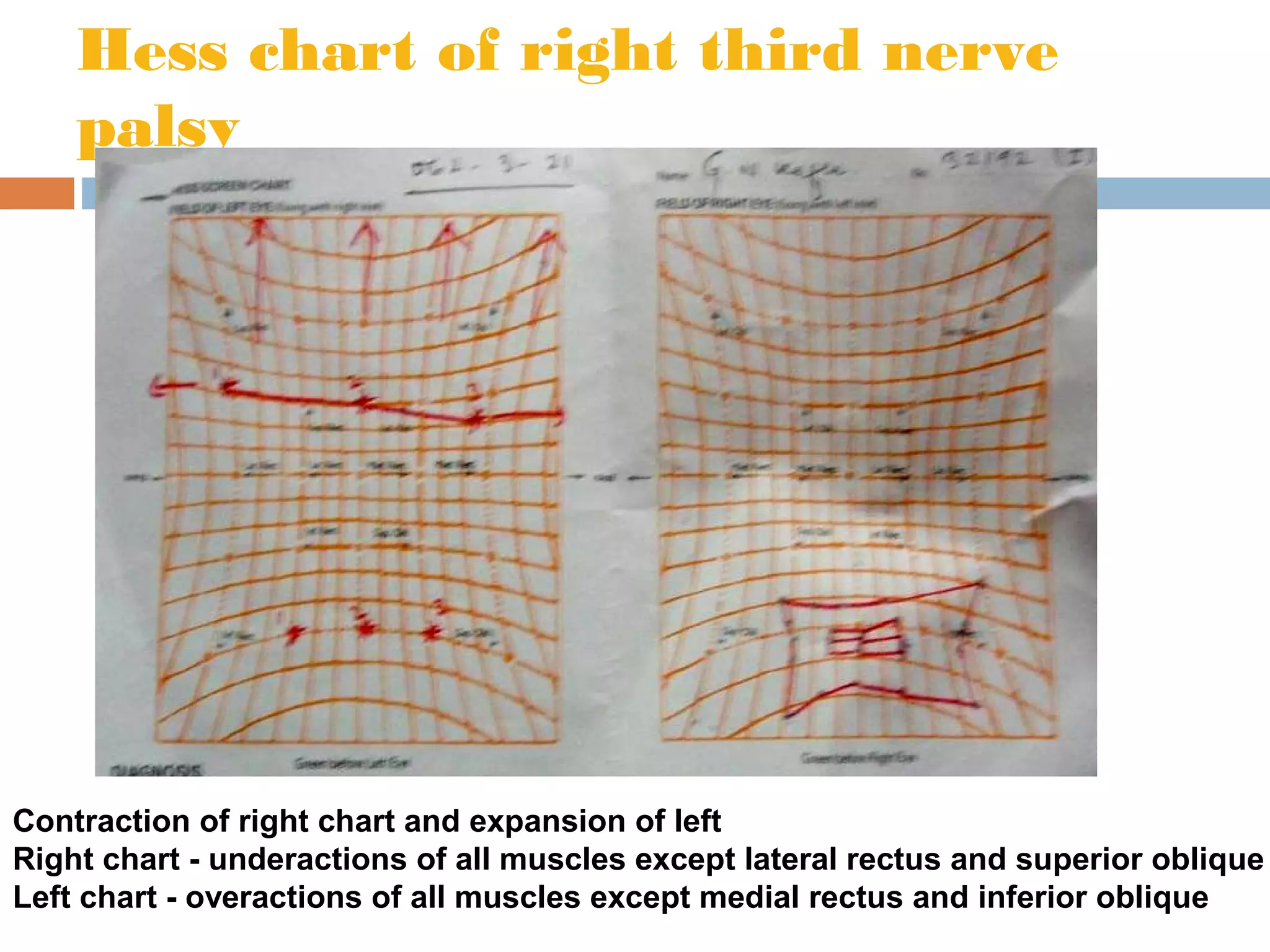
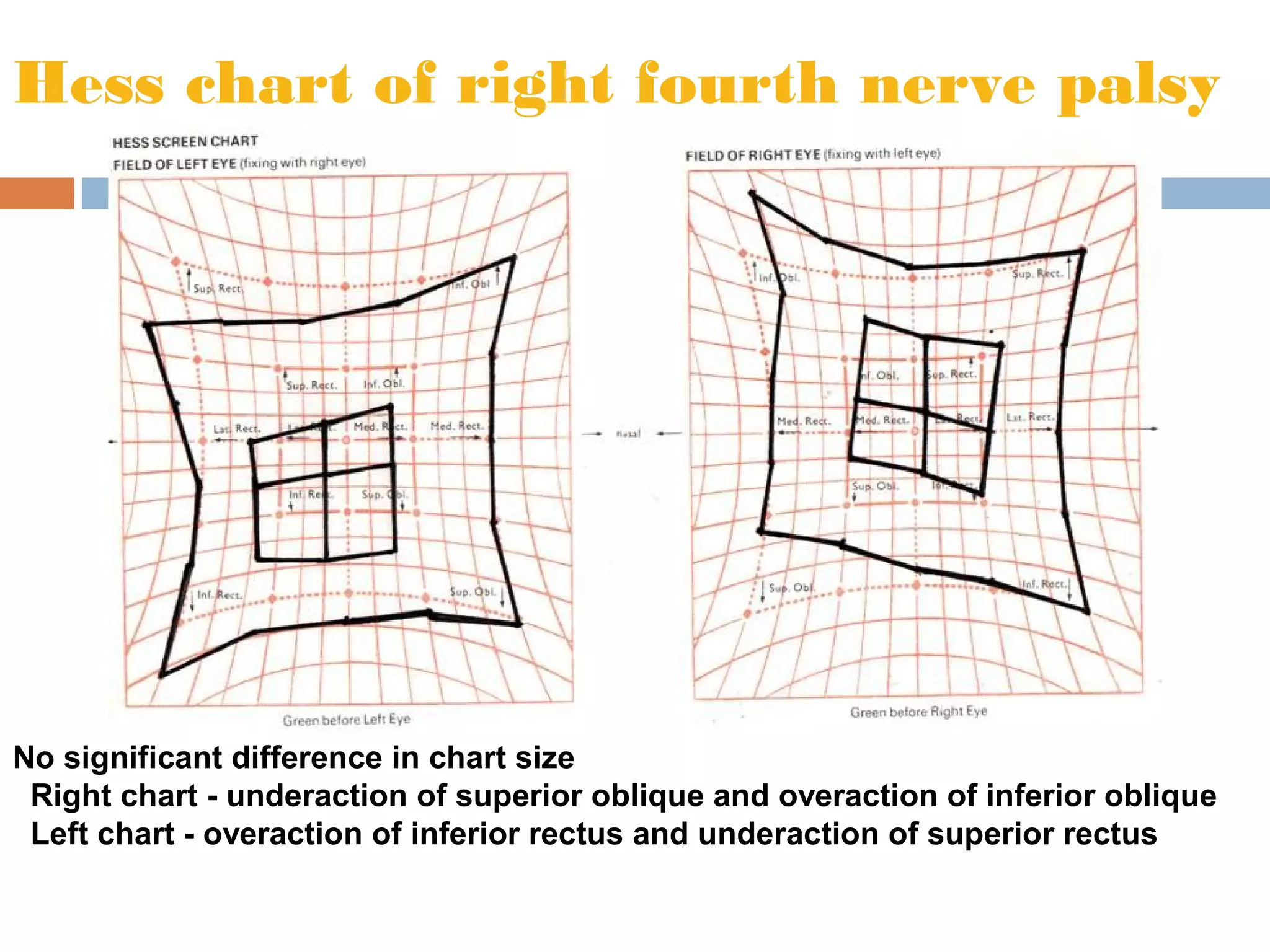
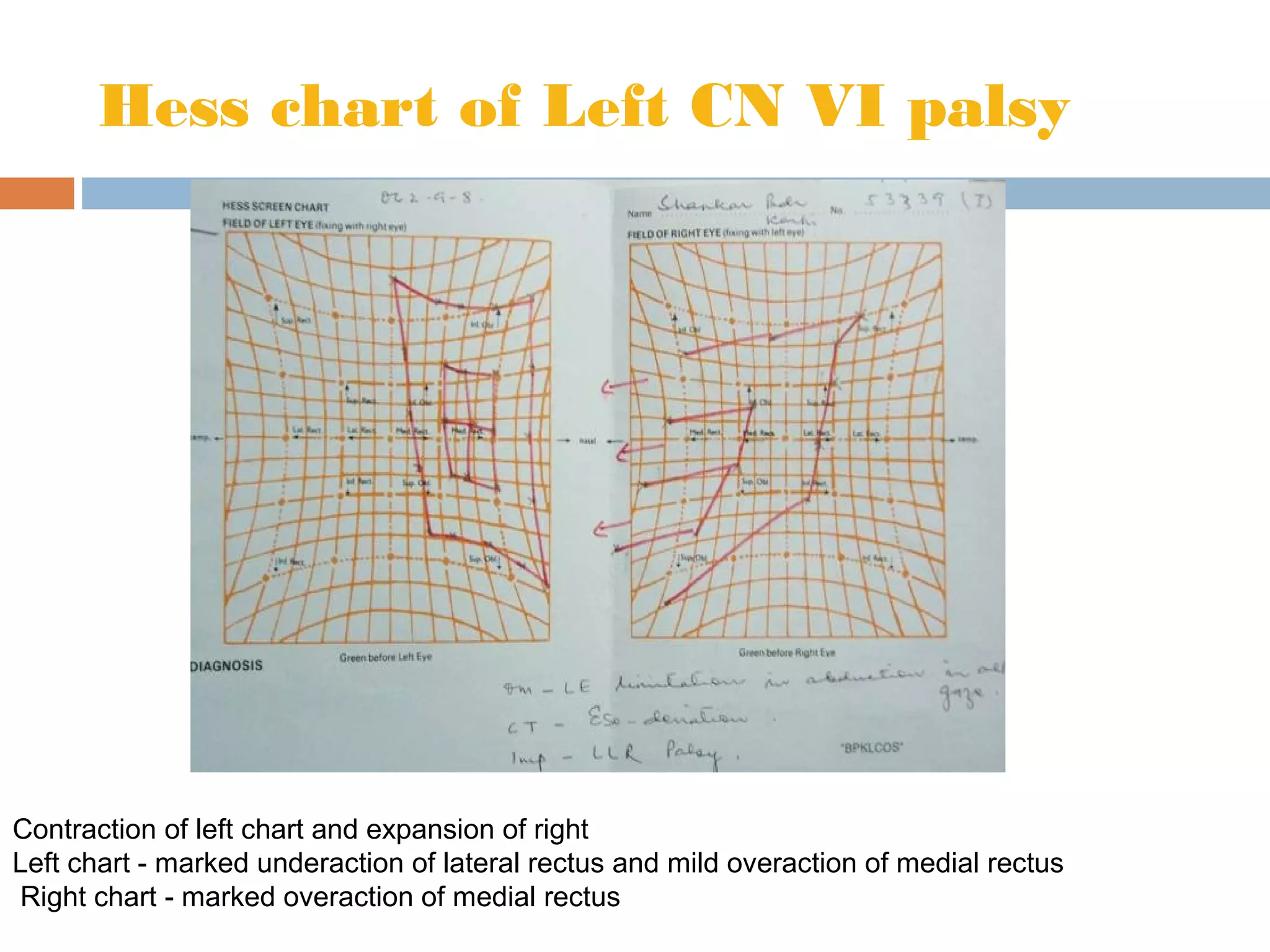
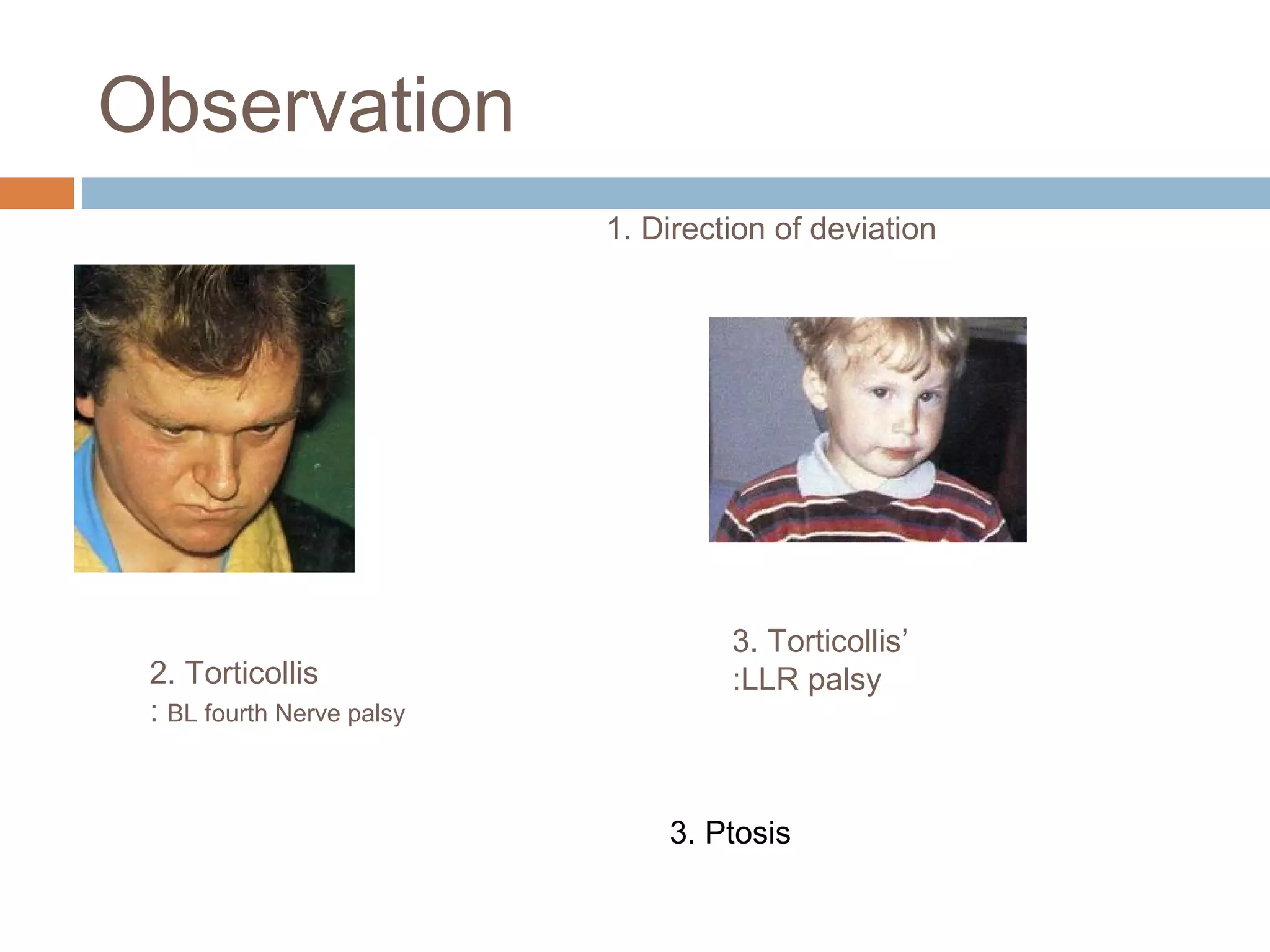
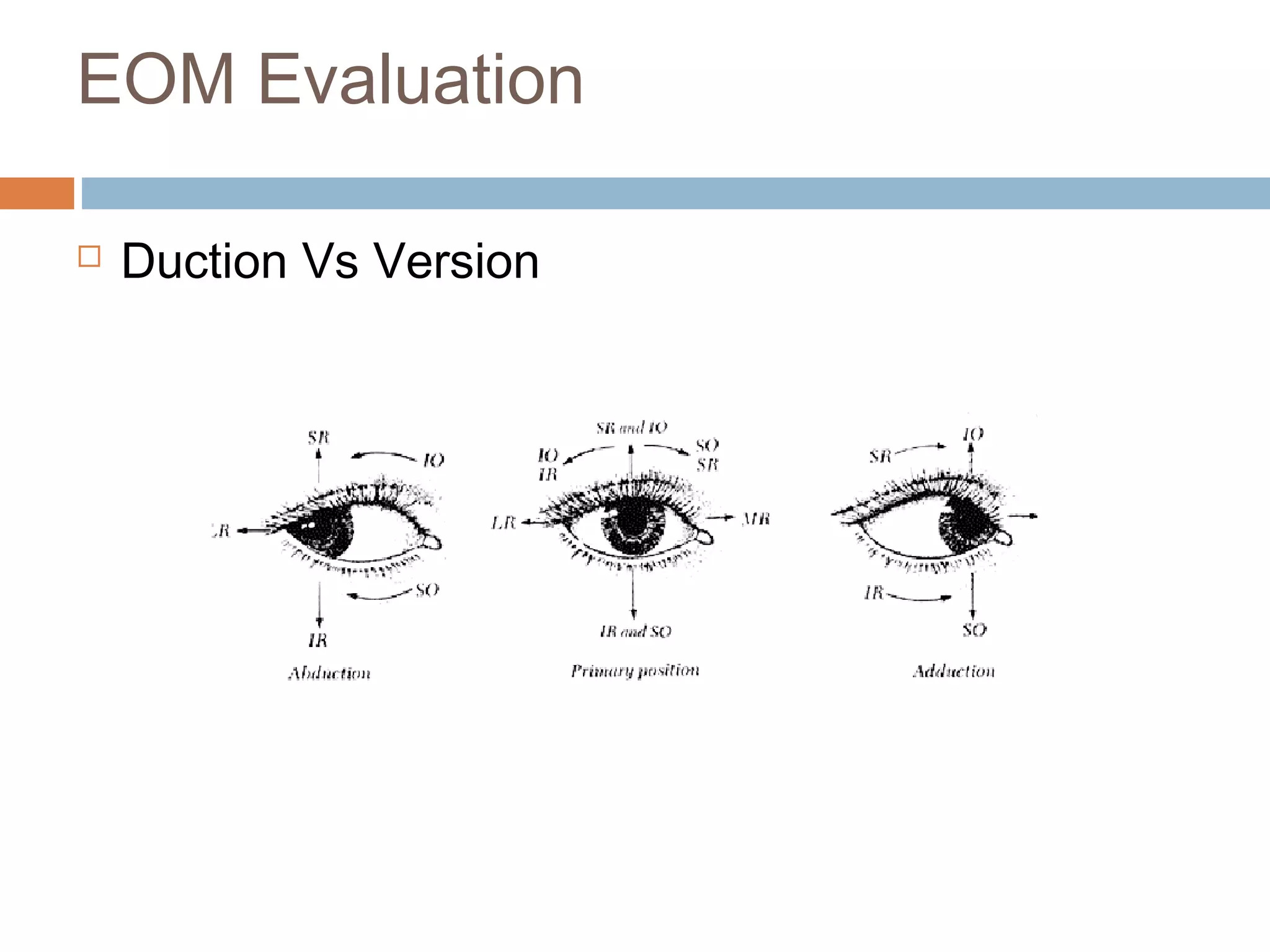
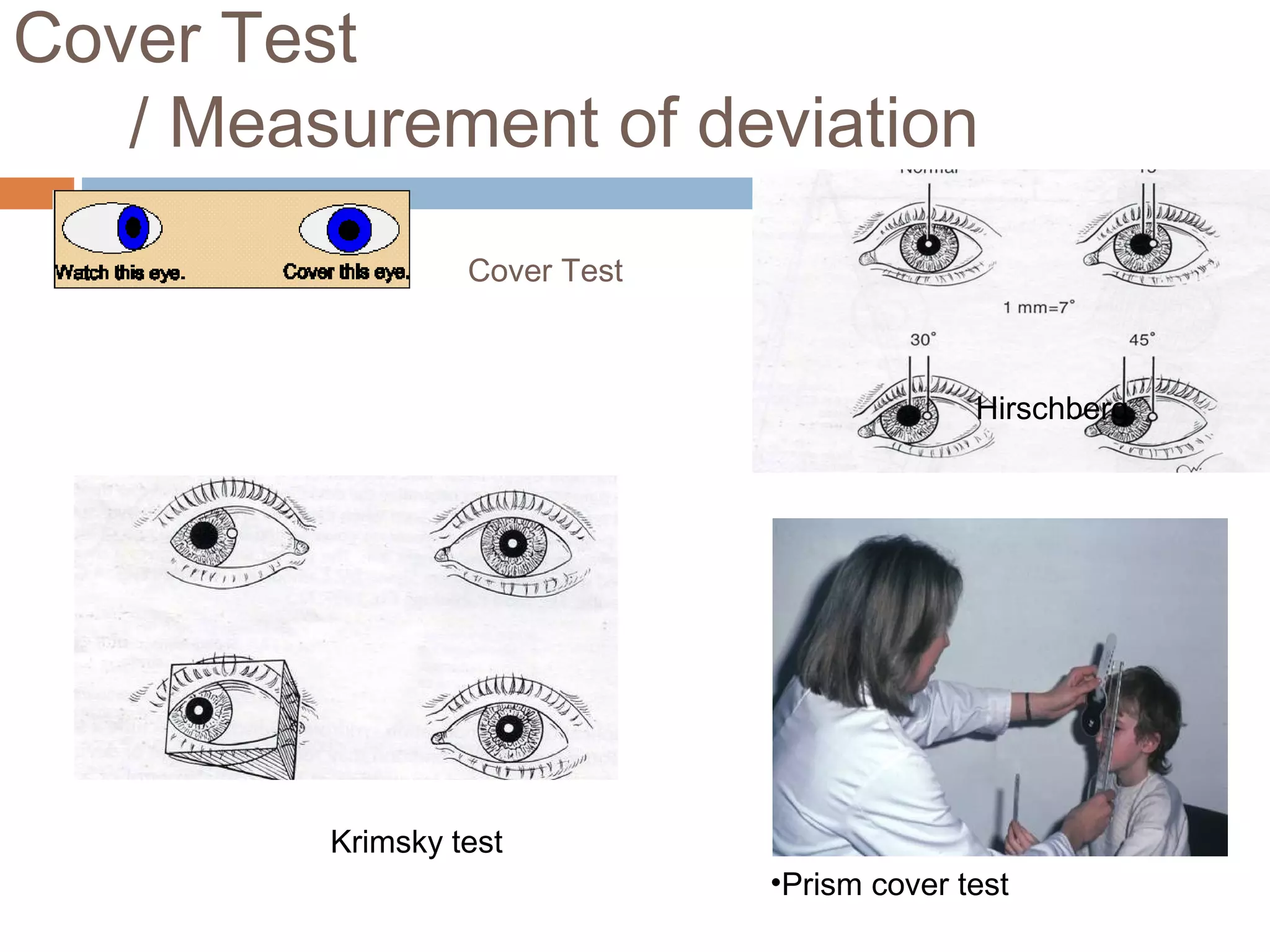
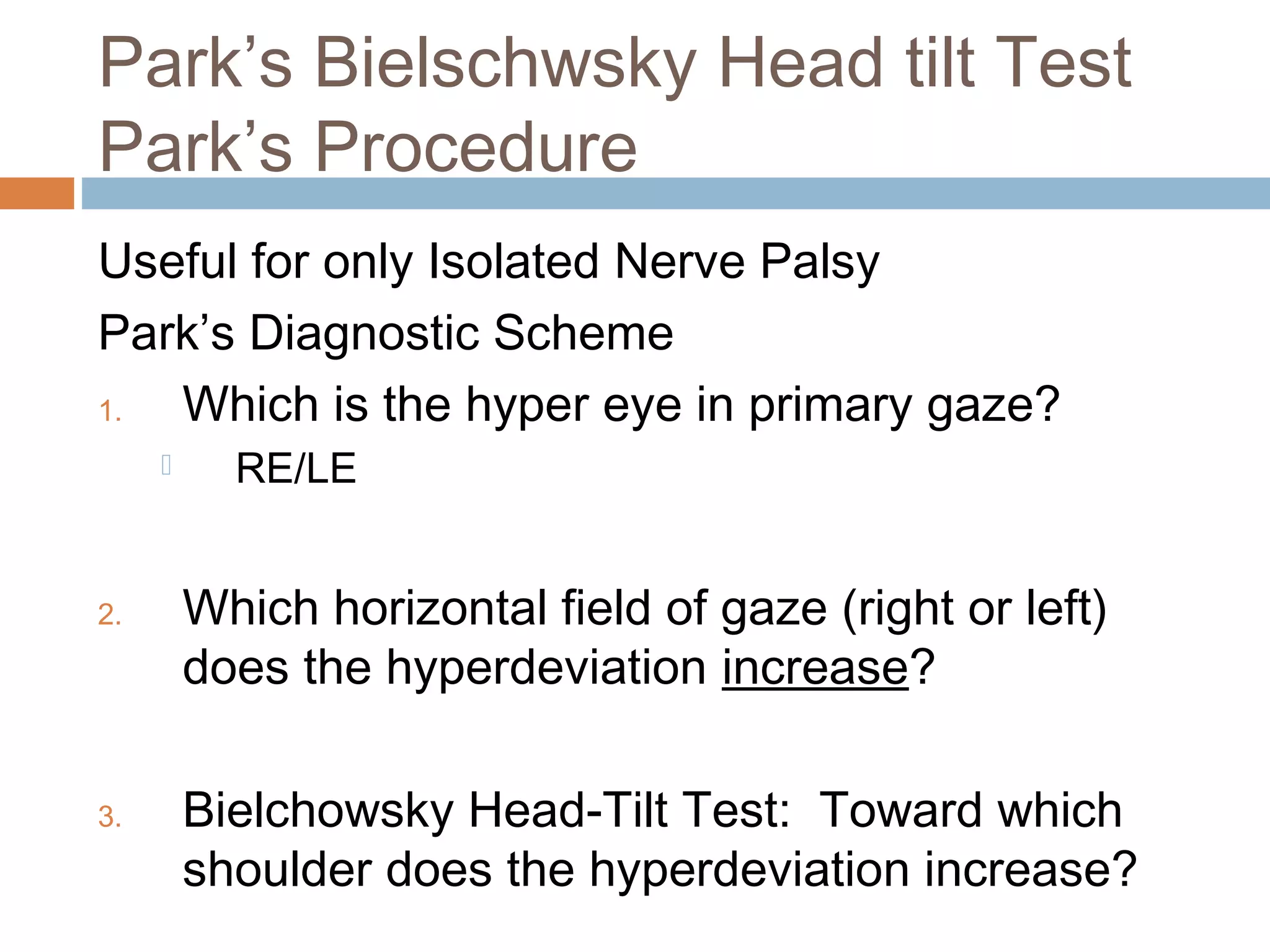
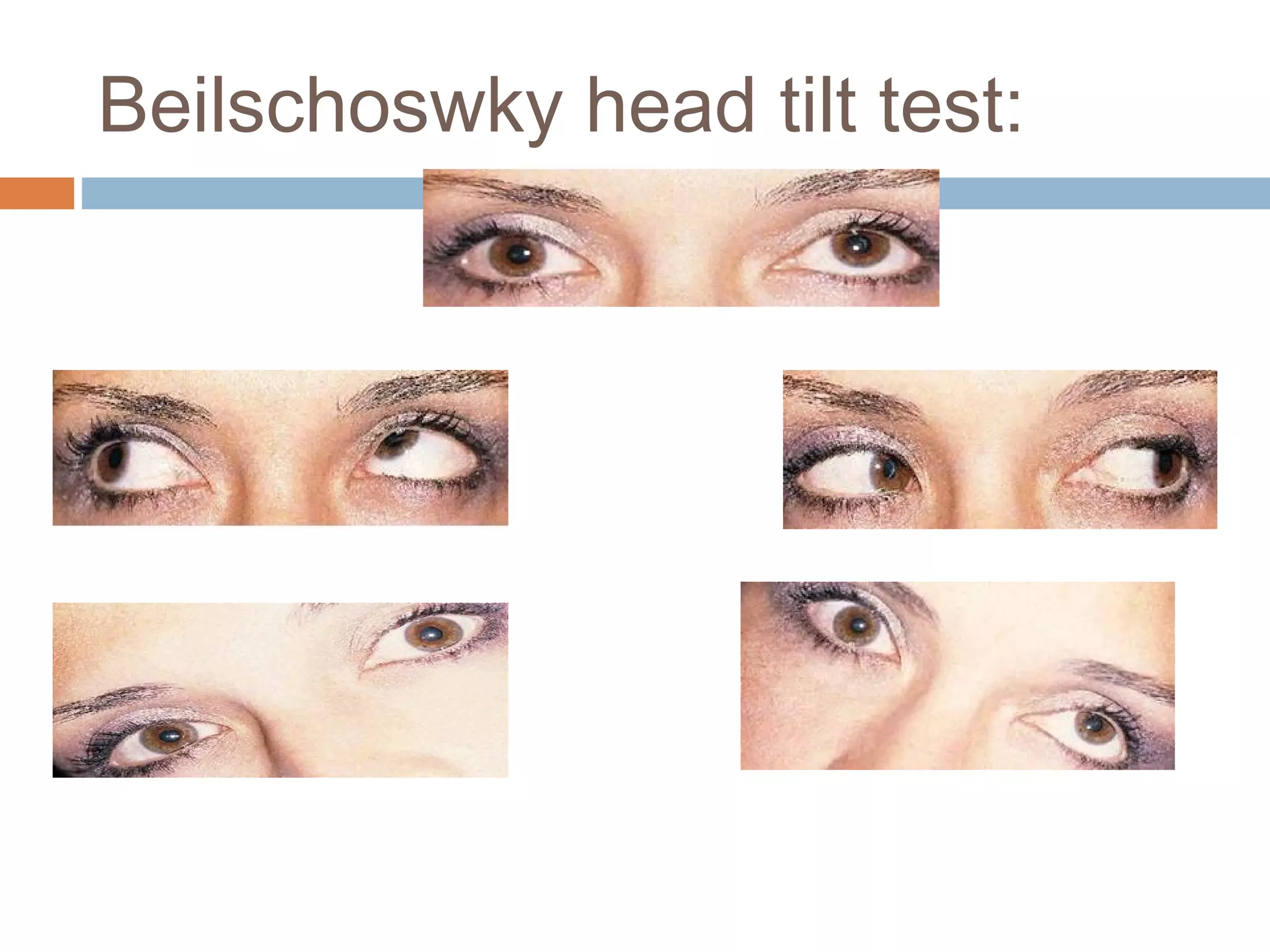
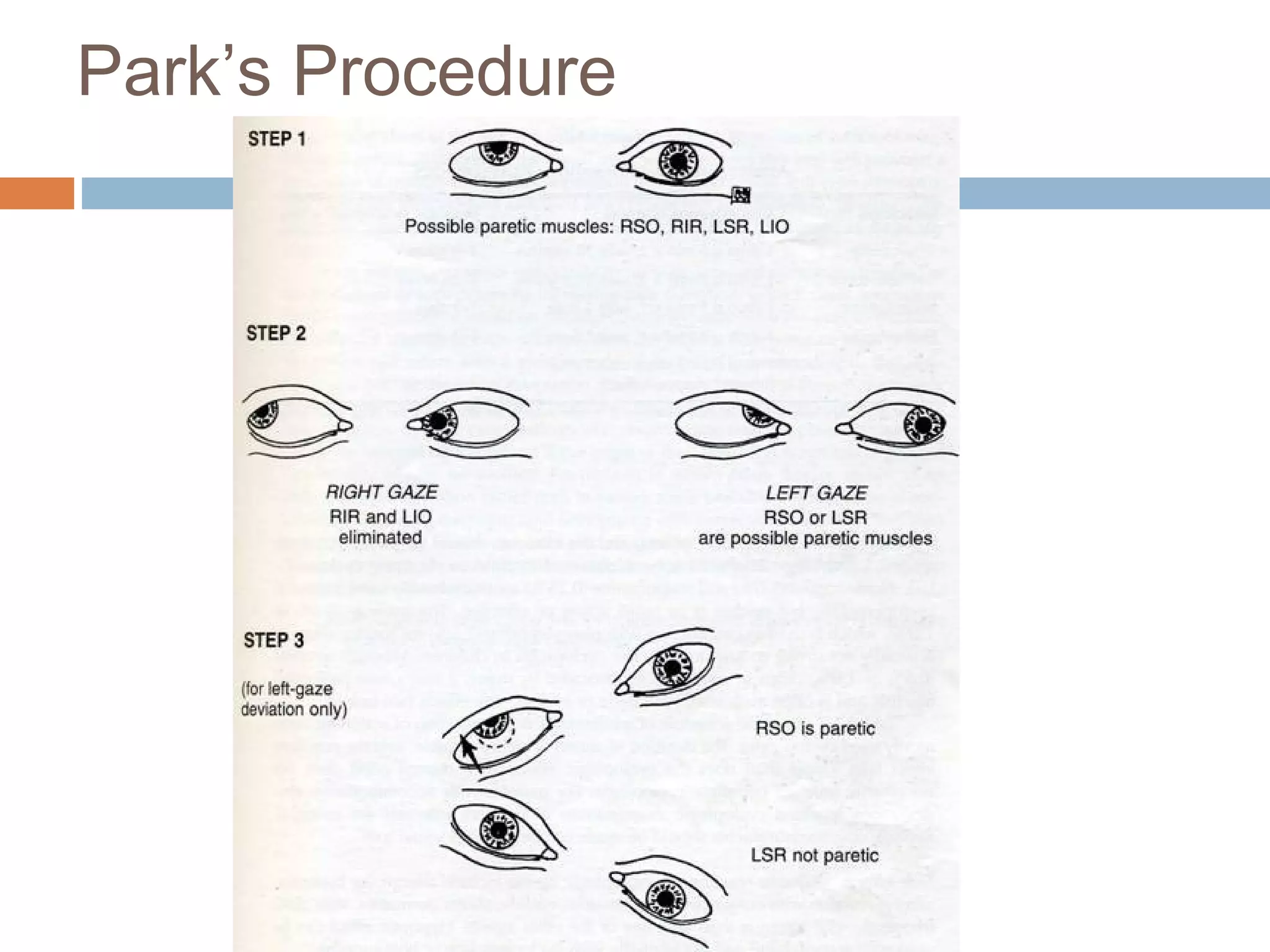
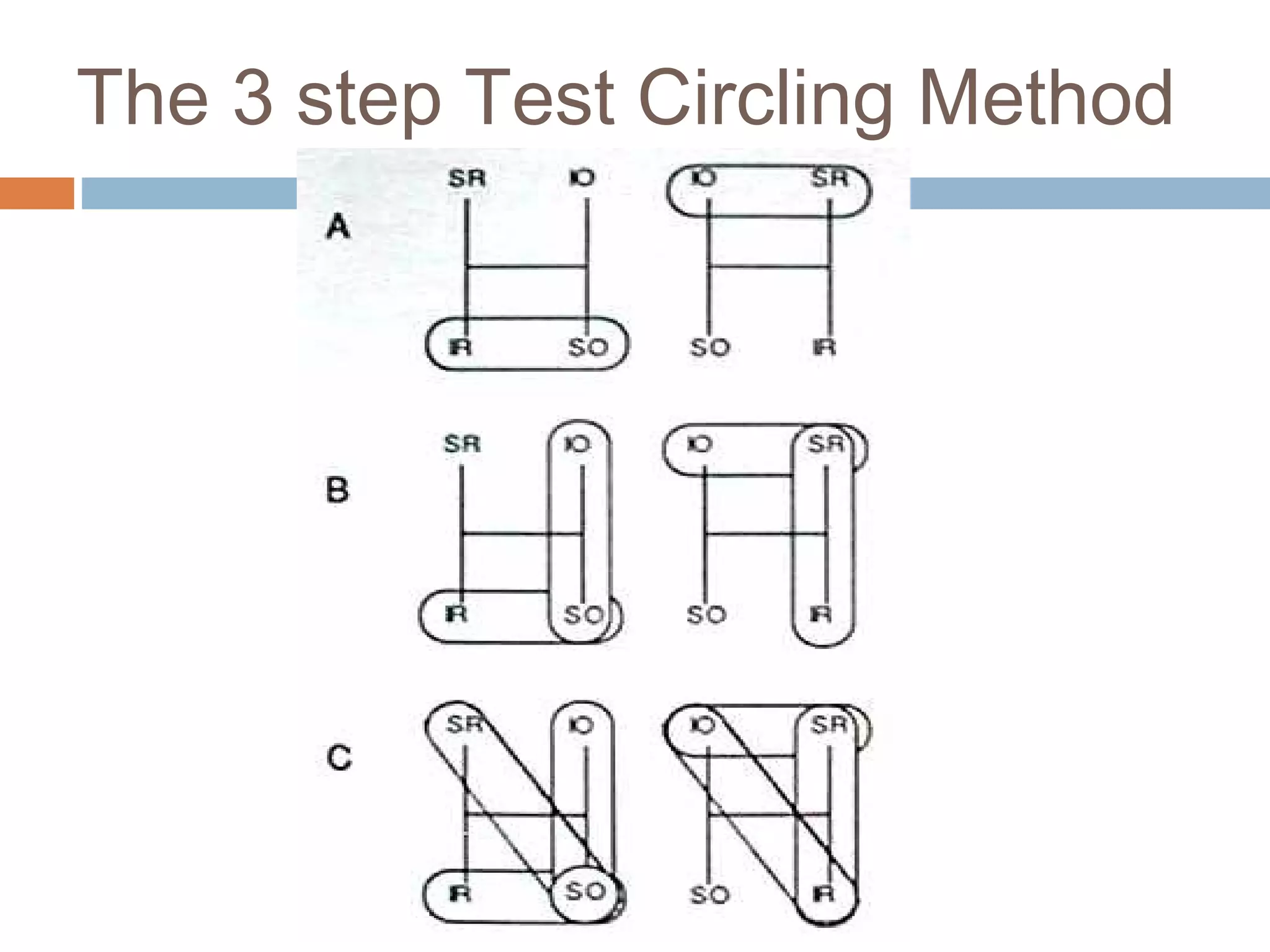
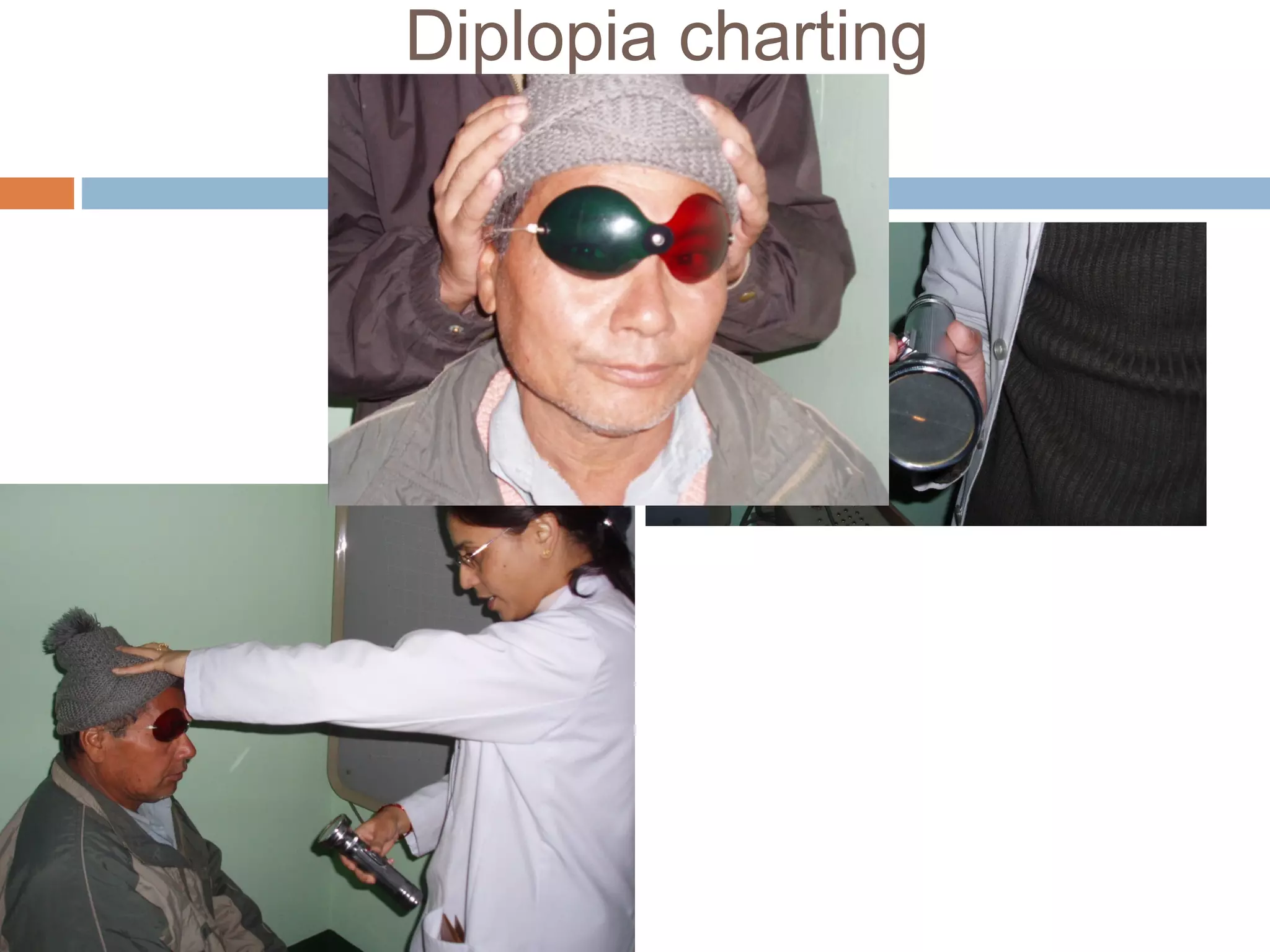
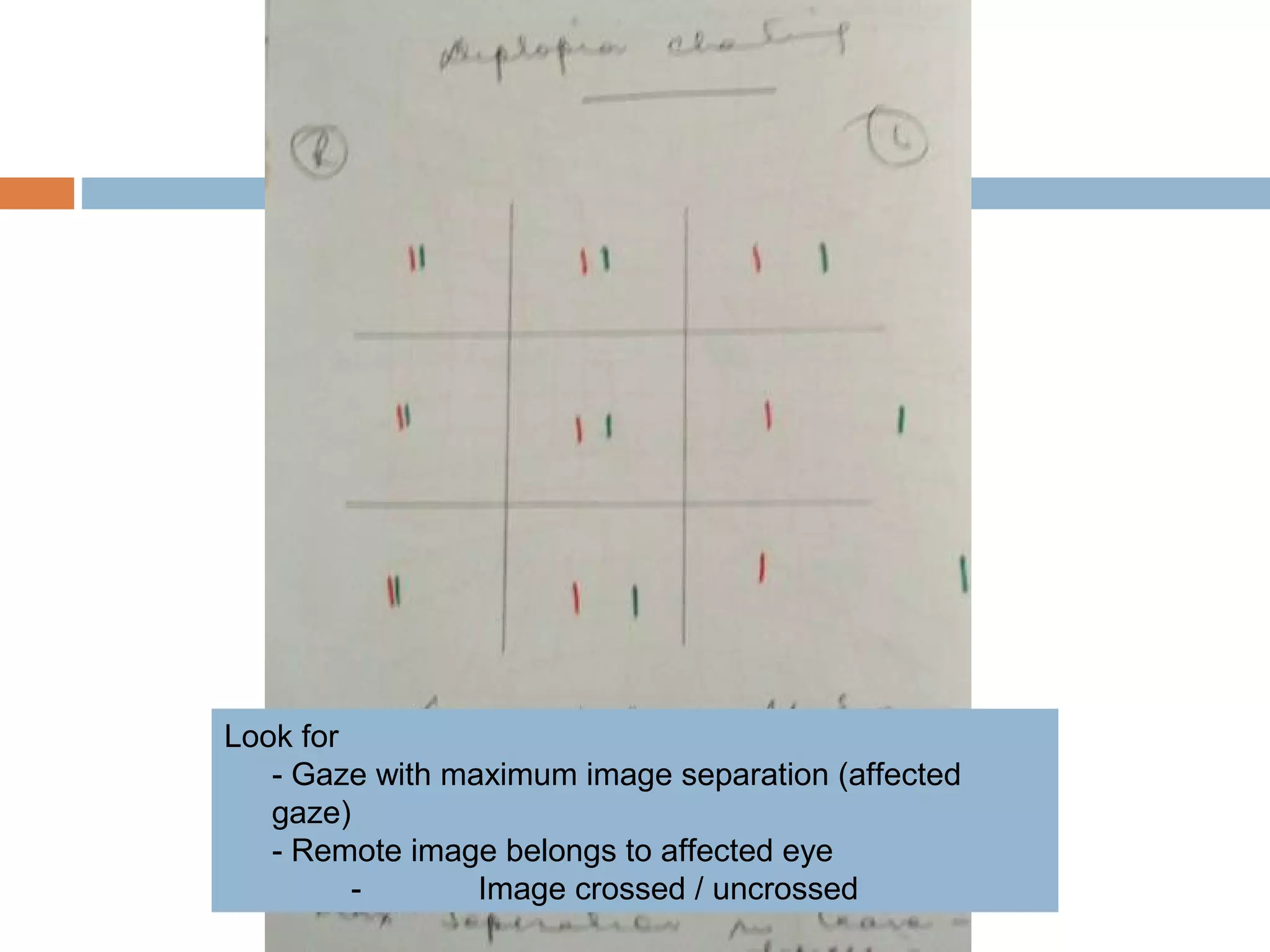
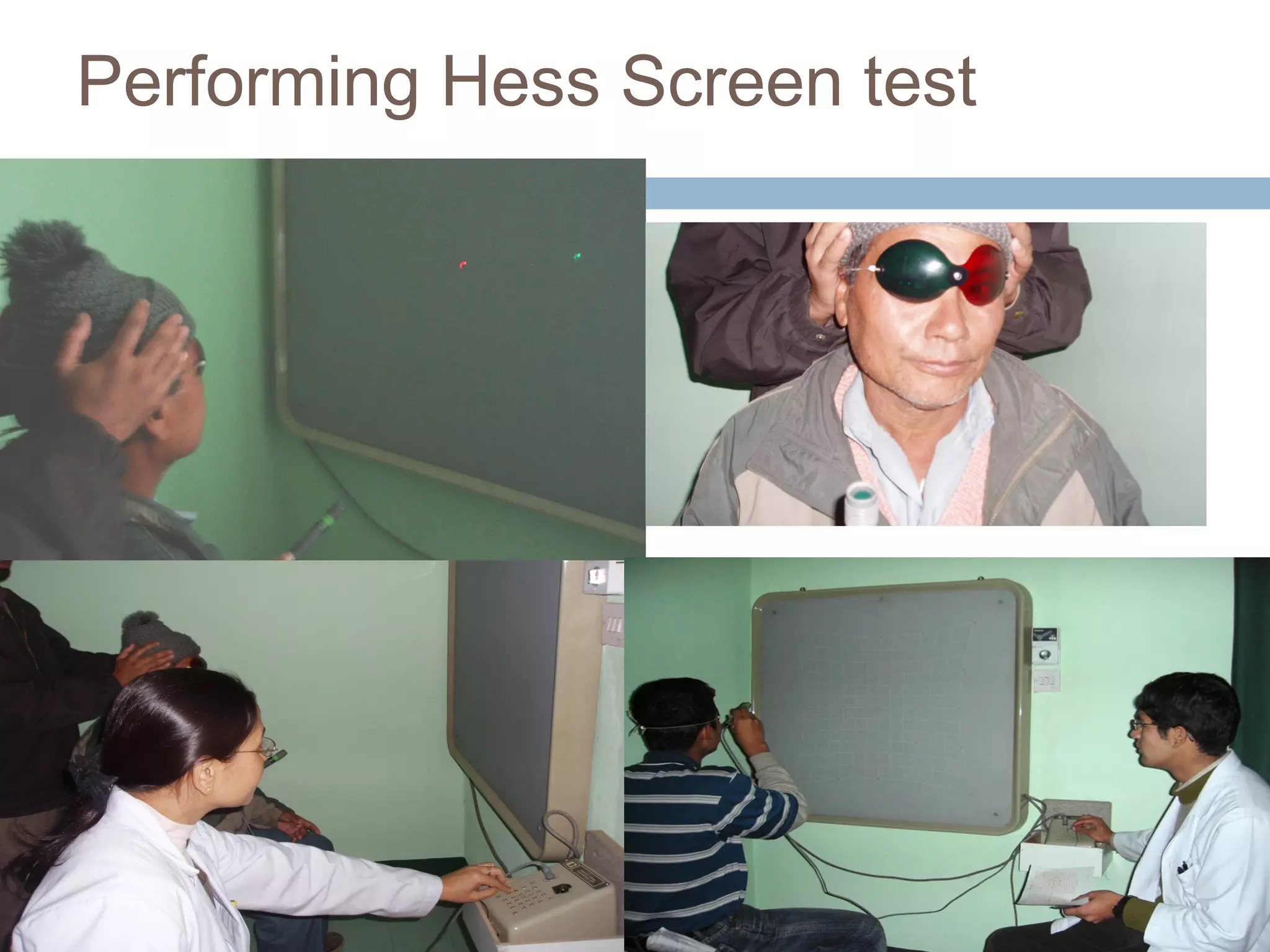
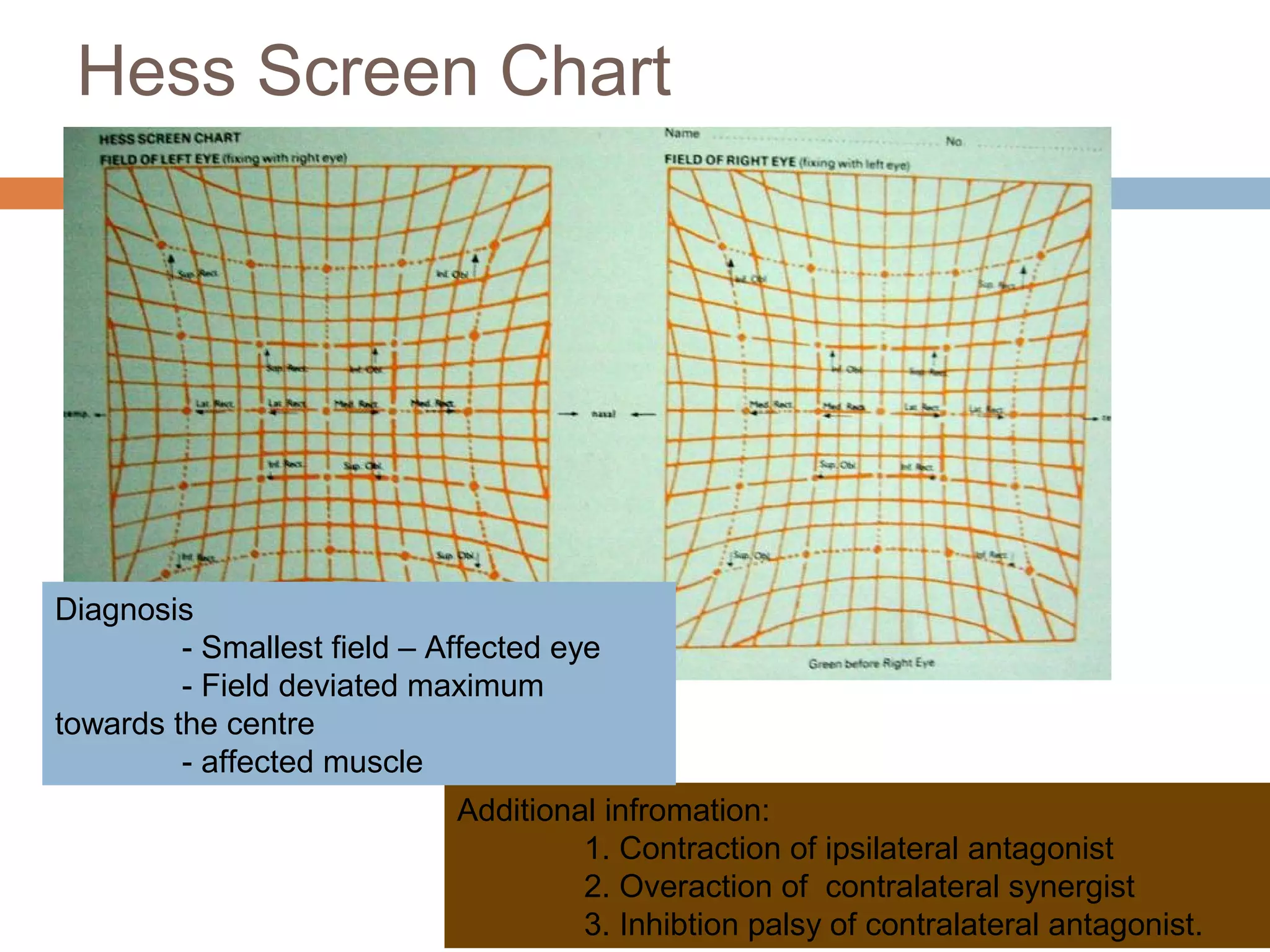
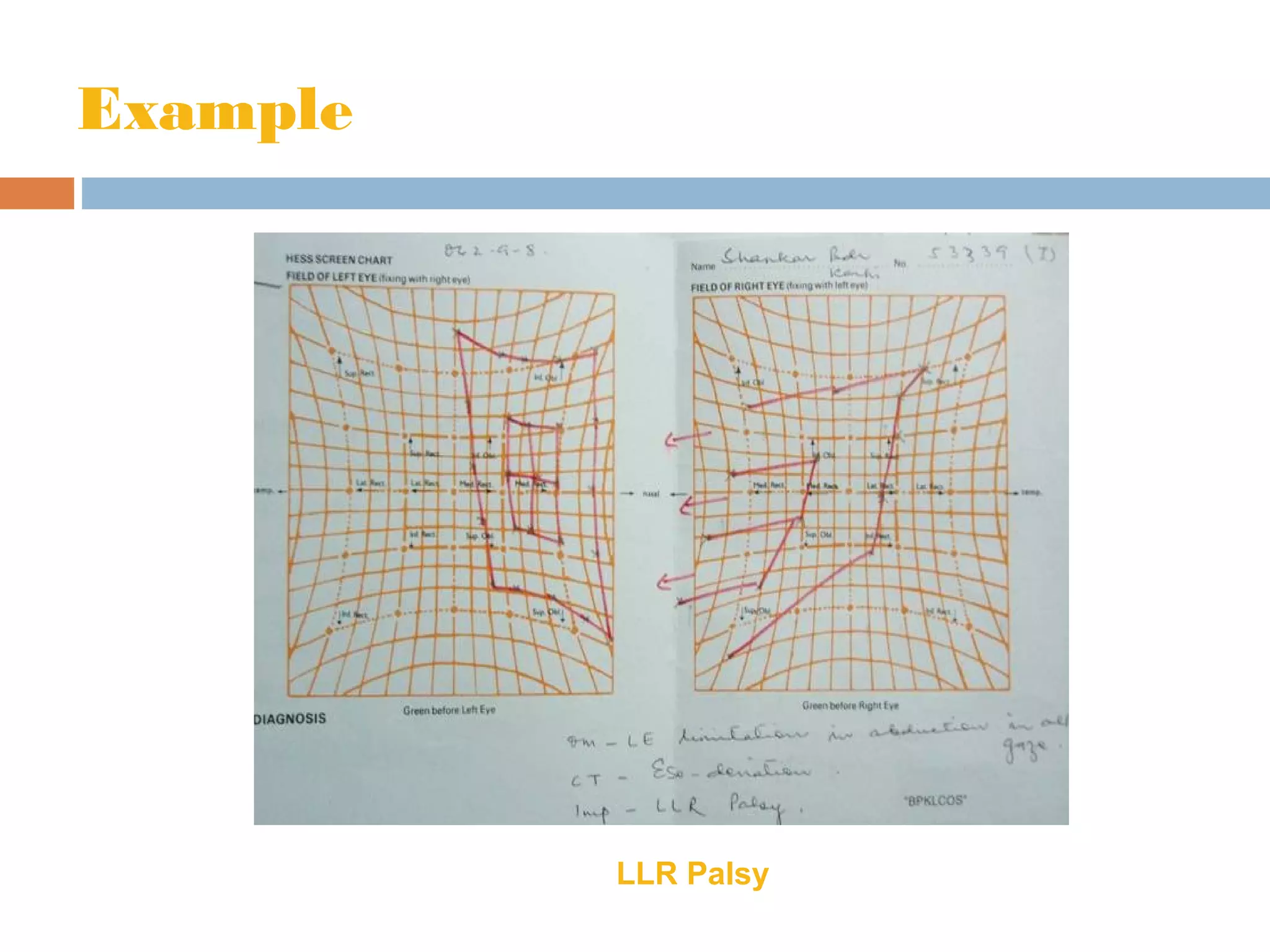
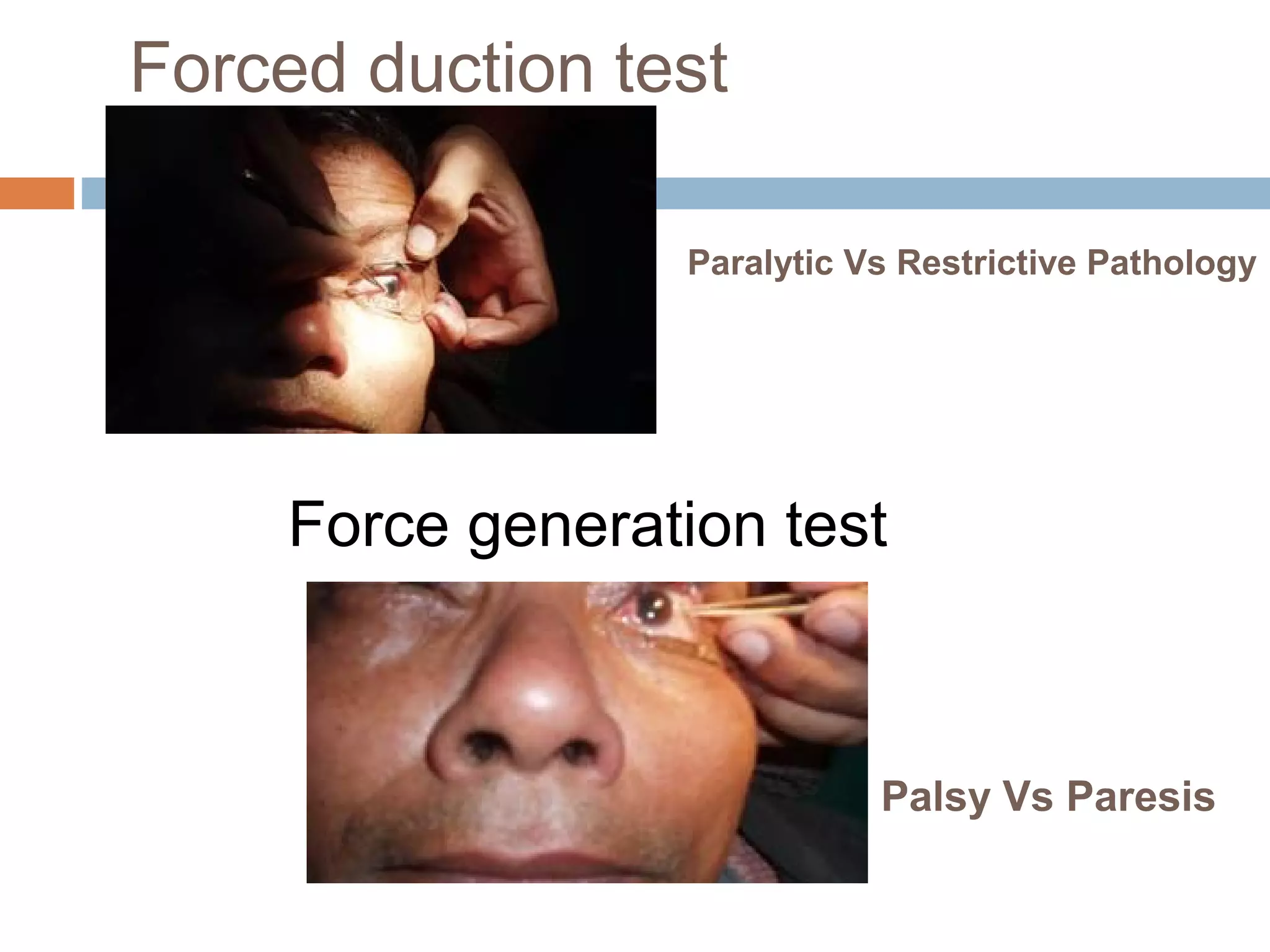
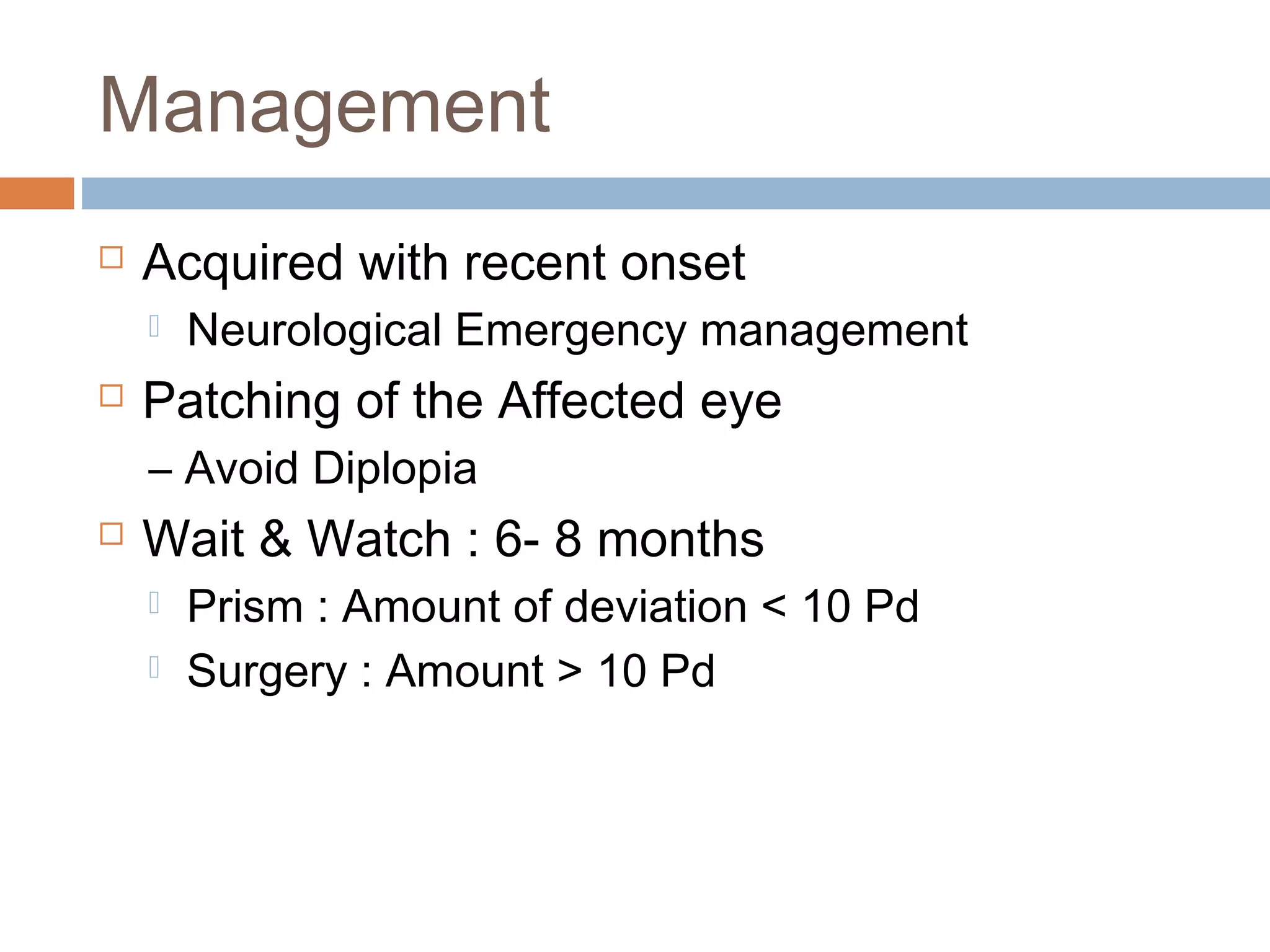
The document provides a comprehensive overview of incomitant strabismus, detailing its types, diagnosis, and management strategies. It categorizes deviations into paralytic and non-paralytic forms and discusses the underlying causes, clinical symptoms, and evaluation techniques including various tests. Management recommendations are provided based on the severity of the condition, with strategies ranging from observation to surgical intervention.