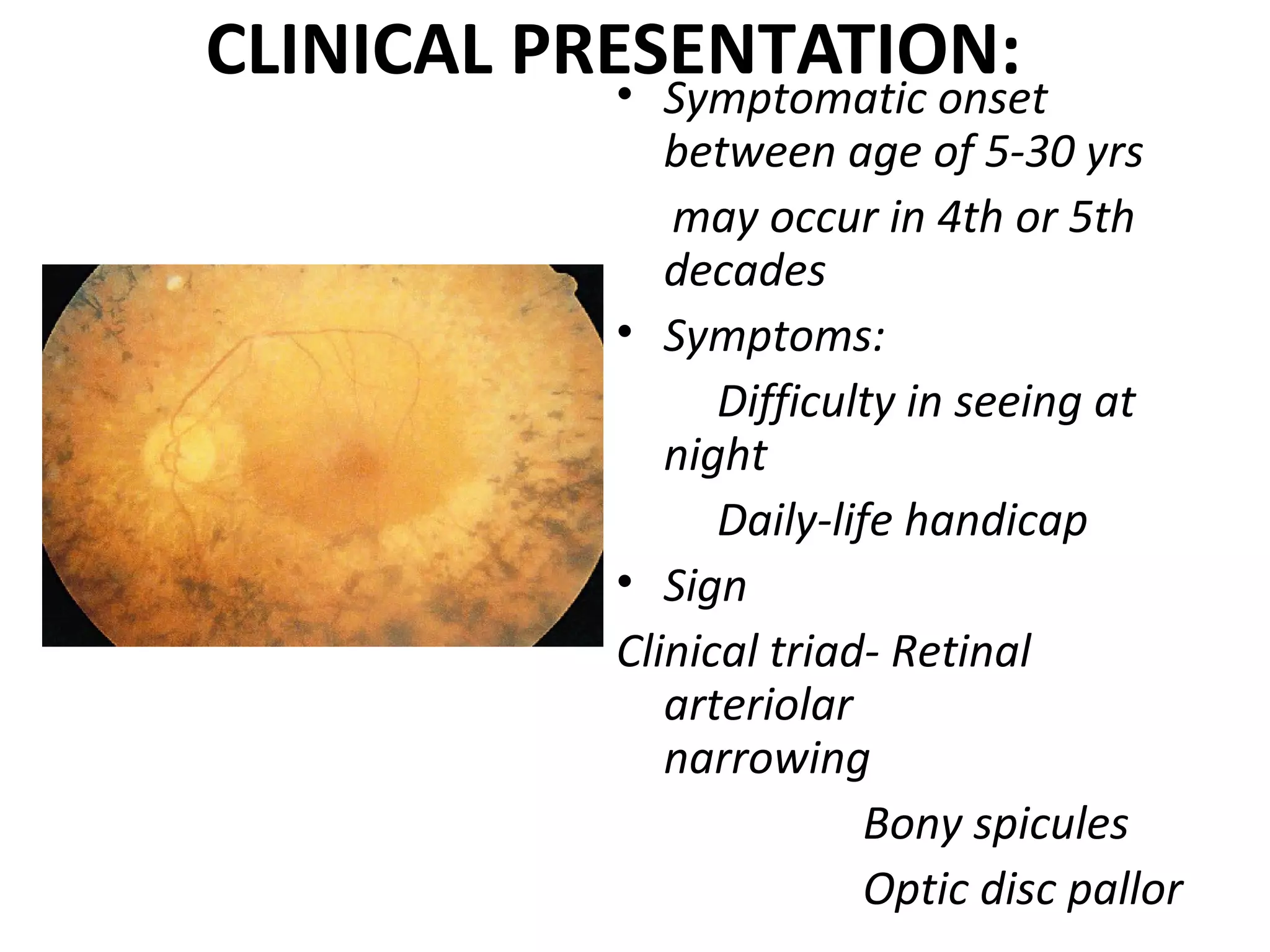
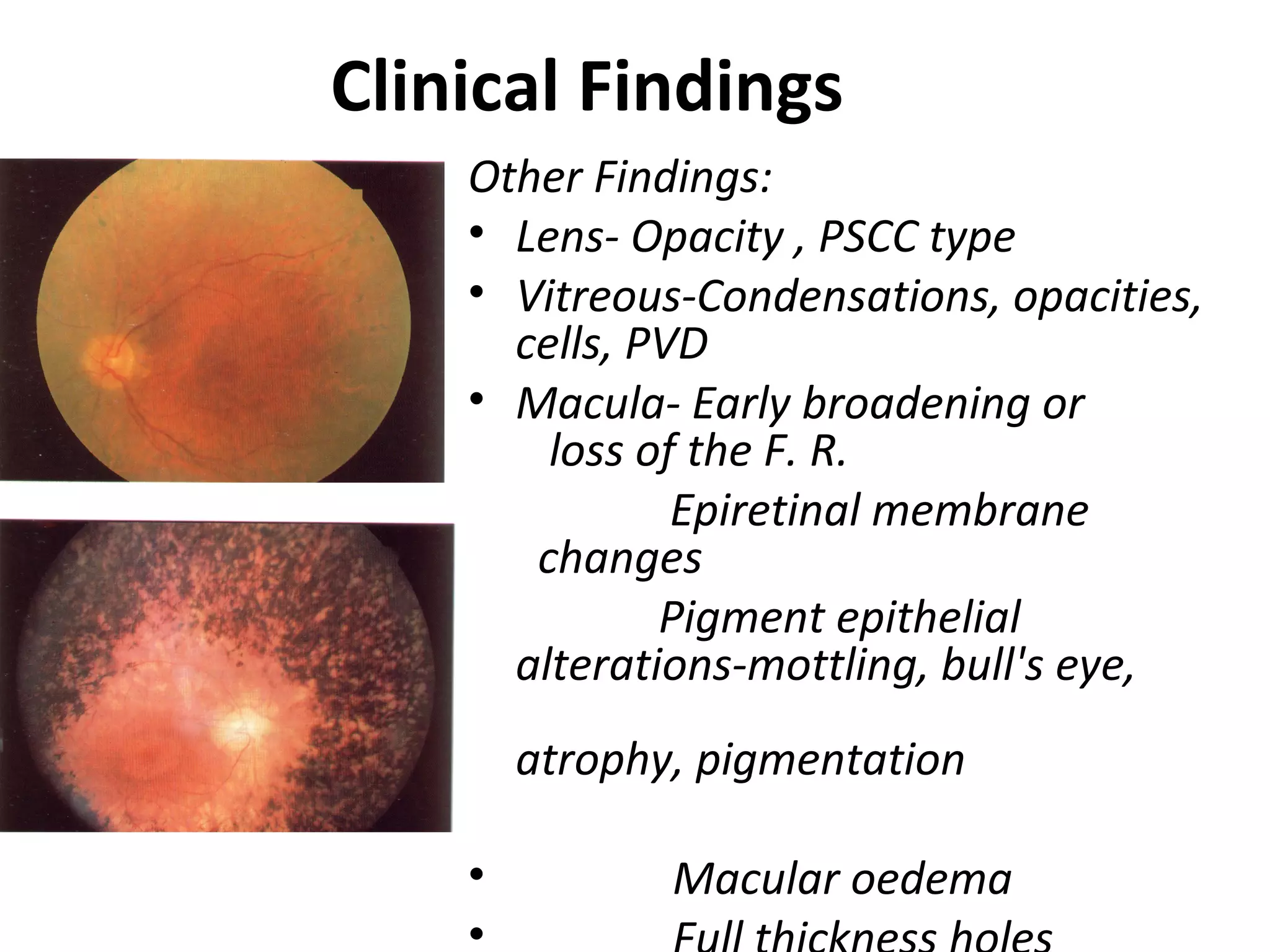
The document discusses night blindness (nyctalopia) and xerophthalmia, emphasizing their definitions, causes, and associations with vitamin A deficiency and various retinal disorders. It highlights specific conditions leading to night blindness, such as retinitis pigmentosa and congenital stationary night blindness, and addresses the prevalence and impact of xerophthalmia as a public health issue in Nepal. The importance of vitamin A in ocular health is stressed, alongside prevention and treatment strategies for deficiencies including dietary interventions and vitamin supplementation.