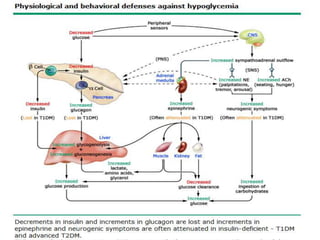
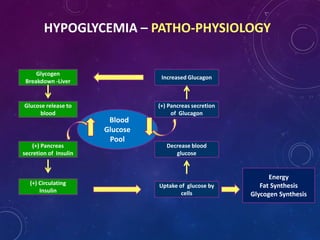
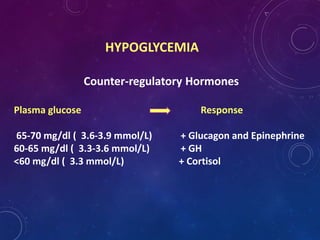
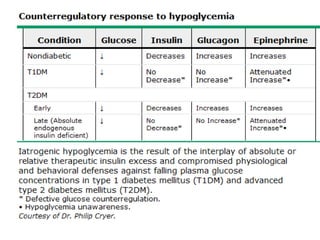
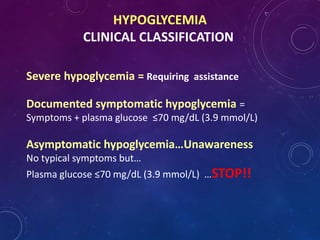
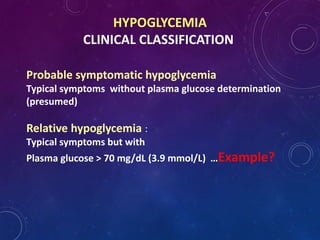
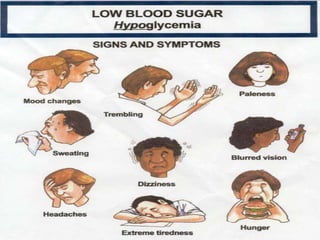
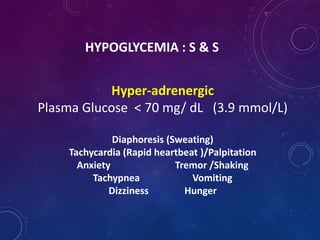
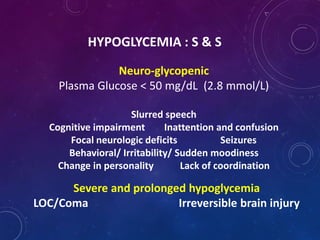
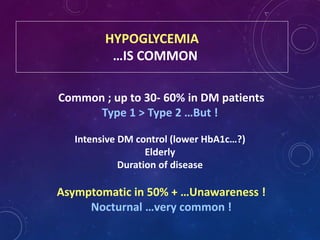
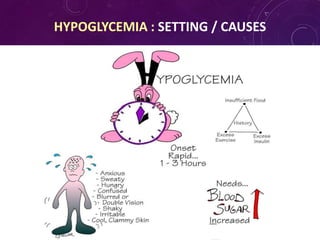
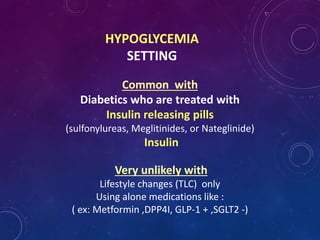
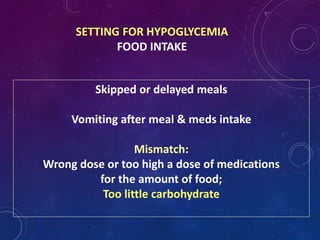
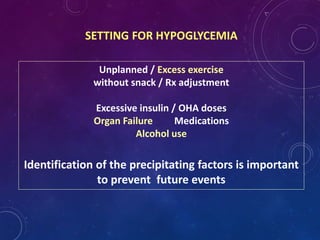
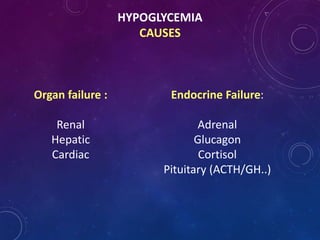
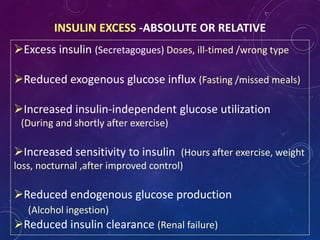
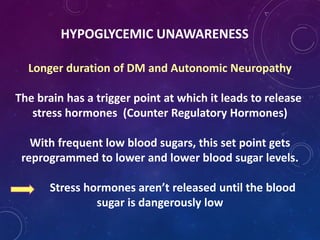
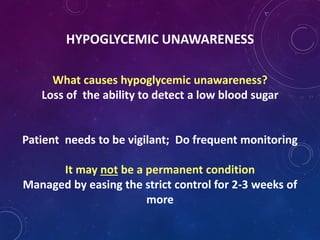
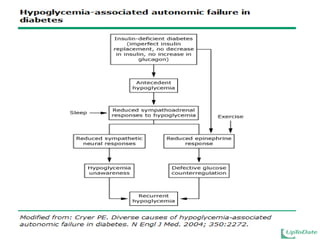
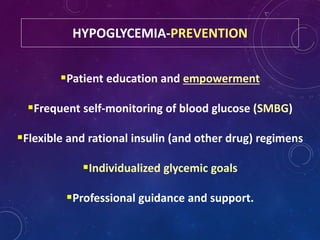
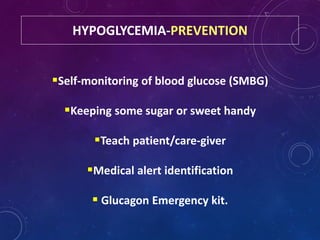
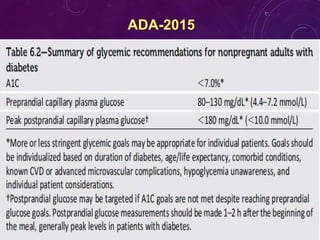
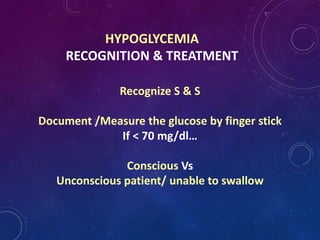
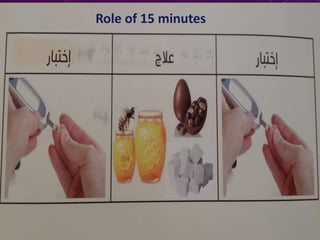
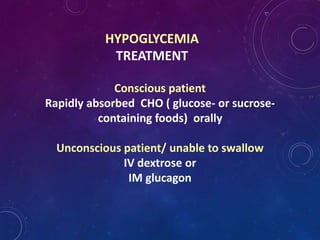
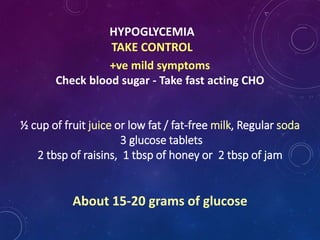
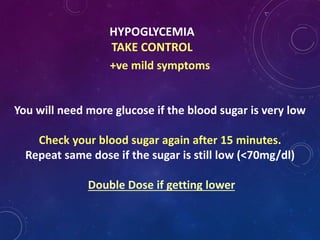
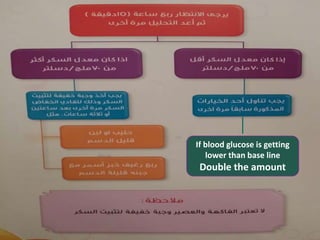
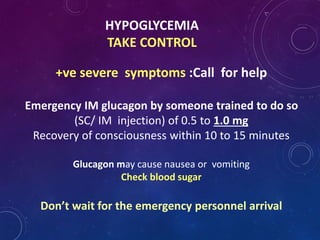
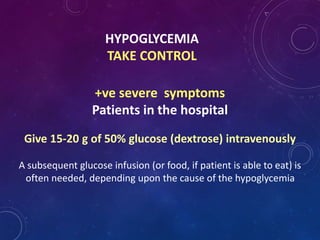
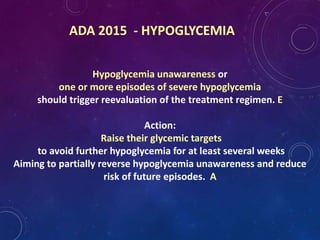
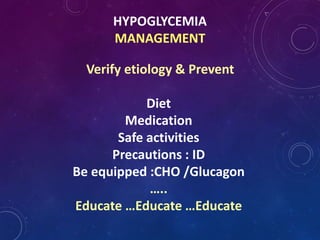
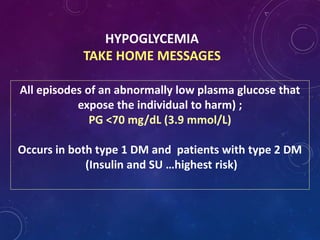
This document provides information about hypoglycemia for diabetes educators. It defines hypoglycemia as a plasma glucose level below 70 mg/dL and describes the physiological response and counter-regulatory hormones involved. Common causes of hypoglycemia are discussed such as insulin excess, missed meals, and hypoglycemic unawareness. The importance of prevention through education and self-monitoring is emphasized. Treatment of mild hypoglycemia involves consuming fast-acting carbohydrates, while glucagon or IV dextrose are recommended for severe hypoglycemia.