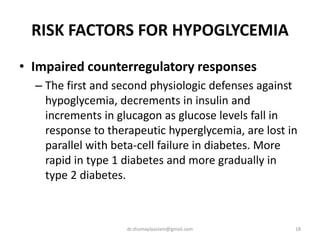
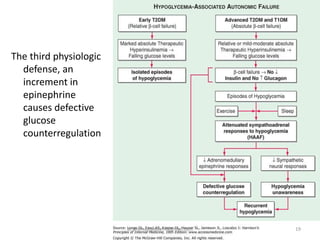
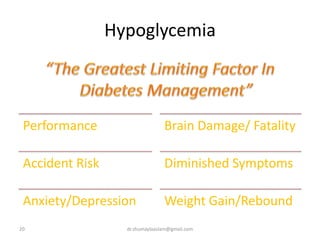
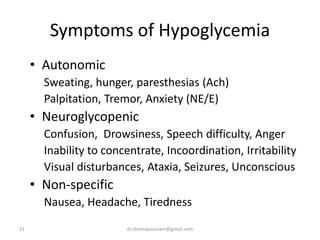
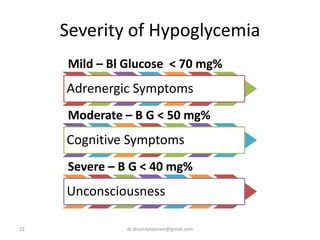
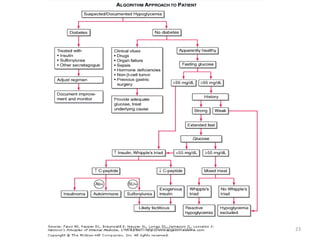
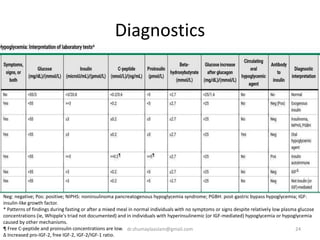
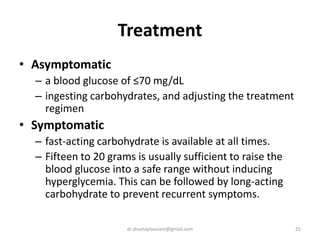
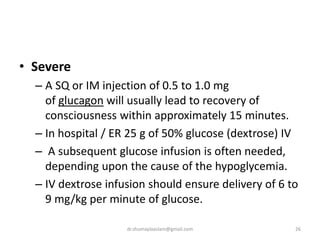
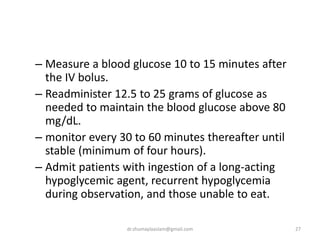
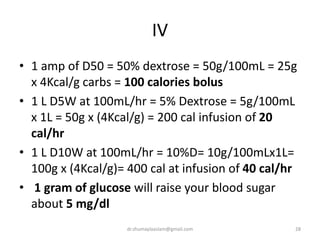
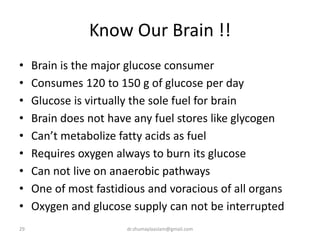
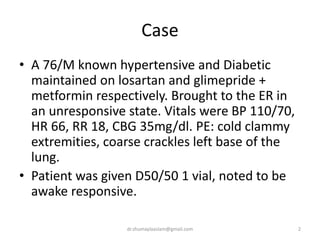
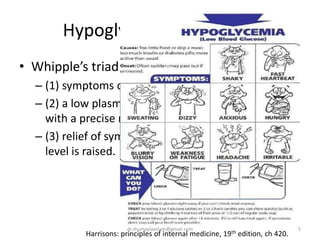
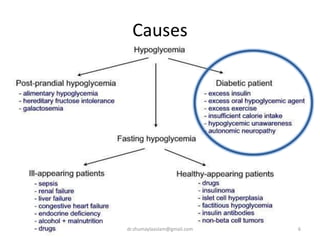
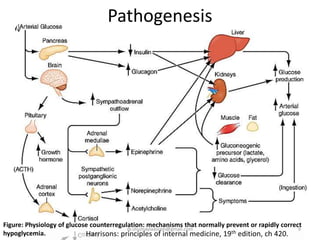
A 76-year old man with diabetes and hypertension was brought to the emergency room in an unresponsive state. His blood sugar was low at 35 mg/dL. He was given dextrose which caused him to become responsive again. Hypoglycemia can be caused by issues with insulin secretion or counterregulation in diabetes. Symptoms range from autonomic to neuroglycopenic. Treatment involves ingestion of fast-acting carbohydrates for mild episodes or intravenous dextrose for more severe cases. Lifestyle changes and medication adjustments are also important to prevent future hypoglycemia.
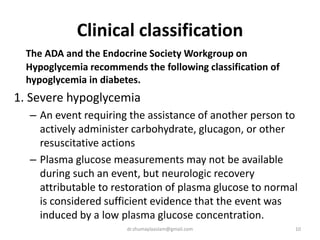
![4. Probable symptomatic hypoglycemia
– typical symptoms of hypoglycemia are not
accompanied by a plasma glucose determination
(glucose concentration ≤70 mg/dL [3.9 mmol/L]).
5. Pseudohypoglycemia
– the person with diabetes reports typical symptoms
of hypoglycemia and interprets those as indicative of
hypoglycemia but with a measured plasma glucose
concentration >70 mg/dL (3.9 mmol/L).
– This category reflects the fact that patients with
chronically poor glycemic control.
12dr.shumaylaaslam@gmail.com](https://image.slidesharecdn.com/hypoglycemia-190302030641/85/Hypoglycemia-in-Adults-12-320.jpg)