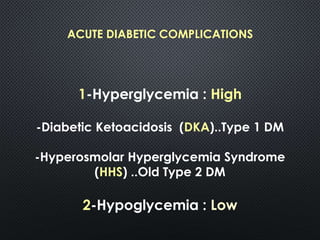
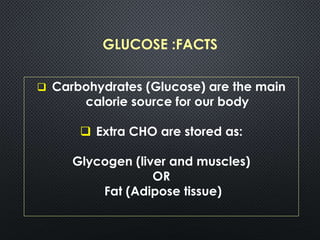
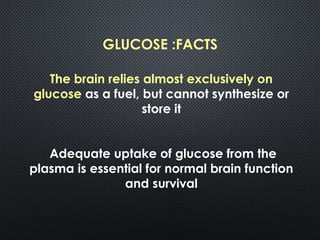
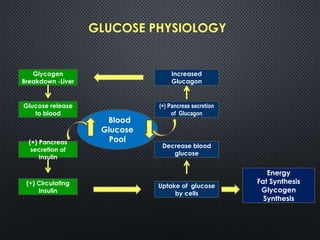
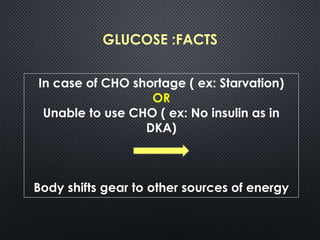
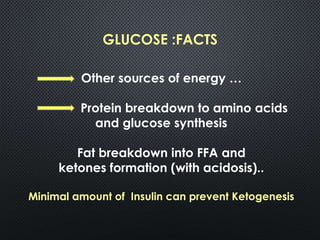
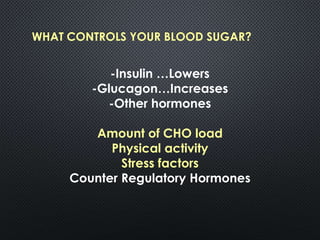
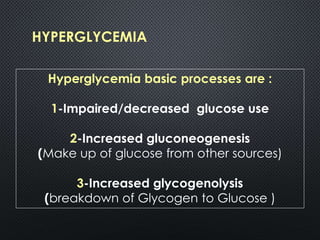
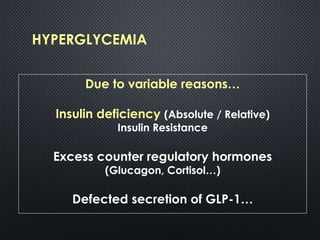
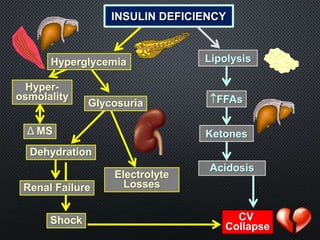
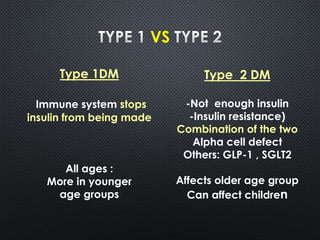
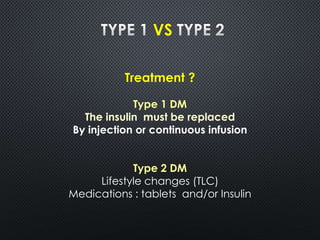
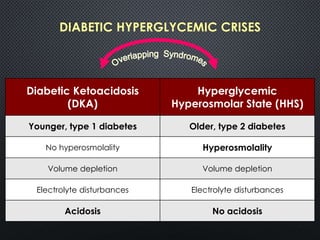
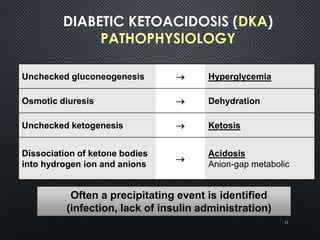
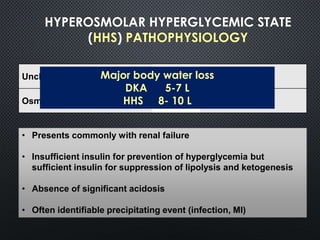
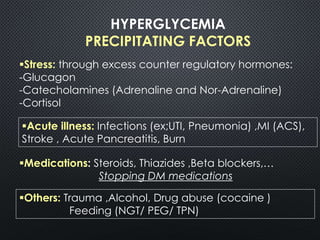
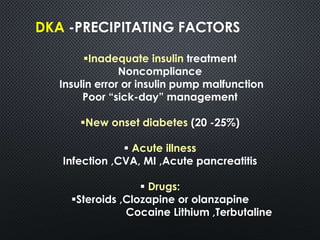
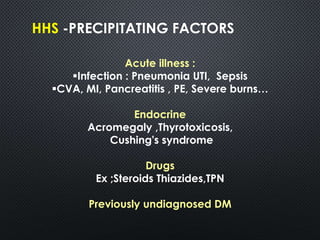
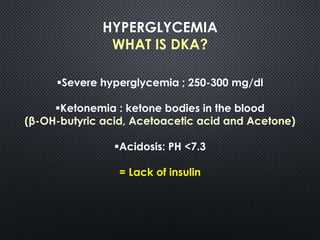
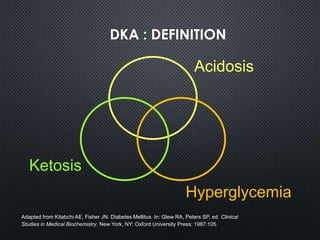
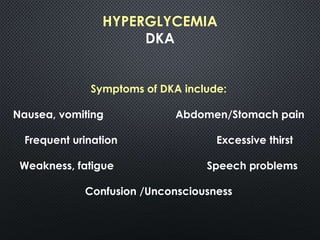
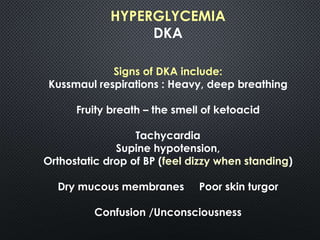
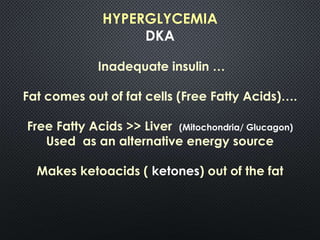
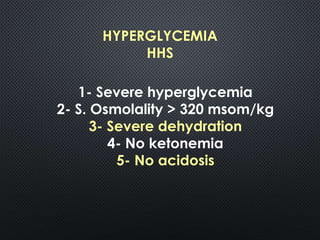
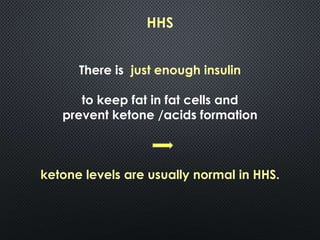
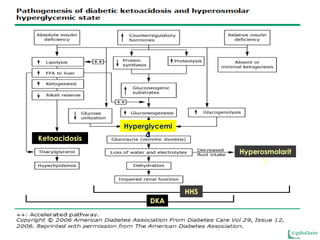
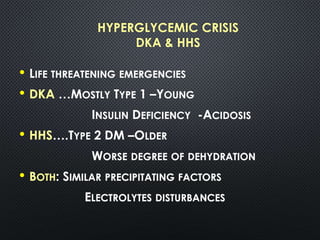
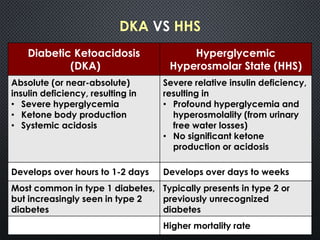
This document provides an overview of diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS), two life-threatening complications of diabetes that result in severe hyperglycemia. It defines DKA and HHS, describes their pathophysiology including the role of insulin deficiency and counterregulatory hormones, and compares their typical presentations and precipitating factors. The key differences between DKA and HHS are noted, with DKA more common in type 1 diabetes and characterized by ketosis and acidosis, while HHS occurs more often in type 2 diabetes and lacks significant ketosis or acidosis. Early aggressive management of both conditions is emphasized through hydration, insulin administration, and electrolyte