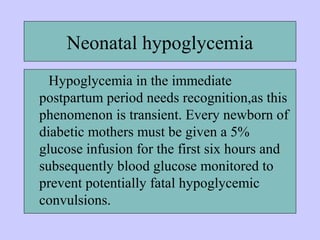
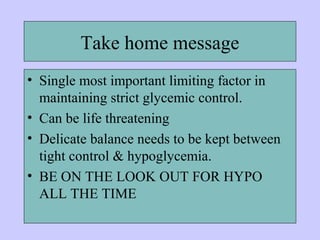
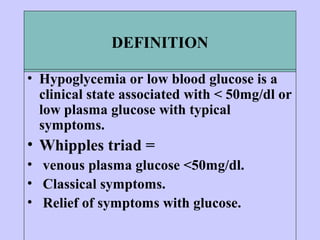
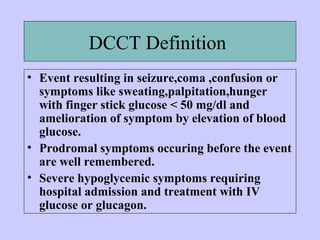
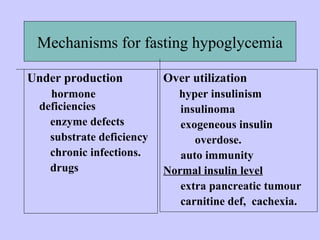
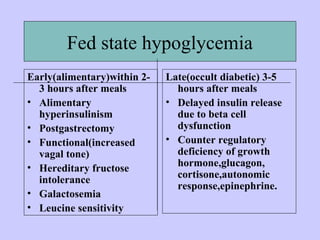
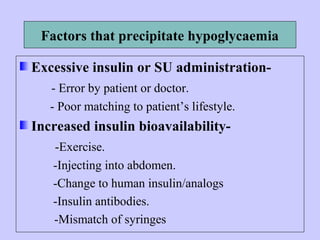
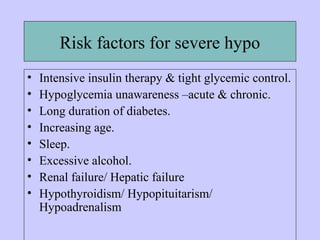
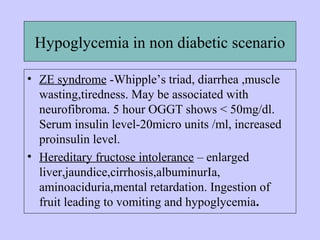
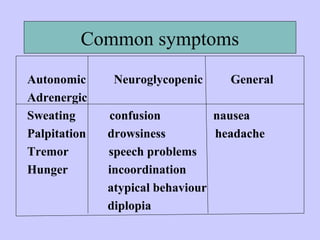
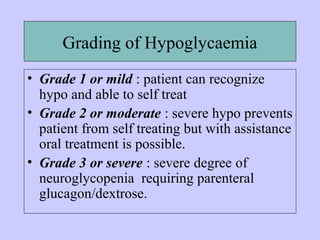
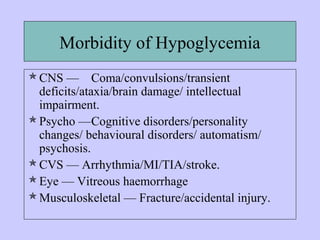
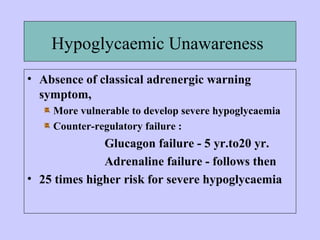
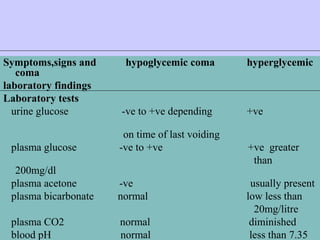
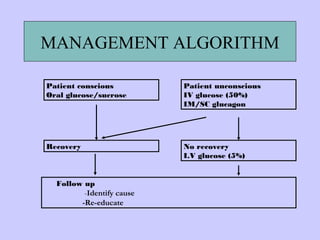
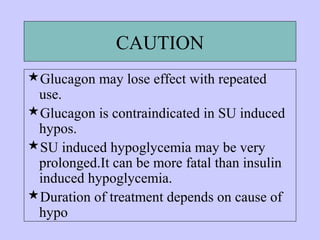
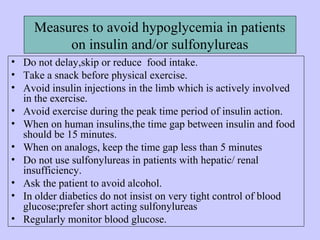
This document defines diabetic hypoglycemia and describes its causes, symptoms, and treatment. Hypoglycemia is low blood glucose below 50mg/dl causing symptoms that are relieved by raising blood glucose. It can be caused by excessive insulin, missed meals, exercise, or drugs interacting with insulin. Symptoms range from autonomic reactions to neuroglycopenic effects like confusion. Treatment involves oral glucose for conscious patients or IV glucose/glucagon for unconscious patients. Strict avoidance and glucose monitoring are needed to prevent hypoglycemia in insulin-treated diabetics.

![Drugs causing hypo
• Increase in SU effect
• Salicylates, probenecid, sulfonamides,
nicoumalone, fluconazole [inhibits CYP2C9 which
metabolizes glimepiride], ketoconazole,
ciprofloxacin [inhibits CYP3A4 which
metabolizes glibenclamide], gatifloxacin
• Direct hypoglycemic effect
• ACE(I), disopyramide, SSRIs, quinine,
sulfamethoxazole, mefloquine, pentamidine,
doxycycline, ethanol](https://image.slidesharecdn.com/diabeticcomaclinicalfeatures1-180111115406/85/Diabetic-coma-clinical_features-27-320.jpg)