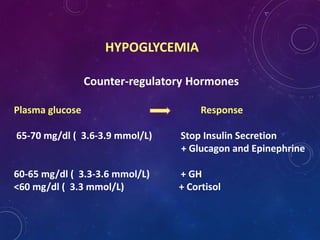
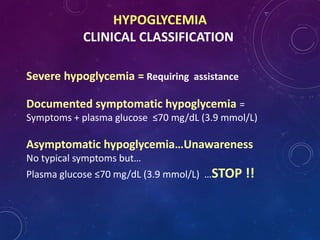
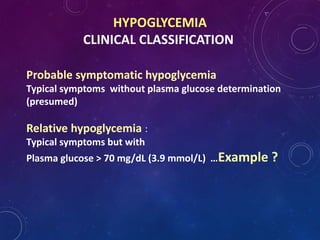
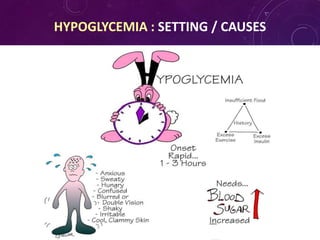
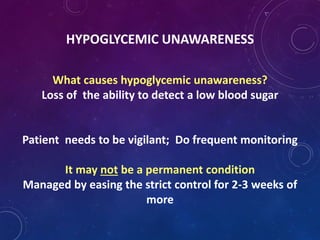
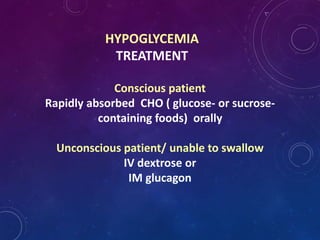
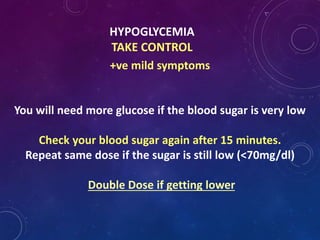
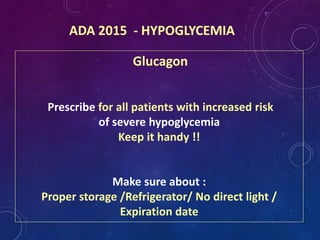
This document provides information about hypoglycemia for diabetes educators. It defines hypoglycemia as a blood glucose level below 70 mg/dL and describes the physiological response and counter-regulatory hormones involved. Symptoms of hypoglycemia are outlined as either hyperadrenergic or neuroglycopenic depending on blood glucose level. Causes of hypoglycemia include insulin excess, reduced food intake, exercise, and organ dysfunction. Management involves prevention through education, recognition and treatment of low blood sugar with fast-acting carbohydrates, and addressing the underlying cause to prevent future episodes.