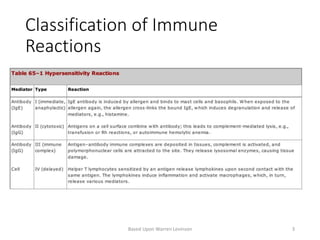
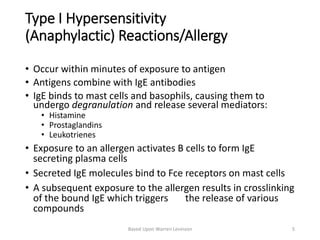
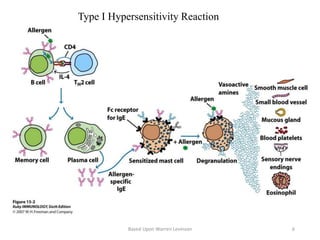
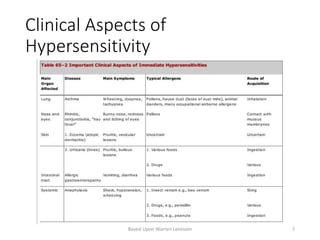
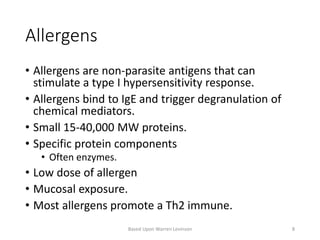
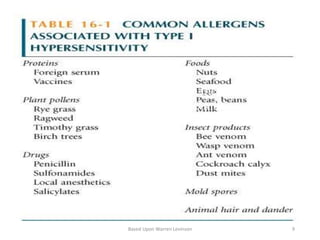
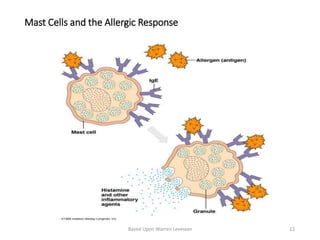
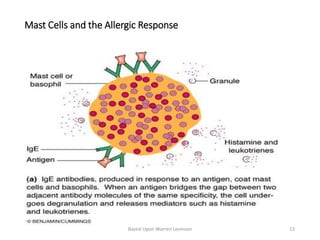
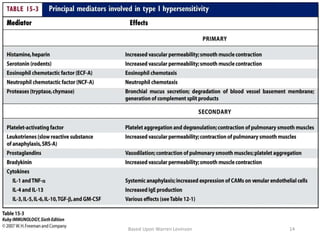
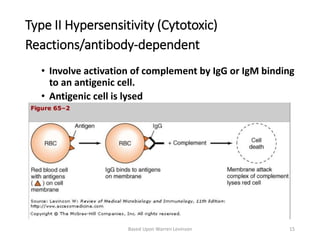
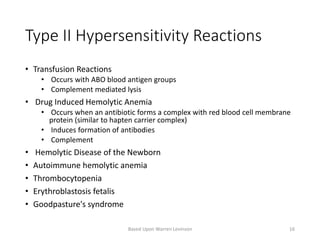
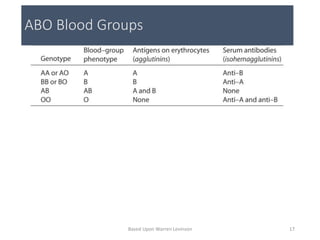
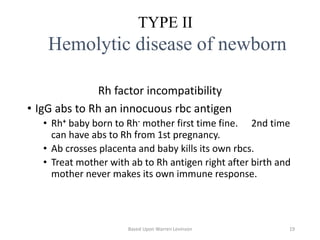
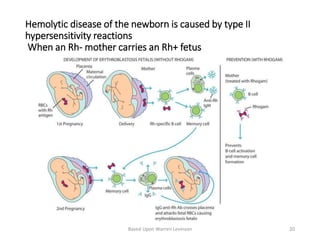
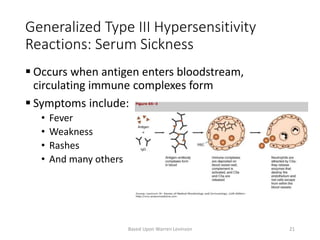
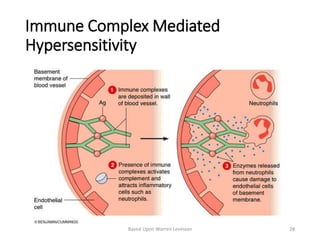
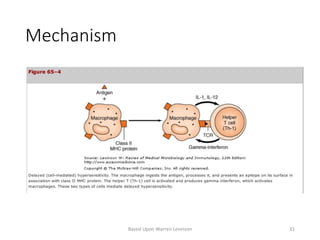
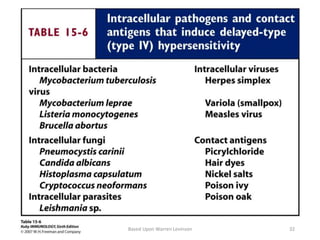
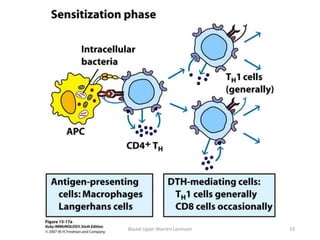
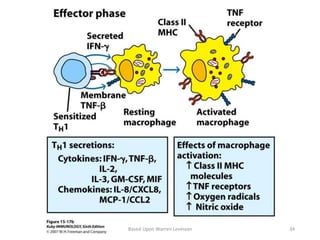
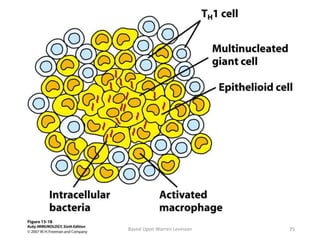
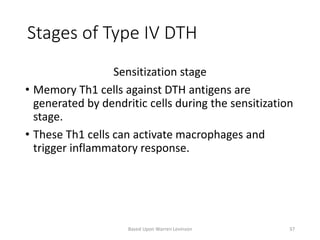
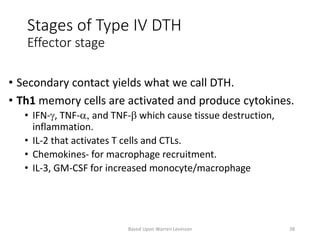
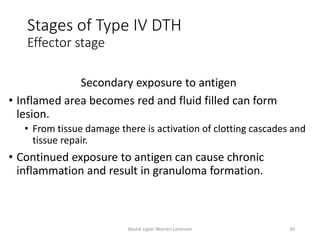
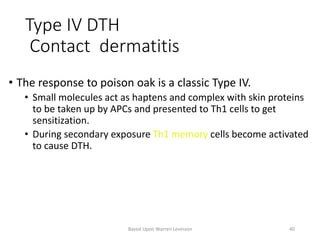
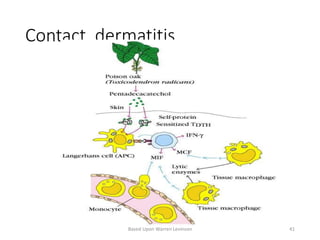
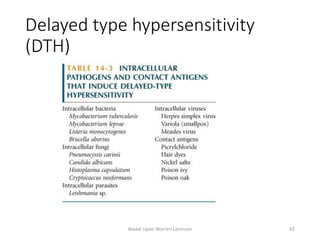
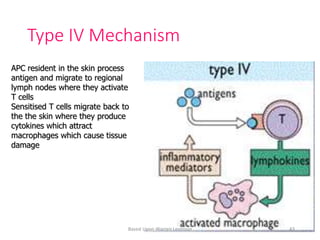
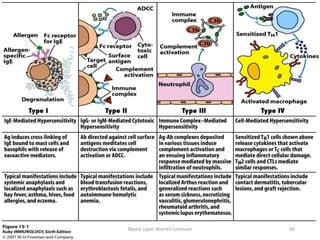
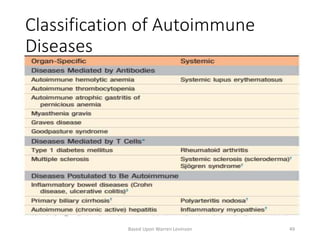
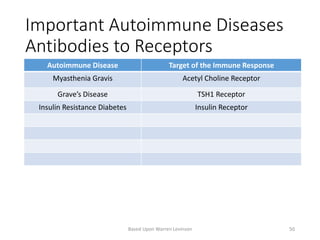
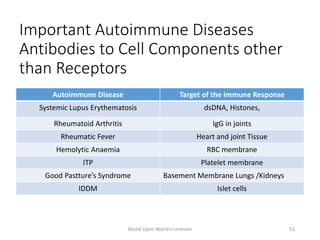
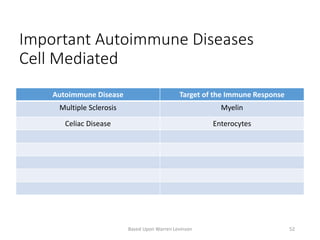
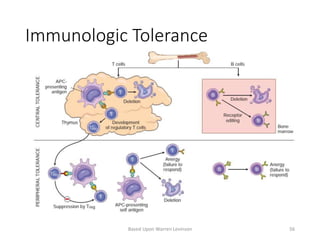
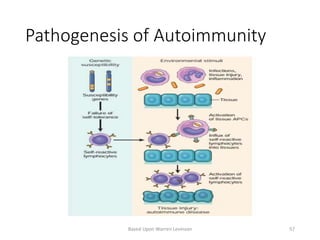
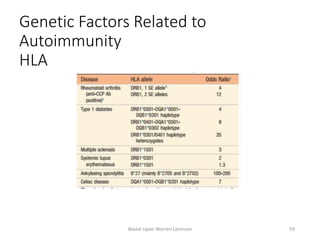
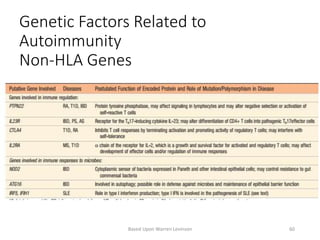
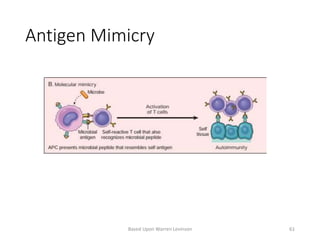
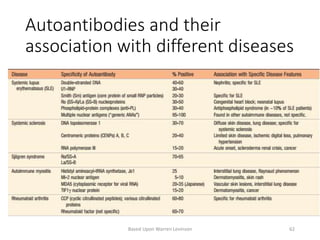
This document discusses different types of hypersensitivity reactions and autoimmune diseases. It covers four types of hypersensitivity reactions: type I involves IgE antibodies and mast cells/basophils; type II involves IgG/IgM antibodies activating complement and lysing cells; type III involves immune complex formation and deposition; type IV involves delayed T cell responses. Examples and mechanisms of each type are provided. The document also discusses tolerance, genetic and environmental factors in autoimmunity, common autoimmune diseases and the antibodies associated with them.