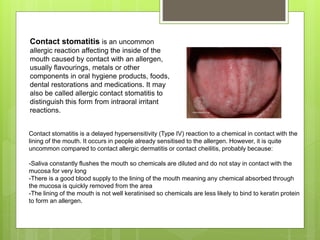
This document discusses the different types of hypersensitivity reactions as classified by Gell and Coombs. It provides details on type I (immediate), type II (antibody-mediated), type III (immune complex-mediated), and type IV (delayed) hypersensitivity reactions, including the antibodies or cells involved, examples of diseases, and a brief description of the immunological reaction for each type. It also discusses contact stomatitis as an uncommon allergic reaction affecting the inside of the mouth.



![Type I hypersensitivity (or immediate hypersensitivity), in the Gell and
Coombs classification of allergic reactions, is an allergic reaction
provoked by re-exposure to a specific type of antigen referred to as an
allergen.[1] Type I is distinct from type II, type III and type IV
hypersensitivities.
1. med/1101 at eMedicine
2. Descotes, Jacques; Choquet-Kastylevsky, Geneviève (February 2001). "Gell and Coombs's classification: is it still valid?". Toxicology. 158 (1–2):
43–49. doi:10.1016/S0300-483X(00)00400-5. PMID 11164991.
The relevance of the Gell and Coombs classification of allergic reactions
has been questioned in the modern-day understanding of allergy, and it
has limited utility in clinical practice.[2]
Exposure may be by ingestion, inhalation, injection, or direct contact.](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-5-320.jpg)
![In type I hypersensitivity, B cells are stimulated (by CD4+ Th2 cells) to produce IgE
antibodies specific to an antigen. The difference between a normal infectious
immune response and a type 1 hypersensitivity response is that in type 1
hypersensitivity, the antibody is IgE instead of IgA, IgG, or IgM. During sensitization,
the IgE antibodies bind to FcεRI receptors on the surface of tissue mast cells and
blood basophils.[4]
Mast cells and basophils coated by IgE antibodies are "sensitized". Later exposure
to the same allergen cross-links the bound IgE on sensitized cells, resulting in
anaphylactic degranulation, which is the immediate and explosive release of
pharmacologically active pre-formed mediators from storage granules and
concurrent synthesis of inflammatory lipid mediators from arachidonic acid;[5]
some of these mediators include histamine, leukotriene (LTC4 and LTD4 and
LTB4), and prostaglandin, which act on proteins (e.g., G-protein coupled receptors)
located on surrounding tissues.[5] The principal effects of these products are
vasodilation and smooth-muscle contraction.
"The Adaptive Immune System: Type I Immediate Hypersensitivity". Archived from the original on 2010-07-27. Retrieved 2008-09-22.](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-6-320.jpg)
![TYPE I HYPERSENSITIVITY
ALTERNATE NAMES:
Allergy
Immediate
Anaphylactic
ANTIBODIES OR CELL MEDIATOR: IgE
IMMUNOLOGIC REACTION:
Fast response which occurs in minutes, rather than multiple hours or days.
Free antigens cross link the IgE on mast cells and basophils which causes
a release of vasoactive biomolecules. Testing can be done via skin test for
specific IgE.[5]
EXAMPLES: Atopy, Anaphylaxis, Asthma, Churg–Strauss Syndrome
5. Black, C. A. (1999). "Delayed type hypersensitivity: Current theories with an historic perspective". Dermatology Online Journal. 5 (1):
7. doi:10.5070/D32FW0G1XX. PMID 10673450.](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-7-320.jpg)

![The pathophysiology of type II hypersensitivity reactions can be broadly
classified into three types:
Cell depletion or destruction without inflammation
Inflammation mediated by complement or Fc receptor
Cellular dysfunction by antibodies
The process involves a series of immune-mediated events that might take
different forms.[12]](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-9-320.jpg)
![TYPE II HYPERSENSITIVITY
ALTERNATE NAMES:
Antibody- dependent
ANTIBODIES OR CELL MEDIATOR: Antibody IgM, Antibody IgG,
Complement, MAC
IMMUNOLOGIC REACTION:
Antibody (IgM or IgG) binds to antigen on a target cell, which is actually a
host cell that is perceived by the immune system as foreign, leading to
cellular destruction via the MAC. Testing includes both the direct and indirect
Coombs test.[6]
EXAMPLES:Autoimmune hemolytic anemia, Rheumatic heart disease,
Thrombocytopenia, Erythroblastosis fetalis, Goodpasture's syndrome
Graves' disease, Myasthenia gravis, Pemphigus vulgaris
6. Delayed Hypersensitivity Reactions at eMedicine](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-10-320.jpg)
![In type III hypersensitivity reaction, an abnormal immune response is mediated by the
formation of antigen-antibody aggregates called "immune complexes". They can
precipitate in various tissues such as skin, joints, vessels, or glomeruli, and trigger the
classical complement pathway. Complement activation leads to the recruitment of
inflammatory cells (monocytes and neutrophils) that release lysosomal enzymes and
free radicals at the site of immune complexes, causing tissue damage.[citation needed]
2. Usman, Norina; Annamaraju, Pavan (2021), "Type III Hypersensitivity Reaction", StatPearls, Treasure Island (FL): StatPearls
Publishing, PMID 32644548, retrieved 2021-07-05 This article incorporates text available under the CC BY 4.0 license.
The most common diseases involving a type III hypersensitivity reaction are serum
sickness, post-streptococcal glomerulonephritis, systemic lupus erythematosus,
farmers' lung (hypersensitivity pneumonitis), and rheumatoid arthritis.[citation needed]
The principal feature that separates type III reactions from other hypersensitivity
reactions is that in type III reaction, the antigen-antibody complexes are pre-formed in
the circulation before their deposition in tissues.[2]](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-11-320.jpg)
![TYPE III HYPERSENSITIVITY
ALTERNATE NAMES:
Immune complex
ANTIBODIES OR CELL MEDIATOR:Antibody IgG, Complement.
Neutrophils
IMMUNOLOGIC REACTION:
Antibody (IgG) binds to soluble antigen, forming a circulating immune
complex. This is often deposited in the vessel walls of the joints and kidney,
initiating a local inflammatory reaction.[7]
EXAMPLES: Serum sickness, Rheumatoid arthritis, Arthus reaction,
Post streptococcal glomerulonephritis, Membranous nephropathy
Reactive arthritis, Lupus nephritis, Systemic lupus erythematosus,
Extrinsic allergic alveolitis (hypersensitivity pneumonitis)
7. Kumar, Vinay; Abbas, Abul K.; Aster, Jon C., eds. (2014). "Hypersensitivity: Immunologicaly Mediated Tissue Injury". Robbins & Cotran
Pathologic Basis of Disease (9th ed.). Elsevier Health Sciences. pp. 200–11. ISBN 978-0-323-29635-9.](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-12-320.jpg)
![A Type IV hypersensitivity reaction is mediated by T cells that provoke an inflammatory reaction
against exogenous or endogenous antigens. In certain situations, other cells, such as monocytes,
eosinophils, and neutrophils, can be involved. After antigen exposure, an initial local immune and
inflammatory response occurs that attracts leukocytes. The antigen engulfed by the macrophages
and monocytes is presented to T cells, which then becomes sensitized and activated. These cells
then release cytokines and chemokines, which can cause tissue damage and may result in
illnesses.[citation needed]
Examples of illnesses resulting from type IV hypersensitivity reactions include contact dermatitis
and drug hypersensitivity. Type IV reactions are further subdivided into type IVa, IVb, IVc, and IVd
based on the type of T cell (Th1, Th17 and CTLs) involved and the cytokines/chemokines
produced.[citation needed]
Delayed hypersensitivity plays a crucial role in our body's ability to fight various intracellular
pathogens such as mycobacteria and fungi. They also play a principal role in tumor immunity and
transplant rejection. Since patients with acquired immunodeficiency syndrome (AIDS) have a
progressive decline in the number of CD4 cells, they also have a defective type four hypersensitivity
reaction.[3]](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-14-320.jpg)
![TYPE IV HYPERSENSITIVITY
ALTERNATE NAMES:
Delayed,[5][6], cell-mediated immune memory response,
Antibody-independent, Cytotoxic
ANTIBODIES OR CELL MEDIATOR: T-cells
IMMUNOLOGIC REACTION:
CTL's and T helper cells (specifically Th1 and Th17 cells)[8] are activated by an antigen
presenting cell. When the antigen is presented again in the future, the memory Th1
cells will activate macrophages and cause an inflammatory response. This ultimately
can lead to tissue damage.[9]
EXAMPLES: Contact dermatitis, including Urushiol-induced contact, dermatitis (poison
ivy rash), Mantoux test, Chronic transplant rejection,
Multiple sclerosis[10], Coeliac disease, Hashimoto's thyroiditis,
Granuloma annulare
8. Abbas, Abul K. (6 May 2021). Cellular and Molecular Immunology. Elsevier. p. 444. ISBN 978-0-323-75748-5.
9. Le, Tau. First Aid for the USMLE Step 1 2013, p. 203-204](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-15-320.jpg)





![TREATMENT
Immediate hypersensitivity reactions
The treatment of immediate hypersensitivity reactions includes the management of anaphylaxis
with intramuscular adrenaline (epinephrine), oxygen, intravenous (IV) antihistamine, support blood
pressure with IV fluids, avoid latex gloves and equipment in patients who are allergic, and surgical
procedures such as tracheotomy if there is severe laryngeal edema.
Allergic bronchial asthma can be treated with any of the following: inhaled short- and long-acting
bronchodilators (anticholinergics) along with inhaled corticosteroids, leukotriene antagonists, use of
disodium cromoglycate, and environmental control. Experimentally, a low dose of methotrexate or
cyclosporin and omalizumab (a monoclonal anti-IgE antibody) has been used.
Treatment of autoimmune disorders (e.g., SLE) include one or a combination of NSAIDs and
hydroxychloroquine, azathioprine, methotrexate, mycophenolate, cyclophosphamide, low dose IL-
2, intravenous immunoglobulins, and belimumab.
Omalizumab is a monoclonal antibody that interacts with the binding site of the high-affinity IgE
receptor on mast cells. It is an engineered, humanized recombinant immunoglobulin. Moderate to
severe allergic bronchial asthma can improve with omalizumab.[13]
13. Justiz Vaillant, Angel A.; Vashisht, Rishik; Zito, Patrick M. (2021), "Immediate Hypersensitivity Reactions", StatPearls, Treasure Island
(FL): StatPearls Publishing, PMID 30020687, retrieved 2021-07-05 This article incorporates text available under the CC BY 4.0 license.](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-22-320.jpg)
![Delayed hypersensitivity reactions
Treatment of type 4 HR involves the treatment of the eliciting cause.
The most common drugs to treat tuberculosis include isoniazid, rifampin, ethambutol, and
pyrazinamide. For drug-resistant TB, a combination of antibiotics such as amikacin, kanamycin, or
capreomycin should be used.
The most common drugs to treat leprosy include rifampicin and clofazimine in combination with
dapsone for multibacillary leprosy. A single dose of antimicrobial combination to cure single lesion
paucibacillary leprosy comprises ofloxacin, rifampicin, and minocycline.
Praziquantel can be useful for treating infections caused by all Schistosoma species.
Hydroxychloroquine and chloroquine can use in the therapy of sarcoidosis involving the skin, lungs,
and the nervous system.
The use of anti-TNF monoclonal antibodies such as adalimumab and certolizumab have been
approved for Crohn disease.[14]
14. Justiz Vaillant, Angel A.; Zulfiqar, Hassam; Ramphul, Kamleshun (2021), "Delayed Hypersensitivity Reactions", StatPearls, Treasure
Island (FL): StatPearls Publishing, PMID 30085565, retrieved 2021-07-05 This article incorporates text available under the CC BY 4.0
license.
External links](https://image.slidesharecdn.com/delayedhypersensitivtypresentation-240416032845-fa2c8167/85/Delayed-Hypersensitivty-Presentation-pptx-23-320.jpg)

