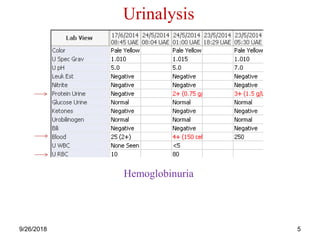
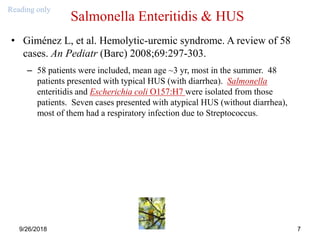
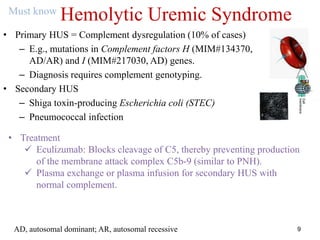
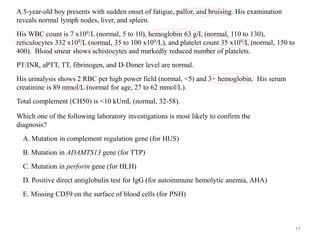
The document provides an overview of hemolytic uremic syndrome (HUS), detailing its classifications as atypical (primary, due to inherited complement dysregulation) and typical (secondary, often due to gastrointestinal pathogens like E. coli). It discusses clinical presentations, laboratory findings, and the role of eculizumab as a treatment for complement-mediated HUS. It also highlights the importance of complement genotyping and the differential diagnoses for related symptoms.
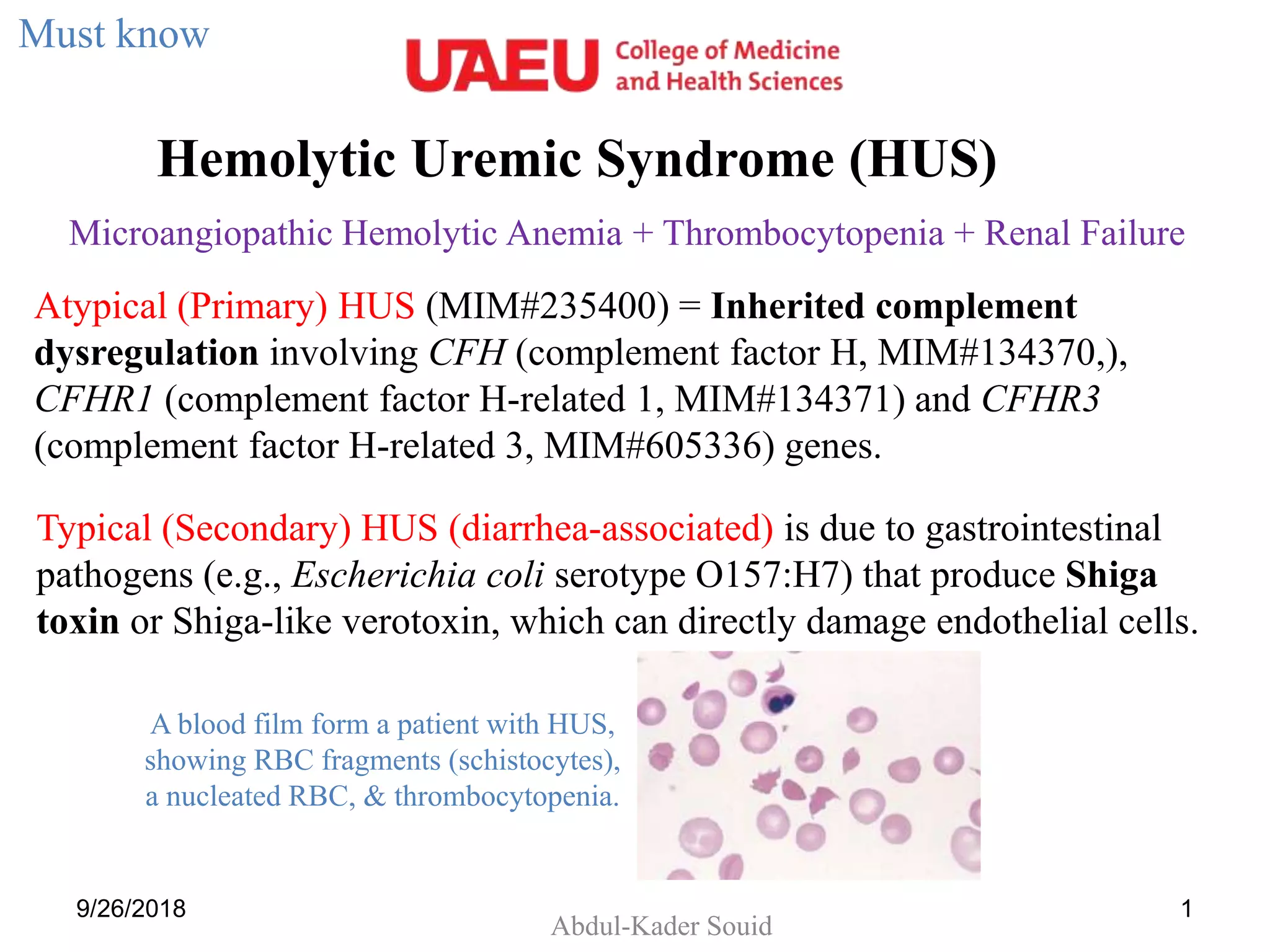
![Typical (Secondary) HUS (diarrhea-associated) is due to gastrointestinal pathogens
(e.g., Escherichia coli serotype O157:H7) that produce Shiga toxin or Shiga-like
verotoxin, which can directly damage endothelial cells.
9/26/2018 2
[Moake JL. Thrombotic
microangiopathies. N Engl J Med.
2002;347:589-600. PMID: 12192020]](https://image.slidesharecdn.com/11hus-180926043558/85/HUS-ppt-2-320.jpg)