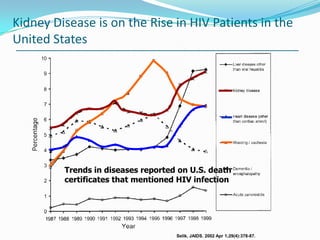
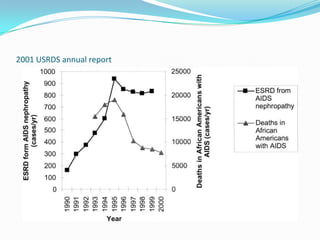
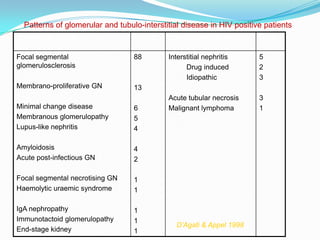
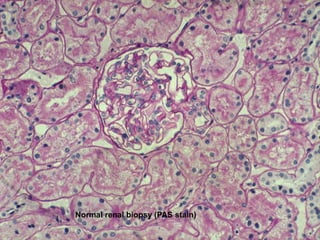
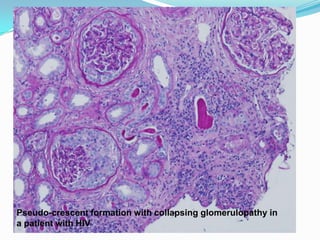
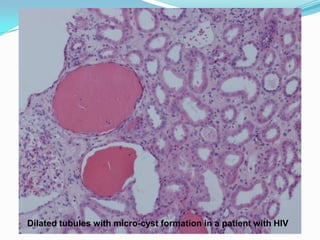
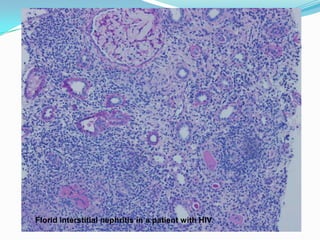
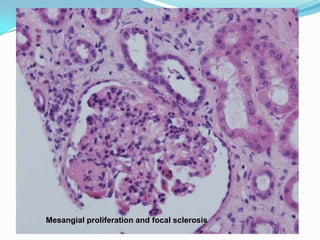
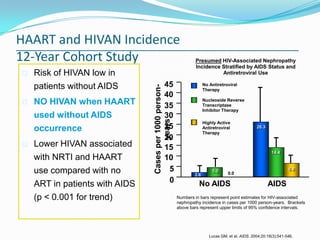
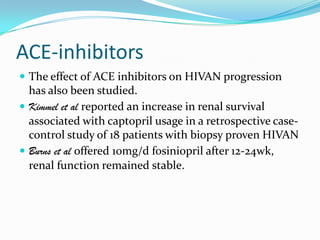
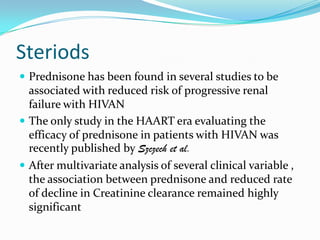
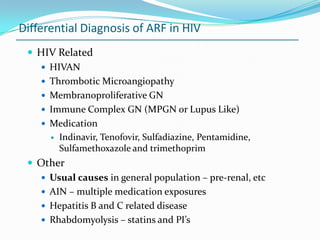
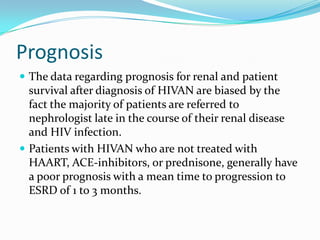
HIV-associated nephropathy (HIVAN) is a kidney disease characterized by proteinuria, kidney damage, and focal segmental glomerulosclerosis that primarily affects people with HIV. It was first reported in 1984 and is most common in African Americans. The introduction of antiretroviral therapy has decreased the incidence of end-stage renal disease due to HIVAN. HIV infection of renal epithelial cells directly contributes to HIVAN pathogenesis, and the kidneys may serve as an important viral reservoir even when viral loads are undetectable in blood. Treatment with antiretroviral therapy, ACE inhibitors, and steroids can help reduce progression of kidney disease in patients with HIVAN.