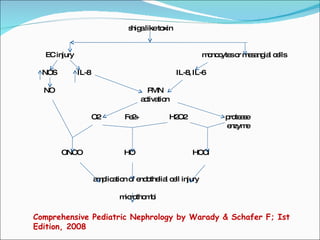
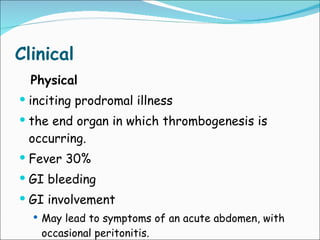
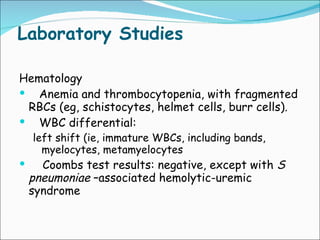
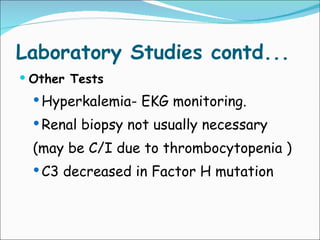
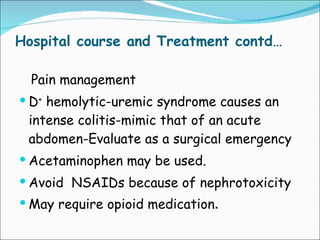
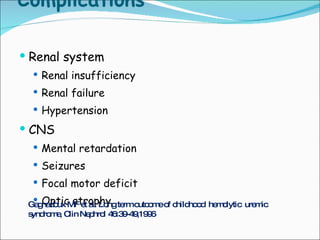
The document summarizes the pathophysiology, clinical presentation, diagnosis, and management of hemolytic uremic syndrome (HUS). It notes that HUS is most commonly caused by Shiga toxin-producing E. coli infection, with diarrhea as a common prodrome. The Shiga toxin damages endothelial cells leading to thrombocytopenia, hemolytic anemia, and renal impairment. Treatment involves supportive care, dialysis, and plasma exchange or infusion depending on the subtype.