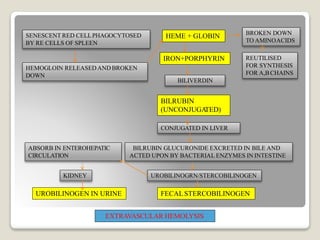
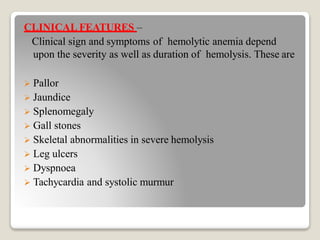
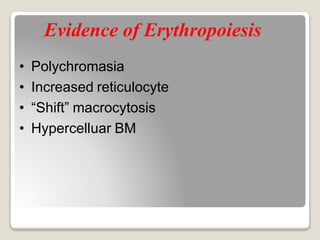
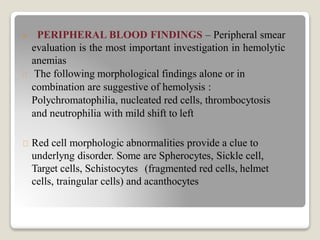
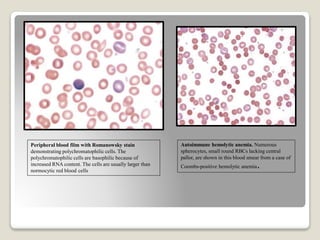
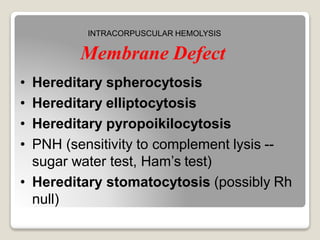
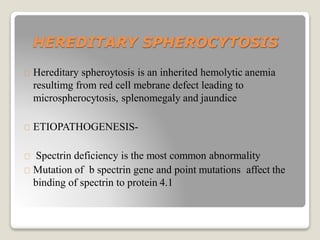
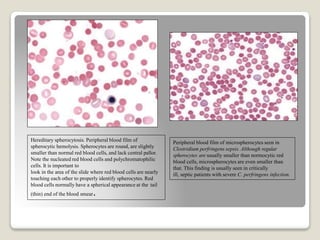
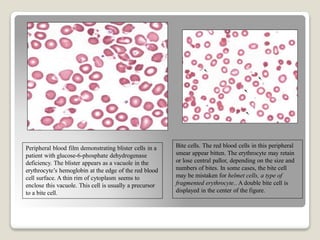
Hereditary spherocytosis is a hereditary hemolytic anemia caused by a red blood cell membrane defect that results in spherocytosis. The misshapen red blood cells, called spherocytes, are destroyed by the spleen, leading to hemolysis and a shortage of red blood cells. Clinical features include jaundice, splenomegaly, and gallstones. Laboratory findings show microspherocytes on peripheral blood film and increased reticulocytes, with normal red blood cell size.