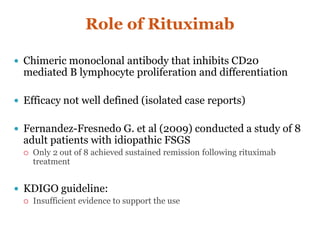
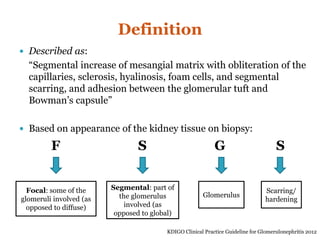
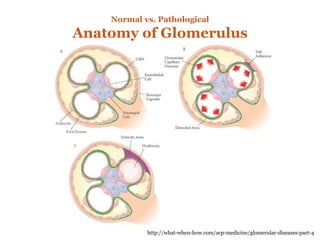
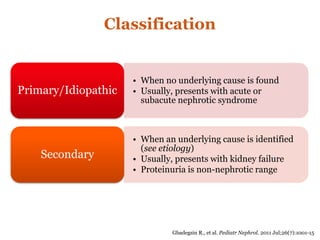
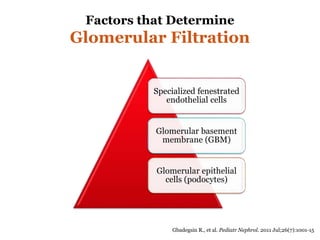
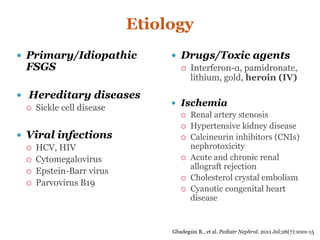
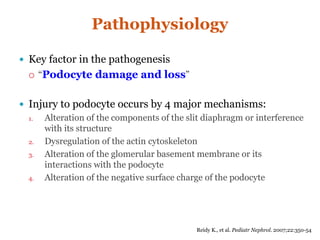
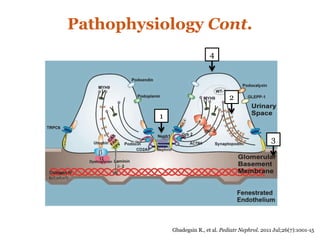
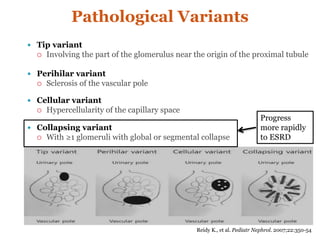
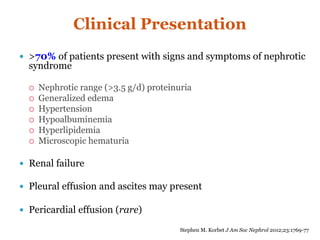
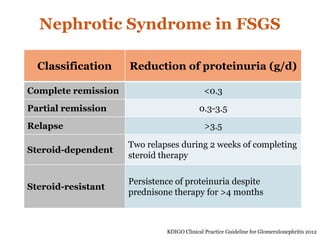
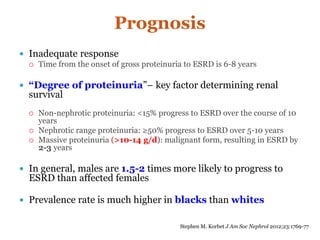
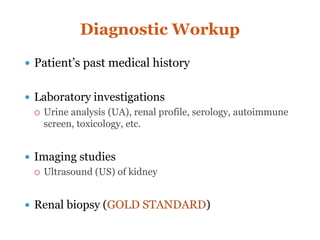
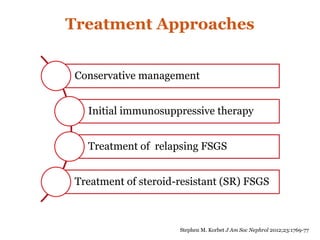
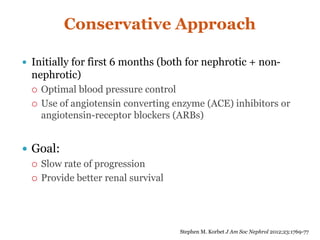
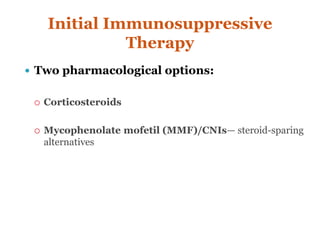
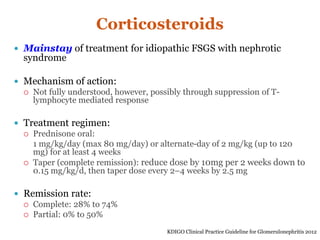
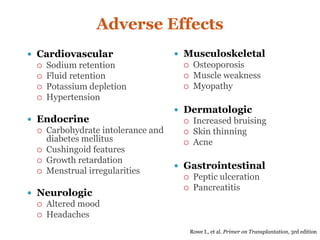
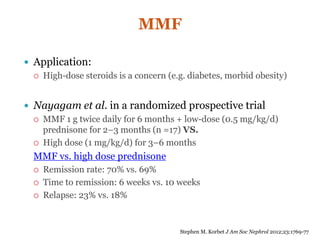
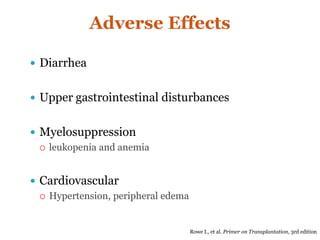
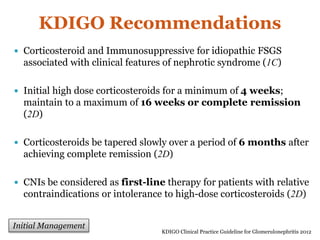
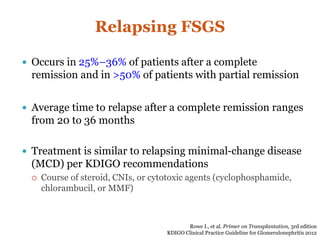
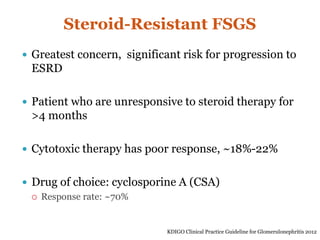
Focal segmental glomerulosclerosis (FSGS) is a kidney disease characterized by scarring in the glomeruli. It can be primary/idiopathic or secondary to other causes like viral infections, drugs, ischemia, etc. Patients often present with nephrotic syndrome. Treatment involves controlling blood pressure and proteinuria with ACE inhibitors/ARBs initially. For idiopathic FSGS with nephrotic syndrome, the first line treatment is corticosteroids. Mycophenolate mofetil or calcineurin inhibitors can be used as steroid-sparing alternatives. For steroid-resistant FSGS, calcineurin inhibitors like cyclosporine A are recommended.

![Steroid-Resistant FSGS Cont.
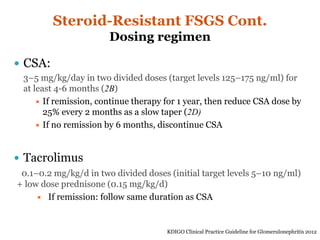
Cattran el at. conducted the largest randomized placebo-
controlled trial of 49 steroid resistant FSGS patients,
CSA group (n = 26): 3.5 mg/kg/d in two divided doses for 6 months
All received low dose corticosteroid (0.15 mg/kg/d)
Results:
Complete remission at 6 months: 69% (CSA group) vs. 12% (placebo)
Partial remission: 57% (CSA group) vs. <5% (placebo)
Average time to remission: 7 weeks [range: 1,25]
However, at 78 weeks 60% of CSA group relapsed
Meyrier et al. studied nephrotoxicity of CSA using renal
biopsy post 1 year of CSA therapy
Result: risk of nephrotoxicity was generally seen at 11-29 months and
dose >5.5 mg/kg/d posed greatest toxicity
Stephen M. Korbet J Am Soc Nephrol 2012;23:1769-77](https://image.slidesharecdn.com/a47bc6cd-76b1-482e-8a81-0a439d7b9114-160809054904/85/Focal-Segmental-Glomerulosclerosis-FSGS-33-320.jpg)