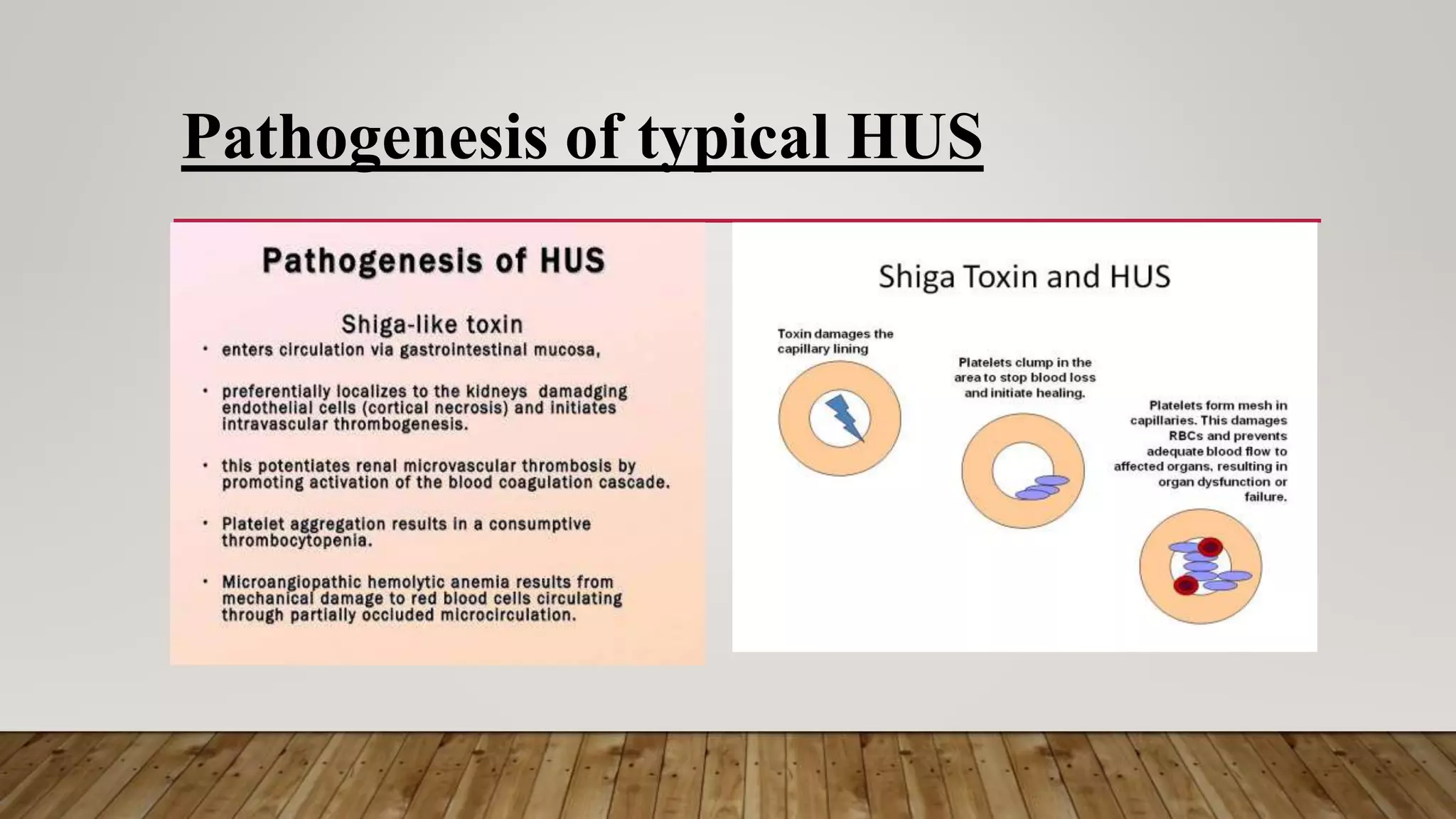
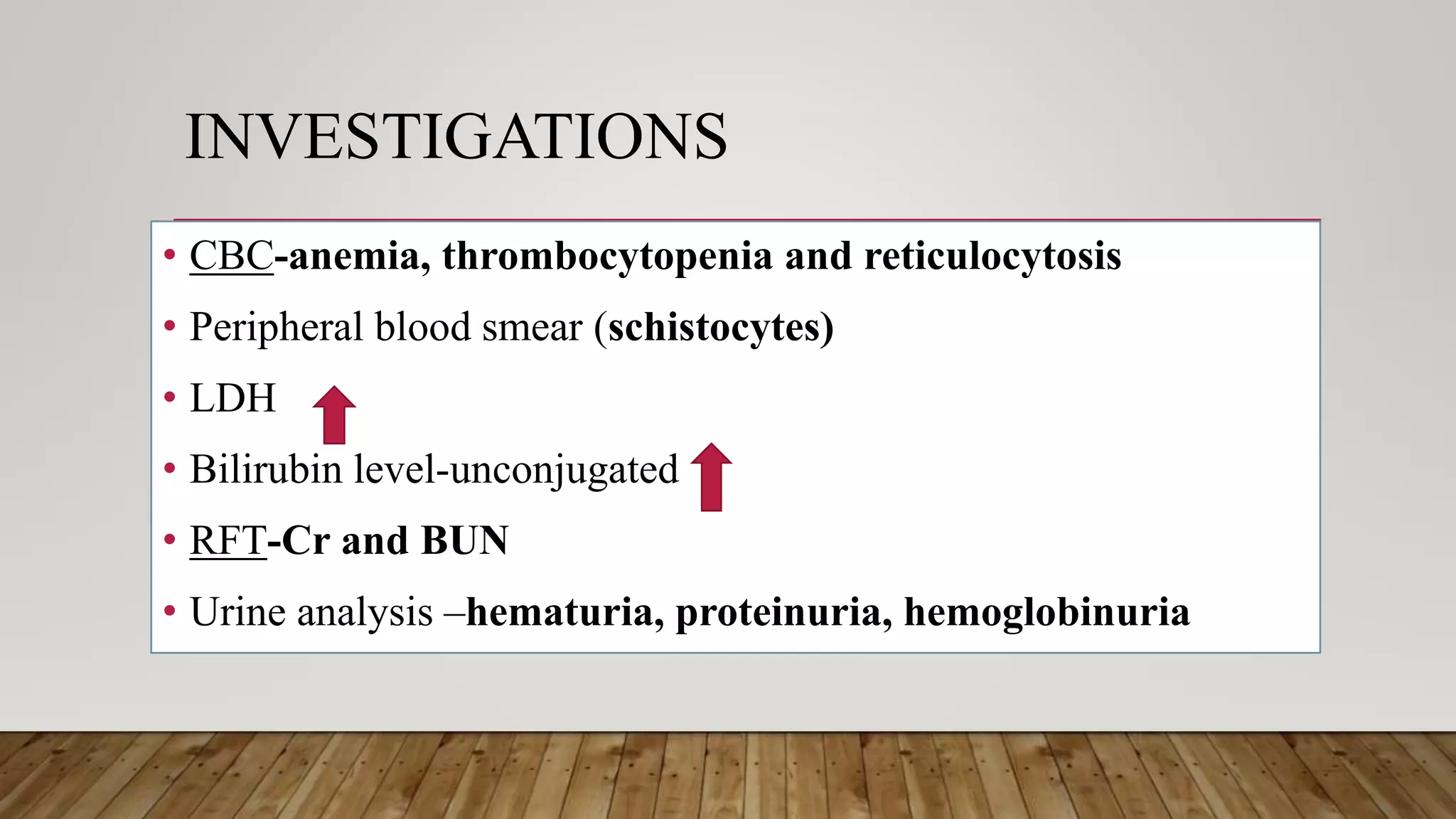
This document provides an overview of hemolytic uremic syndrome (HUS). It begins with background information, noting that HUS is characterized by hemolytic anemia, thrombocytopenia, and acute kidney injury. It is most common in children under 5. HUS is then classified as typical (diarrhea-associated) or atypical. The etiopathogenesis of typical HUS involves shiga toxin-producing bacteria like E. coli damaging endothelial cells. Clinically, HUS presents with anemia, oliguria, hematuria, and hypertension. Investigations show anemia, thrombocytopenia, and schistocytes on blood smear. Management involves supportive care, antibiotics, and plasma therapy. The
















![(b) Use of antibiotics
• Use of antimicrobial agent{contradicting)- no evidence of
benefit
• [c] Plasma infusion in severe cases
• Complement replacements](https://image.slidesharecdn.com/presentation-180729192137/75/hemolytic-uremic-syndrome-19-2048.jpg)


