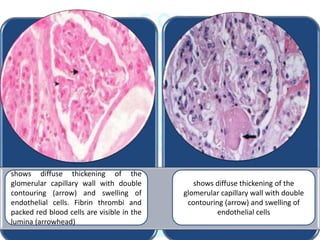
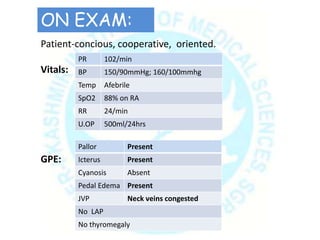
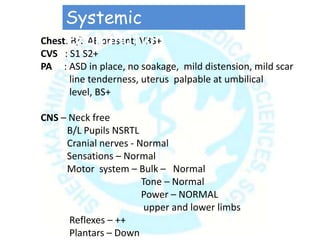
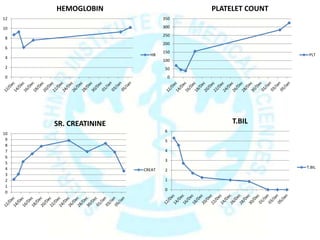
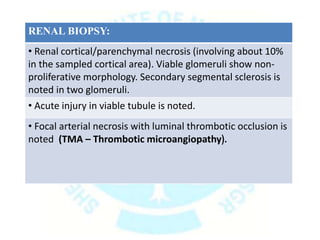
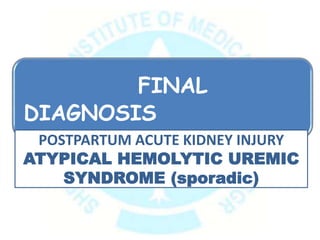
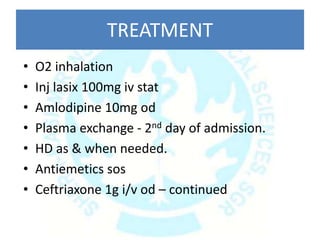
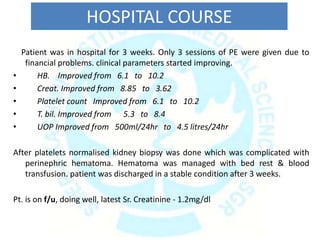
This case presentation describes a 27-year-old female who presented with decreased urine output, swelling of the face and feet, anorexia, and vomiting two days after a cesarean section. Laboratory investigations revealed thrombocytopenia, microangiopathic hemolytic anemia, and acute kidney injury. A renal biopsy showed features of thrombotic microangiopathy. She was diagnosed with postpartum atypical hemolytic uremic syndrome (aHUS). Treatment included plasma exchange, hemodialysis as needed, and supportive care. Her clinical parameters improved with treatment and she was discharged after three weeks.




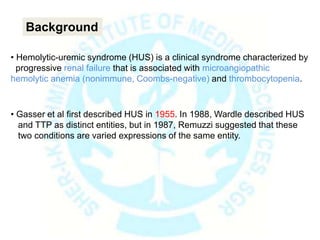
![ Damage to endothelial cells is the primary event in the pathogenesis of hemo-
lytic uremic syndrome (HUS).
The cardinal lesion is composed of arteriolar and capillary microthrombi
(thrombotic microangiopathy [TMA]) and red blood cell (RBC) fragmentation.
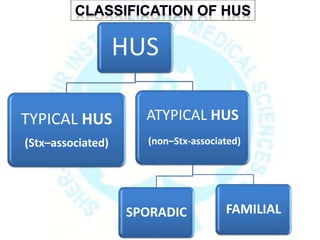
• HUS is classified into two main categories, depending on whether it is assoc-
ated with Shiga-like toxin (Stx) or not.
Pathophysiology](https://image.slidesharecdn.com/ahus05-180827190111/85/Atypical-Hemolytic-uremic-syndrome-18-320.jpg)
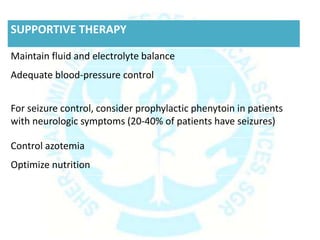
![• Nonenteric infections
• Viruses
• Drugs
• Malignancies
• Transplantation
• Pregnancy
• Antiphospholipid syndrome [APL]
• Systemic lupus erythematosus [SLE]
Triggers for SPORADIC Atypical HUS:](https://image.slidesharecdn.com/ahus05-180827190111/85/Atypical-Hemolytic-uremic-syndrome-24-320.jpg)