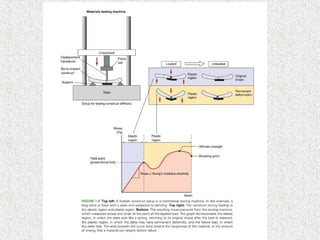
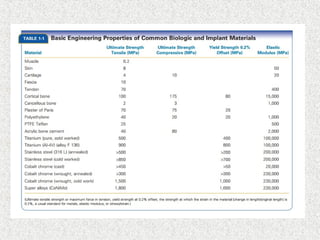
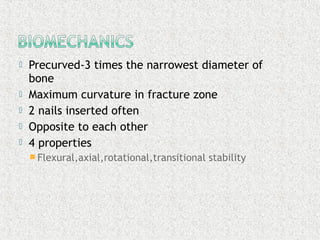
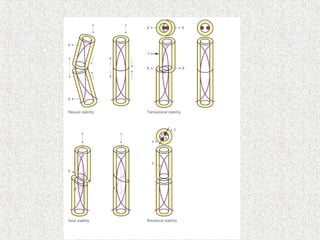
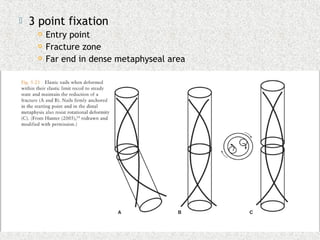
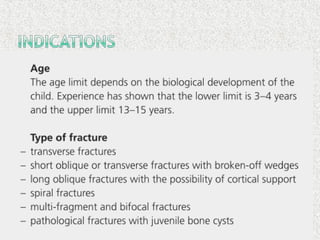
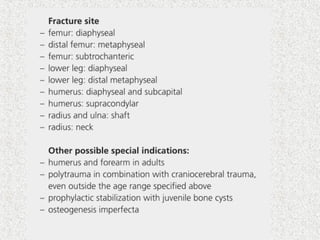
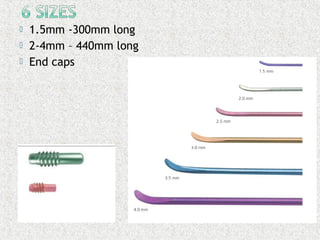
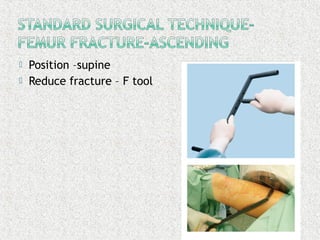
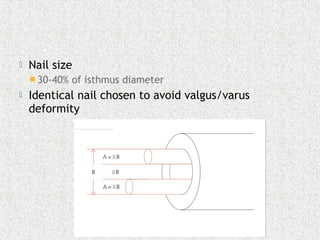
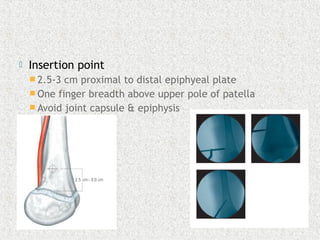
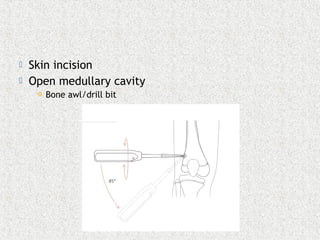
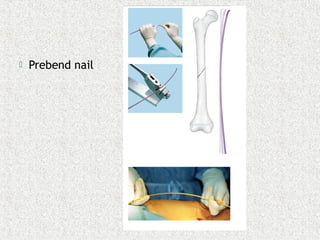
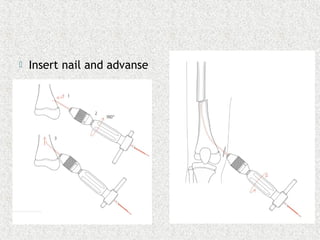
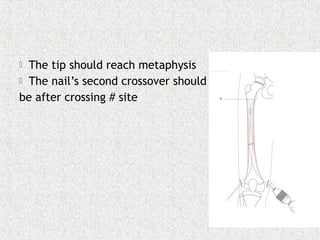
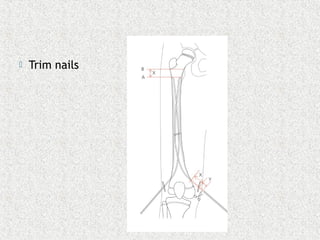
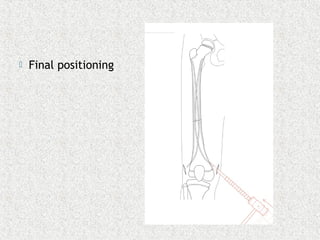
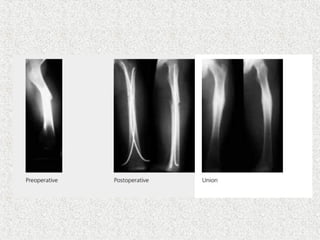
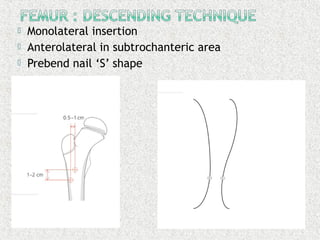
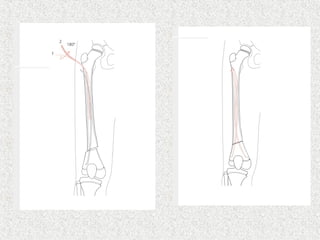
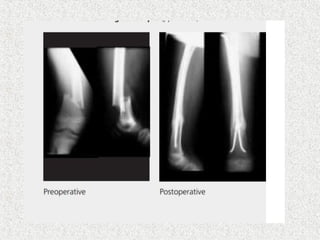
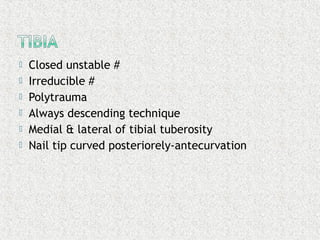
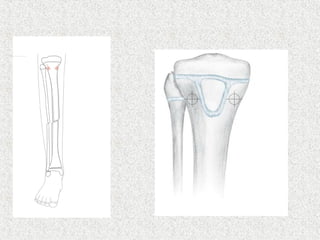
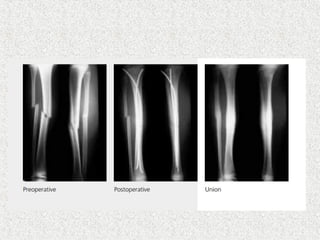
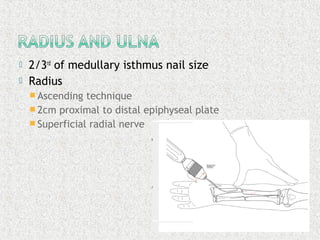
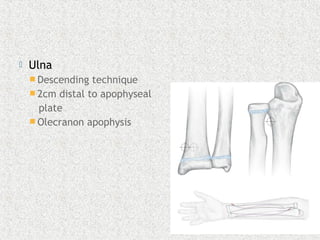
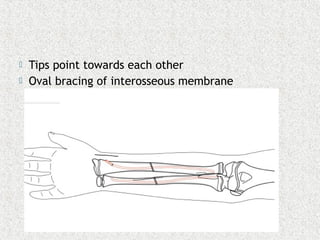
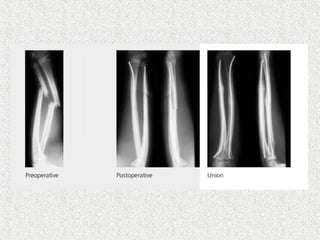
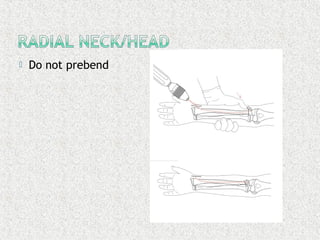
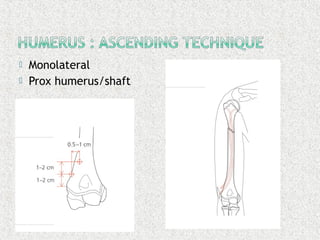
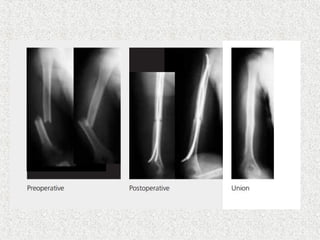
The document discusses the history and development of elastic stable intramedullary nailing (ESIN) for fractures in children. It describes early techniques using rigid pins and wires, and the development of the modern ESIN method in the 1980s using pre-bent titanium nails inserted from opposite sides of the bone for axial, lateral, and rotational stability. Key aspects of ESIN technique are outlined, including nail sizing, insertion points, pre-bending, and final positioning to stabilize fractures while minimizing soft tissue injury and allowing callus formation. Risks and special considerations for different bone fractures are also mentioned.