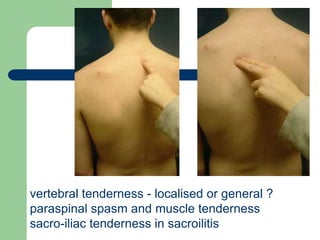
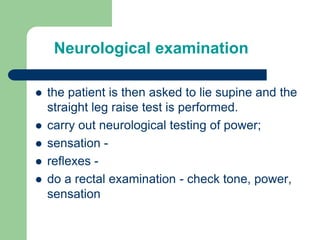
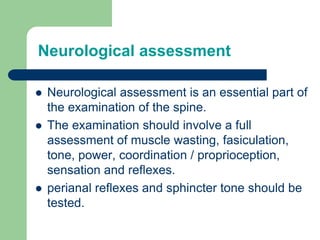
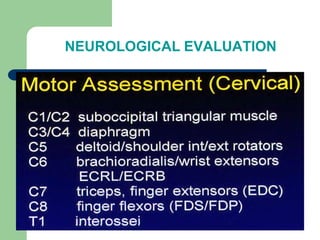
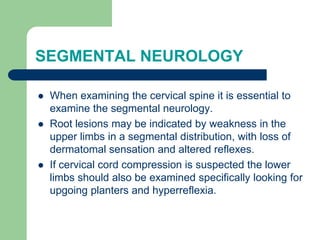
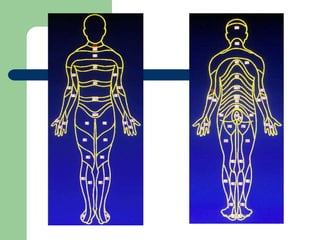
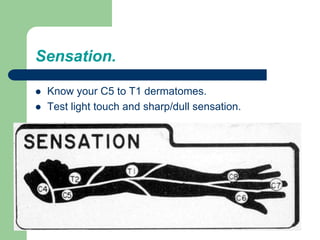
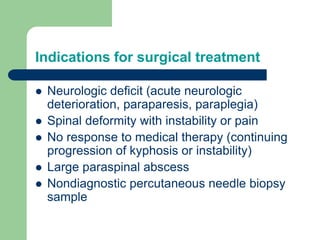
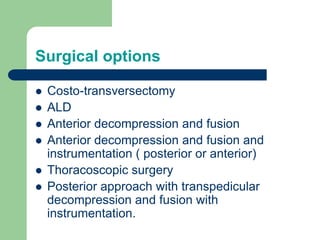
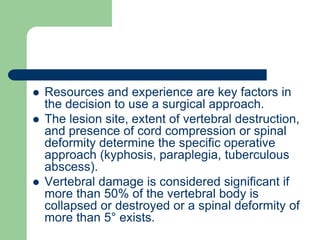
TB spine with neurological deficit can present with varying symptoms depending on the location and severity of involvement. On examination, patients may have spinal tenderness and deformity as well as neurological deficits. Investigations like ESR, Mantoux test, imaging and microbiology can help confirm the diagnosis of TB spine. Treatment involves anti-tubercular medications alongside surgical intervention if needed to address neurological deficits, deformity or abscesses.